Abstract
During atherogenesis, excess amounts of low-density lipoproteins (LDL) accumulate in the subendothelial space where they undergo oxidative modifications. Oxidized LDL (oxLDL) alter the fragile balance between survival and death of vascular smooth muscle cells (VSMC) thereby leading to plaque instability and finally to atherothrombotic events. As protein kinase C δ (PKCδ) is pro-apoptotic in many cell types, we investigated its potential role in the regulation of VSMC apoptosis induced by oxLDL. We found that human VSMC silenced for PKCδ exhibited a protection towards oxLDL-induced apoptosis. OxLDL triggered the activation of PKCδ as shown by its phosphorylation and nuclear translocation. PKCδ activation was dependent on the reactive oxygen species generated by oxLDL. Moreover, we demonstrated that PKCδ participates in oxLDL-induced endoplasmic reticulum (ER) stress-dependent apoptotic signaling mainly through the IRE1α/JNK pathway. Finally, the role of PKCδ in the development of atherosclerosis was supported by immunohistological analyses showing the colocalization of activated PKCδ with ER stress and lipid peroxidation markers in human atherosclerotic lesions. These findings highlight a role for PKCδ as a key regulator of oxLDL-induced ER stress-mediated apoptosis in VSMC, which may contribute to atherosclerotic plaque instability and rupture.
Similar content being viewed by others
Main
Atherosclerosis is a slow degenerative process and is the underlying cause of heart attacks, strokes, and peripheral artery diseases in humans. This complex disorder is characterized by the focal accumulation of lipids and the remodeling of the arterial wall, leading to the formation of the atherosclerotic plaque. Modified lipoproteins, specially oxidized low-density lipoproteins (oxLDL), are present within atheroma plaques, and are thought to play a role in atherogenesis.1 OxLDL exhibit a variety of atherogenic properties, by inducing foam cell formation, inflammatory response, cell proliferation, at low concentration, and apoptosis at higher concentration.2, 3 The balance between aberrant proliferation and apoptosis is responsible for mediating intense changes in the development of atherosclerosis. Apoptosis of vascular smooth muscle cells (VSMC) increases as atherosclerotic plaques develop and is sufficient to induce features of plaque vulnerability in atherosclerosis.4 Overall, loss of VSMC is detrimental for plaque stability and increases the risk of thrombotic events.
The apoptotic signaling triggered by oxLDL is mediated through a complex sequence of signaling events that lead to activation of caspase-dependent or caspase-independent apoptotic pathways. We previously reported that treatment of human VSMC with oxLDL induced a sustained rise of cytosolic calcium, leading to the activation of the intrinsic mitochondrial apoptotic pathway.5, 6 More recently, we showed in human vascular endothelial cells an interaction between the deregulation of cytosolic calcium and the endoplasmic reticulum (ER) stress in triggering the apoptotic response induced by oxLDL.7 ER plays an essential role in sensing cellular stress (i.e., accumulation of misfolded proteins, potential redox or calcium deregulation) as it rapidly detects changes in cell homeostasis, and responds by eliciting UPR (unfolded protein response) via the activation of ER transmembrane sensors, PERK (double-stranded RNA-dependent protein kinase (PKR)-like ER kinase), IRE1α (inositol-requiring 1α) and ATF6 (activating transcription factor 6). The UPR results in a temporary downregulation of protein translation, an upregulation of ER chaperones and folding machinery, and the expression and activation of ER-associated degradation (ERAD).8 Prolonged ER stress switches towards apoptotic cell death via the activation of downstream signals like CHOP (C/EBP homologous protein), JNK and members of the Bcl-2 family.9, 10 Our previous data11 and those from Myoishi et al.12 demonstrated that ER stress markers are present in human advanced atherosclerotic lesions thus raising the question of the possible role of ER stress in the stability/instability of atherosclerotic plaques, since this adaptive response may influence the fate of cells to survive or die.
Protein kinase C δ (PKCδ), a member of the PKC family of serine–threonine kinases, is known to be a critical pro-apoptotic signal in many cell types.13 More particularly, PKCδ-deficient mice develop exacerbated intimal hyperplasia associated with diminished SMC apoptosis in vein grafts14 and carotid ligation models,15 indicating that PKCδ is an important regulator of SMC apoptosis after vascular injury. Recently, it has been shown that PKCδ plays a crucial role in the propagation of TNFα-induced ER stress-mediated JNK activation and CHOP/GADD53 induction.16 Hitherto, whether PKCδ contributes to oxLDL-induced vascular SMC apoptosis and ER stress is not known.
Here, we investigated the possible involvement of PKCδ in the apoptotic signaling pathway triggered by oxLDL and its role in the transmission of the pro-apoptotic signal of the ER stress in human VSMC. We found that oxLDL mediate PKCδ activation through reactive oxygen species (ROS) production and that PKCδ plays a crucial role in the regulation of oxLDL-induced apoptosis mainly through the IRE1α/JNK pathway of ER stress. Importantly, we provided evidence that activated PKCδ is colocalized with ER stress and lipid peroxidation markers in human atherosclerotic lesions.
Results
SiRNA-mediated suppression of PKCδ expression reduces oxLDL-induced human vascular smooth muscle apoptosis
We first investigated the involvement of PKCδ in the apoptosis of human vascular smooth muscle (hVSMC) cells treated with oxLDL. The expression of PKCδ was silenced by small interfering RNA (siRNA) specific to human PKCδAs shown in Figure 1a. The inhibitory effect of siRNA on PKCδ expression was obvious 48 h after transfection and was not influenced by treatment with oxLDL. To assess whether the effect of PKCδ knockdown relates to hVSMC survival, PKCδ knockdown ()()and control cells were treated with oxLDL for 24 h. PKCδ knockdown cells displayed a protection towards oxLDL-induced apoptosis as demonstrated by a significant decrease in cell death (Figure 1b). The involvement of caspase-3 is supported by the protective effect of the multicaspase inhibitor z-VAD-fmk against oxLDL-induced apoposis (Figure 1c). We also showed the release of cytochrome C from the mitochondria, which is accompanied by an increased expression of the pro-apoptotic protein Bak and a decreased expression of the pro-survival protein Bcl-2 in agreement with the data of Yang et al.17 (Supplementary Figure S1). The activation of caspase-3 is prevented in PKCδ knockdown cells as shown by the inhibition of its cleavage, compared with control cells (Figure 1d).
SiRNA silencing of PKCδ reduced oxLDL-induced apoptosis of human VSMC. (a) Representative western blot of the expression of PKCδ after siRNA silencing. Human VSMC were transfected with 100 nM scrambled siRNA or 100 nM PKCδ siRNA for 48 h as described under ‘Materials and Methods.’ After siRNA transfection, hVSMC were treated with oxLDL (200 μg ApoB/ml) at the indicated times. Immunoblots were performed on cell lysates using an anti-PKCδ antibody and β-actin was used as a loading control. (b) Analysis of oxLDL-induced cell death. Human VSMC transfected with scrambled (scr) or PKCδ siRNA were incubated with oxLDL (200 μg ApoB/ml) for 24 h and apoptotic cells were counted after staining with SYTO-13/PI as described under ‘Materials and Methods.’ The left graph represents the results expressed as percentage of untreated control and the mean±S.E.M. of four independent experiments (>200 cells were counted for each variable per experiment). **P<0.01 indicates significance (comparison between apoptotic cells from scr siRNA transfected cells+oxLDL and PKCδ siRNA transfected cells+oxLDL groups. The left panel illustrates the SYTO-13/IP labeling of human VSMC treated or not with oxLDL (200 μg ApoB/ml, for 24 h). (c, d) Involvement of caspase-3 in oxLDL-induced apoptosis. (c) Human VSMC pretreated with z-VAD-fmk (50 μM) were incubated with oxLDL (200 μg ApoB/ml) for 24 h and apoptotic cells were counted after staining with SYTO-13/PI as described under ‘Materials and Methods.’ The graph represents the results expressed as percentage of untreated control and the mean±S.E.M. of four independent experiments (>200 cells were counted for each variable per experiment). **P<0.01 indicates significance (comparison between apoptotic cells from oxLDL-treated and z-VAD+oxLDL-treated groups). (d) Representative western blot of time-course analysis of procaspase-3 processing and cleaved caspase-3 generation in human VSMC transfected with scrambled or PKCδ siRNA and treated with oxLDL (200 μg ApoB/ml, 16 h). Immunoblots representative of three independent experiments, were performed on cell lysates using anti-procaspase-3, anti-cleaved caspase-3 antibodies and β-actin was used as a loading control
We further demonstrated the involvement of PKCδ in the apoptosis induced by oxLDL by the use of mouse embryonic fibroblasts (MEF) invalided for PKCδ MEF PKCδ−/−) that showed a strong resistance to oxLDL-induced cell death as explored by cell viability assay, apoptotic characteristics, Bcl-2 expression, cytochrome C release and caspase-3 cleavage compared with MEF PKCδ cells (Figures 2a–e). Moreover, the central role of PKCδ in the broad regulation()of apoptosis is supported by the protection of MEF PKCδ−/−cells towards the apoptotic inducer antimycin A (Figure 2a).
MEF PKCδ−/− are protected from oxLDL-induced apoptosis. (a) Analysis of cell toxicity in MEF PKCδ−/− and MEF wild-type (named PKCδ+/+) was evaluated by the MTT assay. MEF PKCδ and MEF PKCδ+/+ were treated with oxLDLs (50–200 μg ApoB/ml), native LDL (nLDL, 100 μg ApoB/ml) or antimycin A (10 μM) for 24 h and cell toxicity was analyzed as described. Results are expressed as percentage of untreated control and represent the mean±S.E.M. of five separate experiments. **P<0.01 and *P<0.05 indicate significance (comparison were made between PKCδ−/− and PKCδ +/+ treated with 100 and 200 oxLDL μg ApoB/ml or 10 μM antimycin A), ns indicates no significance. (b) SYTO-13/PI staining of MEF PKCδ−/− and MEF PKCδ+/+ treated or not with oxLDL (200 μg ApoB/ml, for 24 h), the images illustrate the resistance of MEF PKCδ−/− towards oxLDL-induced apoptosis. (c) Time-course analysis of Bcl-2 expression in MEF PKCδ−/− and MEF PKCδ+/+ treated with oxLDL (200 μg ApoB/ml). Immunoblots representative of three independent experiments were performed on cell lysates using anti-Bcl-2 antibody and β-actin was used as a loading control. (d) Immunocytochemistry experiments showing the release of the cytochrome C monitored by immunofluorescence in MEF PKCδ−/− and MEF PKCδ+/+ treated with oxLDL (200 μg apoB/ml) 16 h. Cells were fixed and labeled with anti-cytochrome C antibody. The results are representative of three separate experiments. (e) Representative western blot of time-course analysis of procaspase-3 processing and cleaved caspase-3 generation in MEF PKCδ−/− and MEF PKCδ+/+ treated with oxLDL (200 μg ApoB/ml, 16 h). Immunoblots representative of three independent experiments were performed on cell lysates using anti-procaspase-3, anti-cleaved caspase-3 antibodies and β-actin was used as a loading control
The resistance to apoptosis in PKCδ−/− cells likely results from the loss of PKCδ expression, to prove that apoptosis is directly dependent on PKCδ we asked if the re-expression of PKCδ is sufficient to restore the apoptotic response induced by oxLDL.
MEF PKCδ−/− cells were transduced with adenovirus expressing either GFP (AdGFP) or a PKCδ–GFP (AdPKCδ–GFP) fusion protein (Figure 3a). As shown in Figure 3b, transduction of AdPKCδ–GFP completely re-establishes their apoptotic response to oxLDL, whereas PKCδ−/− cells transduced with AdGFP remained resistant to oxLDL-induced apoptosis. Our data clearly demonstrate that re-expression of PKCδ in PKCδ−/− cells reconstitute apoptotic potential. Altogether, our results indicate that PKCδ plays a major role in the apoptosis induced by oxLDL.
Re-expression of PKCδ–GFP in MEF PKCδ−/− cells reconstitutes apoptotic potential. (a) Western blot analysis of re-expression of PKCδ in MEF PKCδ−/− compared with MEF PKCδ+/+. MEF PKCδ−/− were infected with adenovirus GFP (AdGFP) or a PKCδ–GFP (AdPKCδ–GFP) fusion protein for 24 h. Immunoblots were performed on cell lysates using anti-PKCδ and β-actin was used as a loading control. (b) Analysis of cell toxicity in MEF PKCδ−/− expressing AdPKCδ–GFP or AdGFP fusion protein was evaluated by the MTT assay. MEF PKCδ−/− infected with adenovirus GFP (AdGFP) or a PKCδ–GFP (AdPKCδ–GFP) fusion protein for 24 h. Cells were treated or not with oxLDLs (200 μg ApoB/ml) for 24 h and cell toxicity (left panel) was analyzed as described. Results are expressed as percentage of untreated control and represent the mean±S.E.M. of four separate experiments. **P<0.01 indicate significance (comparison were made between PKCδ−/−+AdGFP and PKCδ−/−+AdPKCδ–GFP treated with oxLDL). SYTO-13/PI labeling (right panel) of PKCδ−/−+AdGFP and PKCδ−/−+AdPKCδ–GFP) treated with oxLDL (200 μg ApoB/ml, for 24 h), the images illustrate the restoration of the apoptotic potential of MEF PKCδ−/− expressing AdPKCδ–GFP. Cells treated with oxLDL showed chromatin condensation and appearance of apoptotic bodies, because of the brightness of SYTO-13, GFP fluorescence is not apparent
PKCδ is activated in response to oxLDL stimulation in human vascular smooth muscle
The ability of PKCδ to activate an apoptotic program is regulated by key events such as phosphorylation on specific tyrosine residues and nuclear accumulation where it may be cleaved by caspase to generate a pro-apoptotic PKCδ catalytic fragment (δCF).13 We analyzed the phosphorylation of PKCδ on tyrosine 311 because (i) this critical residue located in the catalytic domain is phosphorylated in response to apoptotic stimulus such as oxidative stress induced by hydrogen peroxide18, 19 and because (ii) oxLDL treatment generates an oxidative stress through the production of hydrogen peroxide (H2O2) and superoxide anion (O2−).20 To examine the effect of oxLDL on PKCδ tyrosine 311 phosphorylation, hVSMC were treated with increasing concentrations of oxLDL (0–200 μg ApoB/ml) for 5 h or with cytotoxic concentration of oxLDL (200 μg ApoB/ml) for 1–8 h. As shown in Figure 4a, the phosphorylation level of tyrosine 311 increases with the concentration of oxLDL and with the length of time treatment being visible at 5 h stimulation. We then followed the nuclear translocation of PKCδ by two methods: cell fractionation and fluorescence microscopy. After hVSMC treatment with oxLDL, the nuclear and cytosolic fractions were separated by differential centrifugation. We found that in untreated cells, PKCδ was expressed in the cytosol and translocated to the nucleus beyond 12 h of oxLDL stimulation (Figure 4b). Using immunofluorescence microscopy, we confirmed that PKCδ was located mostly in the cytosol in untreated control cells and that oxLDL induced the translocation of PKCδ to the nucleus in about 90–95% of the cells as observed following 18 h treatment with oxLDL (Figure 4c). Collectively, these data show that oxLDL induce the activation of PKCδ to trigger hVSMC apoptosis.
OxLDL induce PKCδ activation through tyrosine 311 phosphorylation and nuclear translocation in human VSMC. (a) Time-course analysis of PKCδ phosphorylation in human VSMC treated with oxLDL (200 μg ApoB/ml). Western blot experiments were performed on total protein extracts using anti-phosphotyrosine 311 PKCδ antibody and β-actin expression was used as loading control. The graph represents values of phosphotyrosine 311 PKCδ band intensity after normalization for total PKCδ by densitometry, *P<0.05 and **P<0.01 indicate significance (comparison between untreated cells and oxLDL 5 h and between untreated cells and oxLDL 8 h), ns indicates no significance. Blots are representative of four independent experiments. (b) Time-course analysis showing nuclear translocation of PKCδ in human VSMC treated with oxLDL (200 μg ApoB/ml). Immunoblots were performed on cell lysates and analyzed for the presence of PKCδ after nuclear and cytosolic fractionation as described under ‘Materials and Methods.’ TBP (TATA-binding protein, nuclear marker) and β-actin (cytosolic marker) were also used as a loading control. Blots are representative of three independent experiments. (c) Immunocytochemistry experiments showing the nuclear translocation of PKCδ monitored by immunofluorescence in human VSMC treated with oxLDL (200 μg ApoB/ml) for 12 or 18 h. Cells were fixed and labeled with anti-PKCδ antibody. The results are representative of three separate experiments
ROS generated by oxLDL contribute to the activation of PKCδ
We then questioned the mechanisms involved in oxLDL-induced PKCδ activation. We previously showed that oxLDL trigger an intracellular rise in ROS in rabbit smooth muscle cells.21 Therefore, we investigated whether oxLDL-induced ROS generation is involved in PKCδ tyrosine 311 phosphorylation. Incubation of hVSMC with oxLDL but not with nLDL (data not shown) resulted in a rapid increase of intracellular ROS as assessed by the rise of DCF fluorescence (Figure 5a). OxLDL-mediated ROS production is prevented by preincubation with the NADPH oxidase inhibitor 3-benzyl-7-(2-benzoxazolyl)thio-1,2,3-triazolo[4,5-d]pyrimidine (VAS2870, 10 μM) and with the addition of a cell permeable form of the antioxidant enzyme catalase (PEG-catalase 50 UI/ml). Indeed, addition of PEG-conjugated enzyme produces an increase in plasma membrane fluidity, thus enhancing cell association and uptake.22 These data suggest that NADPH oxidases play a major role in the generation of ROS by oxLDL and that H2O2 produced through the dismutation of O2− might be the mediator of ROS-induced cell signaling. We further analyzed the inhibitory efficiency of VAS2870 and PEG-catalase on the tyrosine 311 phosphorylation of PKCδ. As shown in Figure 5b, both antioxidants were able to prevent oxLDL-induced PKCδ phosphorylation in hVSMC. These findings demonstrate that oxLDL generate intracellular ROS responsible for PKCδ activation. Moreover, the inhibitory effect of VAS2870 suggests that ROS production depends on the activity of NADPH oxidase in hVSMC.
ROS generation mediated by oxLDL is involved in the activation of PKCδ. (a) Measurement of intracellular ROS production using the free radical sensor: H2DCFDA (6-carboxy-2′,7′-dichlorodihydrofluorescein diacetate). Human VSMC were pretreated with the NADPH inhibitor (VAS-2870, 10 μM) or with PEG-catalase (50 UI/ml) for 1 h, then incubated with oxLDL (200 μg apoB/mL) for 0.5, 1 and 5 h. The variation of intracellular ROS was detected by fluorescence intensity using using the free radical sensor: 6-carboxy-2′,7′-dichlorodihydrofluorescein diacetate as described under ‘Materials and Methods.’ Results were normalized on protein levels and expressed in ratio to untreated control. The data are expressed as mean±S.E.M. of five separate experiments *or #P<0.05; **or ##P<0.01 indicate significance, (# comparison between untreated cells and oxLDL-treated cells, *comparison between oxLDL-treated cells and oxLDL+VAS2870, between oxLDL-treated cells and oxLDL+catalase). ns indicates no significance. (b) Analysis of oxLDL-induced PKCδ phosphorylation in human VSMC pretreated with NADPH inhibitor (VAS-2870, 10 μM) or with PEG-catalase (50 UI/ml). Western blot experiments were performed on total protein extracts treated with oxLDL (200 μg ApoB/ml) for 8 h, using anti-phosphotyrosine 311 PKCδ antibody and total PKCδ expression was used as loading control. The graph represents values of phosphotyrosine 311 PKCδ band intensity after normalization for total PKCδ by densitometry, **P<0.01 indicates significance (comparison between oxLDL and oxLDL+VAS2870, between oxLDL and oxLDL+catalase). Blots are representative of three independent experiments
The UPR is induced upon oxLDL stimulation and the activation of the ER stress-dependent IRE1/JNK pathway is dependent on PKCδ expression
It has been recently shown that PKCδ participates in ER stress-induced apoptosis in mouse neuroblastoma cells.23 To determine whether UPR is induced in hVSMC following oxLDL treatment, we investigated the activation of the three classical ER sensors: PERK, IRE1α and ATF6. Our data showed the phosphorylation of the PERK substrate eIF2α an increase expression of IRE1α24 and the nuclear translocation of ATF6 upon oxLDL stimulation in hVSMC (Figures 6a and b). Because oxLDL trigger a prolonged ER stress activation, which may have a role in apoptotic cell death through IRE1α-TRAF2-JNK pathway and CHOP expression, we checked the activation of these proapoptotic pathways in hVSMC. OxLDL elicited the activation of JNK and the expression of CHOP protein (Figure 6c), which is in agreement with our previous studies showing the contribution of these two ER stress proapoptotic mediators in oxLDL-induced human endothelial cell apoptosis.7 We provided further evidence for the role of the ER stress induced by oxLDL in the apoptosis of hVSMC by showing the induction of PUMA (p53 upregulated modulator of apoptosis) and BIM (BCL-2 interacting mediator of cell death), two pro-apoptotic BH3 domain-only proteins regulated by CHOP in response to ER stress (Figure 6d).
OxLDL trigger UPR and pro-apoptotic ER stress pathways in human VSMC. Time course of ER stress sensors activation in human VSMC treated with oxLDL (200 μg ApoB/ml). (a) Western blot experiments were performed on total protein extracts, cell lysates were assessed for phospho-eIF2α and IRE1α expression. β-Actin was used as protein loading control. Blots are representative of three independent experiments. (b) Immunocytochemistry experiments show the cytoplasmic and nuclear translocation of ATF6 in human VSMC treated with oxLDL (200 μg ApoB/ml) for 16 h. These data are representative of three separate experiments. (c, d) Time course of the ER stress pro-apoptotic mediators activation in human VSMC treated with oxLDL (200 μg ApoB/ml). Western blot experiments were performed on total protein extracts, cell lysates were assessed for phospho-JNK, CHOP, BIM and PUMA expression. β-Actin was used as protein loading control. Blots are representative of three independent experiments
We next explored whether PKCδ plays a role in oxLDL-induced ER stress signaling. We observed the phosphorylation of the PERK substrate eIF2α and the nuclear translocation of ATF6 in MEF PKCδ+/+ and PKCδ−/− cells following oxLDL treatment (Figures 7a and b). On the other side, in PKCδ+/+ cells oxLDL induced the expression of IRE1α and CHOP, and JNK activation whereas PKCδ−/− cells treated with oxLDL displayed neither increased expression of IRE1α nor JNK activation but showed an increased expression of CHOP (Figures 7a and c).
PKCδ is involved in the activation of the pro-apoptotic ER stress IRE1/JNK pathway but not in CHOP activation. Time course of ER stress sensors activation in MEF PKCδ −/− and MEF PKCδ+/+ treated with oxLDL (200 μg ApoB/ml). (a) Western blot experiments were performed on total protein extracts, cell lysates were assessed for phospho-eIF2α and IRE1α expression. β-Actin was used as protein loading control. Blots are representative of three independent experiments. (b) Immunocytochemistry experiments show the cytoplasmic and nuclear translocation of ATF6 in MEF PKCδ−/− and MEF PKCδ+/+ treated with oxLDL (200 μg ApoB/ml) for 16 h. These data are representative of three separate experiments. (c) Time course of the ER stress proapoptotic mediators activation in MEF PKCδ−/− and MEF PKCδ+/+ treated with oxLDL (200 μg ApoB/ml). Western blot experiments were performed on total protein extracts, cell lysates were assessed for phospho-JNK and CHOP expression. β-Actin was used as protein loading control. Blots are representative of three independent experiments
We then asked whether PKCδ was necessary for the induction of the UPR. MEF PKCδ+/+ and PKCδ cells were stimulated by thapsigargin a potent inducer of ER stress. The activation of the UPR and the ER stress proapoptotic mediators was observed in cells expressing or not PKCδ (Supplementary Figure S2), indicating that PKCδ does not globally regulate the ER stress.
Therefore, our results demonstrated for the first time that PKCδ participates in oxLDL-induced ER stress-dependent apoptotic signaling mainly through the IRE1/JNK pathway.
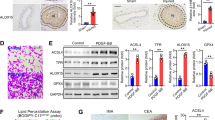
Activated PKCδ colocalized with ER stress and oxidative markers in human atherosclerotic lesions
Since oxLDL and oxidized lipids are found in atherosclerotic lesions, we investigated whether PKCδ phosphorylated on tyrosine 311 is expressed in human atherosclerotic lesions of carotid endarterectomy. Immunostaining of phosphorylated PKCδ was strongly positive in the necrotic core of advanced atherosclerotic lesions compared with normal mammary artery where phosphorylated PKCδ was not detected (Figure 8). Interestingly, the staining of UPR markers with KDEL (Lys–Asp–Glu–Leu) antibody that recognizes both ER chaperones GRP78 and GRP94, was increased in advanced lesions and colocalized with PKCδ phosphorylated and the lipid peroxidation marker 4-hydroxynonenal (4-HNE). In normal artery, there was no KDEL or 4-HNE positivity. Furthermore, we confirmed that KDEL-, 4-HNE- and activated PKCδ-positive cells were foams cells (SMC and macrophages) of the necrotic core as shown by immunostaining of serial sections with anti-CD68 antibody. These results support our in vitro data and strongly suggest that PKCδ and ER stress may be activated by oxidized lipids within the atherosclerotic lesions.
PKCδ colocalized with ER stress and lipid peroxidation markers in advanced human carotid plaques. Immunostaining of human carotid plaque specimens (upper panel) and normal mammary arteries (lower panel) with anti-phosphotyrosine 311 PKCδ, anti-KDEL, anti-4-HNE-adduct, anti-CD68 and anti-α-actin antibodies. The scale bars represent 50 μm (advanced carotid plaque) and 25 μm (normal mammary artery)
Discussion
OxLDL-induced apoptosis of vascular cells may contribute to the erosion and instability of atherosclerotic plaques, thereby increasing the risk of subsequent thrombotic events. In this study, we identified a novel regulatory pathway in oxLDL-induced apoptosis of VSMC. We report for the first time that PKCδ is activated by oxLDL in human VSMC and contributes to oxLDL-induced ER stress-dependent apoptotic signaling through the I IRE1α/JNK pathway.
The function of PKCδ depends on the cell type and specific stimulus but currently a large number of studies are consistent with the central role of PKCδ in the regulation of cell apoptosis in response to various apoptotic stimuli.25 We showed that knockdown of PKCδ expression significatively reduces the effect of oxLDL-induced apoptosis in primary human VSMC and reintroduction of PKCδ into PKCδ knockout cells restores their apoptotic capacity, indicating that PKCδ is sufficient to specifically control the ability of the cells to undergo apoptosis. In addition, the modulation of the expression of pro-apoptotic and pro-survival members of the Bcl-2 family and, the reduced release of cytochrome C in PKCδ knockout cells suggests that PKCδ plays a central role in the mitochondria-dependent apoptotic pathway triggered by oxLDL. Altogether our findings corroborate previous results showing that forced higher expression in normal VSMC increased their apoptotic responses to the H2O2.15 However, it has been demonstrated that SMC isolated from PKCδ knockout mice displayed decreased proliferation compared with wild-type SMC;26 thus, suggesting that PKCδ exhibits contrasting roles in cell death and cell proliferation. In our experimental conditions, we did not observe such modification in cell viability and cell number in human VSMC knockdown for PKCδ, therefore, supporting that the proapoptotic function of PKCδ depends on the biological context.
PKCδ is activated by a large array of stimuli including mechanical stress, pro-inflammatory cytokines and oxidative stress, which are known to be associated with vascular remodeling and atherogenesis. The generation of ROS induced by oxLDL raises the question regarding how PKCδ is activated, which may include binding of second messenger diacyglycerol, phosphorylation, membrane translocation and proteolysis. One of the key event involved in the transduction of a death signal to PKCδ is the phosphorylation of PKCδ on tyrosine residues. In this study, we provided evidence that the rise in intracellular ROS triggered the phosphorylation of the tyrosine 311 residue of PKCδ which have been linked to increased kinase activity and apoptosis in cells treated with H2O2.18 The inhibitory effect of VAS2870, a well-validated specific inhibitor of NADPH oxidase (NOX),27 on oxLDL-induced ROS production and PKCδ tyrosine 311 phosphorylation raises the question of the enzymatic sources of ROS. Our data are consistent with the work of Stielow who showed that the VAS2870 inhibited28 oxLDL-induced ROS production in HUVEC. Moreover, the antioxidant enzyme catalase exerts the same inhibitory effect as VAS2870, which also supports a potential role of H2O2 generated by oxLDL treatment on PKCδ activation.
The main substrates of PKCδ in apoptotic cells are nuclear proteins and it has been shown that PKCδ translocates from the cytoplasm to the nucleus in response to specific apoptotic stimuli.29 Indeed, a nuclear localization sequence (NLS) has been defined in PKCδ that is required for its ability to induce apoptosis.30 As we observed a nuclear localization of PKCδ following oxLDL stimulation, we can hypothesize that oxLDL through the production of ROS, may induce post-translational modifications in PKCδ, which allow its translocation into the nucleus. Although in some systems, apoptotic cell death is associated with caspase-3-dependent cleavage of PKCδ, we did not observe any formation of the catalytically active fragment of PKCδ in our cellular model following oxLDL treatment. Nevertheless, our results are consistent with other reports showing lack of proteolytic cleavage of PKCδ in H2O2-rendered apoptotic CHO cells18 or in phorbol ester-induced apoptosis in prostate cancer cells.31
In agreement with our previous data reporting that oxLDL induced UPR and triggered ER stress-dependent apoptosis in human endothelial cells,7, 11 the current study demonstrated the activation of UPR sensors/ER stress in human VSMC exposed to oxLDL. The cellular response to a prolonged and excessive ER stress includes the activation of signaling pathways, which lead to apoptosis as supported by the increased expression of the proapoptotic factor CHOP/GADD53 and its targets BIM and PUMA, and the activation of the IRE1/JNK pathway in oxLDL-stimulated VSMC. To go further on the mechanisms mediating the apoptotic effect of PKCδ, we examined the potential link between ER stress and PKCδ Interestingly, we found that PKCδ participates in oxLDL-induced ER stress-dependent apoptotic signaling mainly through the IRE1α/JNK pathway. Indeed, we observed that in PKCδ−/− cells, oxLDL induced PERK activation, ATF6 nuclear translocation and CHOP induction but not IRE1α/JNK activation, which is consistent with previous report showing that inhibition of PKCδ reduces ER stress-induced JNK activation in Neuro2a cells.23 However, the regulatory role of PKCδ on ER stress is dependent on the signaling pathway triggered by the stimuli as thapsigargin induced UPR in cells expressing or not PKCδ, thus, indicating that PKCδ does not globally regulate ER stress.
The physiological importance of PKCδ in the development of atherosclerotic lesions is evidenced by our immunohistological analyses as we observed the expression of tyrosine 311 phosphorylated PKCδ in advanced human atherosclerotic lesions. Interestingly, the expression of phosphorylated PKCδ colocalized in atherosclerotic areas containing 4-HNE adducts and ER stress marker such as KDEL-positive cells, thus, suggesting that oxLDL through lipid peroxidation derivatives may locally contribute to trigger PKCδ activation and ER stress. These findings indicate that a similar activation mechanism of PKCδ such as we described in human VSMC exists in the atherosclerotic lesion. Moreover, our results corroborate the work of Yamanouchi et al.15 that showed a robust expression of PKCδ in apoptotic cells of human restenotic lesions.
Finally, our study identify for the first time PKCδ as a major regulator of oxLDL-induced apoptosis in VSMC, we also provide evidence that ROS generated by oxLDL are responsible for PKCδ activation. Furthermore, the involvement of PKCδ in the transmission of ER stress-dependent apoptotic signaling mainly through the IRE1α/JNK pathway, points out that PKCδ is involved in the fine tuning of apoptosis and raises the question of its role in the stability of atherosclerotic plaque.
Materials and Methods
Reagents
Cell culture reagents were from Invitrogen Life Technologies (Saint Aubin, France). SYTO-13, propidium iodide and 6-carboxy-2′,7′-dichlorodihydrofluorescein diacetate (H2DCFDA) were from Molecular Probes (Invitrogen). VAS2870 was from Enzo Life Sciences (Villeurbanne, France), PEG-Catalase and 3-(4,5 dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), antimycin A from Sigma-Aldrich (Lyon, France). z-VAD-FMK was from R&D Systems Europe (Lille, France). Thapsigargin is from Calbiochem (Millipore, Saint-Quentin-en-Yvelines, France). Following antibodies were used: anti-phospho-PKCδ, anti-IRE1α, anti-phospho-eIF2α, anti-phospho-JNK, anti-CHOP, anti-caspase-3, anti-cleaved caspase-3, anti-Bak, anti-Bim and anti-PUMA were from Cell Signaling Technology (Ozyme, Saint-Quentin-en-Yvelines, France), anti-ATF6 and anti-KDEL from Santa Cruz Biotechnology (Clinisciences, Nanterre, France), anti-cytochrome C from BD Biosciences (Le Pont de Claix, France), monoclonal anti-β-actin and anti-α-actin from Sigma-Aldrich), anti-4-HNE-adducts from Oxis Int (Foster City, CA, USA) and anti-CD68 was from NeoMarkers (Lab Vision, Fremont, CA, USA). Secondary antibodies anti-mouse and anti-rabbit were from Santa Cruz Biotechnology and Alexa fluor 488 was from Molecular Probes (Invitrogen). The ECL chemoluminescence kit was from Amersham Pharmacia (GE Healthcare, Ramonville Saint Agne, France). Hiperfect transfection reagent was from Qiagen (Les Ulis, France).
Cell culture
Human primary VSMC were obtained from human mesenteric arteries at postmortem examinations. All experiments were conformed to the declaration of Helsinki in compliance with French legislation and written informed consent was obtained from patients for the use of surgery residual tissue for research. Briefly, the arteries were cut longitudinally and small pieces of the media were carefully stripped from the vessel wall and cultured. Within 1–2 weeks, SMC migrated from the explants; they were capable of being passaged 3 weeks after the first appearance of cells. They were identified as VSMC by their characteristic hill-and-valley growth pattern and immunohistochemistry for VSMC-specific α-actin. The primary cultured human VSMC were used to generate an immortalized cell line by using SV40T antigen, SV40T-expressing human VSMC retain expression of contractile phenotype markers including smooth muscle α-actin and smMHC to passage 10 and higher as we previously described.32 For all experiments, passage 7–17 SV40T-expressing human VSMC cultures were used. The cultures were maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal calf serum at 37 °C in a humidified, 5% CO2/95% air atmosphere. MEF from PKCδ−/− mice and wild-type MEF were a generous gift from Pr. Mary E Reyland (University of Colorado Denver, USA).33 MEF PKCδ−/− and WT were maintained in DMEM supplemented with 10% fetal calf serum at 37 °C in a humidified, 5% CO2/95% air atmosphere.
Adenovirus expression in MEF PKCδ−/−
The generation and the use of Ad PKCδ–GFP and AdGFP have been described previously.33 MEF PKCδ−/− were infected with Ad PKCδ–GFP or AdGFP at a multiplicity (focus forming units/cell) of 100. Cells were infected in serum-free DMEM over night after which the virus containing medium was removed and replaced with normal medium. Infection was allowed to proceed for 24 h before stimulation with oxidized LDL.
LDL isolation and mild oxidation
LDL from human pooled sera were prepared by ultracentrifugation, dialyzed against PBS containing 100 μM EDTA. LDL were mildly oxidized by UV-C+copper/EDTA (5 μM) (oxLDL) as previously reported.34 OxLDL contained 4.2–7.4 nmol of TBARS (thiobarbituric acid−reactive substances)/μg apoB. Relative electrophoretic mobility (REM) and 2,4,6-trinitrobenzenesulfonic acid (TNBS) reactive amino groups were 1.2–1.3 times and 85–92% of native LDL, respectively.
Nuclear and cytosolic fractionation
Cells were washed once with PBS and lysed in a buffer containing 10 mM HEPES, 1.5 mM MgCl2, 10 mM KCl, 0.5 mM EDTA, 0.5 mM EDGA, proteases inhibitors, 0.1% Nonidet P-40 pH 7.9 for 10 min on ice and homogenates were centrifuged at 800 × g at 4 °C for 10 min. The supernatant that contains the cytoplasmic fraction was transferred and saved for western blotting analysis. The nuclear pellet was resuspended in extraction buffer containing 20 mM HEPES, 1.5 mM MgCl2, 0.2 mM EDTA, 100 mM NaCl, 26% glycerol (v/v), pH 7.9 for 30 min on ice with vortexing at 10-min internals. Homogenates were centrifuged for 30 min at 14 000 × g at 4 °C and the supernatant that contains the nuclear fraction was transferred and saved for western blotting analysis.
Western blot analysis
Cells were lysed in solubilizing buffer (10 mM Tris pH 7.4, 150 mM NaCl, 1% Triton X-100, 1% sodium deoxycholate, 0.1% sodium dodecyl sulfate, 1 mM sodium orthovanadate, 1 mM sodium pyrophosphate, 5 mM sodium fluoride, 1 mM phenylmethylsulfonyl fluoride, 1 μg/ml leupeptin, 1 μg/ml aprotinin) for 30 min on ice. In all, 40 μg of protein cell extracts were resolved by SDS-polyacrylamide gel electrophoresis, transferred onto PVDF membranes (Millipore). Then membranes were probed with the indicated primary antibodies and revealed with the secondary antibodies coupled to horseradish peroxidase using the ECL chemoluminescence kit. Membranes were then stripped and reprobed with anti-β-actin antibody to control equal loading of proteins.
Evaluation of cytotoxicity, necrosis and apoptosis
For cytotoxicity experiments, cells were serum starved for 24 h and stimulated for the indicated times at 37 °C. Cytotoxicity was evaluated using the MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) test, as previously used.7 This method is based on MTT reduction by the respiratory chain and other electron transport systems leading to form non-water-soluble violet formazan crystals that can be determined spectrophotometrically (OD measured at 570 nm) and serves as an estimate for the metabolic activity of living cells. Apoptotic and necrotic cells were counted after fluorescent staining by two fluorescent dyes, the permeant DNA intercalating green fluorescent probe SYTO-13 (0.6 μM) and the non-permeant DNA intercalating red fluorescent probe propidium iodide (15 μM) using an inverted fluorescence microscope (Fluovert FU, Leitz, Grand rapids, MI, USA) as previously described.7 Normal nuclei exhibit a loose green-colored chromatin. Nuclei of primary necrotic cells exhibit loose red-colored chromatin. Apoptotic nuclei exhibited condensed yellow/green-colored chromatin associated with nucleus fragmentation, whereas post-apoptotic necrotic cells exhibited the same morphological features, but were red-colored.
SiRNA transfection
The selected siRNA specific to human PKCδ were ON-TARGET plus SMART pool siRNA human PKCδ (Dharmacon, Waltham, MA, USA). SiRNAs were transfected using the Hiperfect reagent (Quiagen, Courtaboeuf, France) according to the manufacturer’s recommendations.
Immunofluorescence
Human VSMC grown on cover glass slides were washed with PBS and fixed in PBS/4% paraformaldehyde for 10 min. After blocking with PBS containing 3% BSA for 30 min, cells were incubated with the indicated antibodies for 1 h and revealed with Alexa Fluor 488-conjugated secondary antibody for 1 h. The slides were visualized using a Zeiss LSM 510 fluorescence confocal microscope (Le Pecq, France).
Quantification of intracellular ROS
The generation of intracellular ROS was estimated using the 6-carboxy-2′,7′-dichlorodihydrofluorescein diacetate (H2DCFDA) ROS-sensitive fluorescent probe (5 μM). Stimulated cells were incubated with the probe 30 min before determination as described.21
Immunohistochemistry
Human advanced carotid plaques (patients 70–75 years old) were obtained after endarterectomy (Cardiovascular Surgery Department, CHU Toulouse, France), internal mammary arteries were obtained from patients undergoing coronary artery bypass grafting. Tissues were fixed in formalin and paraffin embedded. Serial 3 μm thin sections were incubated with the anti-phosphotyrosine 311 PKCδ anti-KDEL, anti-4-HNE-adduct, anti-CD68 and anti-α-actin antibodies, then with appropriate biotin-labeled antibodies, and revealed by using avidin–biotin horseradish peroxidase visualization system (Vectastain, ABC kit Elite, Vector Laboratories, Burlingame, CA, USA). All experiments were conformed to the declaration of Helsinki in compliance with French legislation and written informed consent was obtained from patients for the use of surgery residual tissue for research.
Statistical analysis
Data are given as mean±S.E.M. Statistical comparison of the data was performed using the t-test for comparison between two groups and is explained in the figure legends (Sigma stat software, San Jose, CA, USA). Values of P<0.05 were considered statistically significant.
Abbreviations
- PKCδ:
-
protein kinase C δ
- oxLDL:
-
oxidized low-density lipoprotein
- ER stress:
-
endoplasmic reticulum stress
- VSMC:
-
vascular smooth muscle cells
- UPR:
-
unfolded protein response
- ROS:
-
reactive oxygen species
References
Steinberg D, Parthasarathy S, Carew TE, Khoo JC, Witztum JL . Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity. N Engl J Med 1989; 320: 915–924.
Napoli C . Oxidation of LDL, atherogenesis, and apoptosis. Ann NY Acad Sci 2003; 1010: 698–709.
Salvayre R, Auge N, Benoist H, Negre-Salvayre A . Oxidized low-density lipoprotein-induced apoptosis. Biochim Biophys Acta 2002; 1585: 213–221.
Clarke MC, Figg N, Maguire JJ, Davenport AP, Goddard M, Littlewood TD et al. Apoptosis of vascular smooth muscle cells induces features of plaque vulnerability in atherosclerosis. Nat Med 2006; 12: 1075–1080.
Ingueneau C, Huynh-Do U, Thiers JC, Negre-Salvayre A, Salvayre R, Vindis C . Caveolin-1 sensitizes vascular smooth muscle cells to mildly oxidized LDL-induced apoptosis. Biochem Biophys Res Commun 2008; 369: 889–893.
Ingueneau C, Huynh UD, Marcheix B, Athias A, Gambert P, Negre-Salvayre A et al. TRPC1 is regulated by caveolin-1 and is involved in oxidized LDL-induced apoptosis of vascular smooth muscle cells. J Cell Mol Med 2009; 13: 1620–1631.
Muller C, Salvayre R, Negre-Salvayre A, Vindis C . HDLs inhibit endoplasmic reticulum stress and autophagic response induced by oxidized LDLs. Cell Death Differ 2011; 18: 817–828.
Zhang K, Kaufman RJ . From endoplasmic-reticulum stress to the inflammatory response. Nature 2008; 454: 455–462.
Marciniak SJ, Yun CY, Oyadomari S, Novoa I, Zhang Y, Jungreis R et al. CHOP induces death by promoting protein synthesis and oxidation in the stressed endoplasmic reticulum. Genes Dev 2004; 18: 3066–3077.
McCullough KD, Martindale JL, Klotz LO, Aw TY, Holbrook NJ . Gadd153 sensitizes cells to endoplasmic reticulum stress by down-regulating Bcl2 and perturbing the cellular redox state. Mol Cell Biol 2001; 21: 1249–1259.
Sanson M, Auge N, Vindis C, Muller C, Bando Y, Thiers JC et al. Oxidized low-density lipoproteins trigger endoplasmic reticulum stress in vascular cells prevention by oxygen-regulated protein 150 expression. Circ Res 2009; 104: 328–U102.
Myoishi M, Hao H, Minamino T, Watanabe K, Nishihira K, Hatakeyama K et al. Increased endoplasmic reticulum stress in atherosclerotic plaques associated with acute coronary syndrome. Circulation 2007; 116: 1226–1233.
Reyland ME . Protein kinase Cdelta and apoptosis. Biochem Soc Trans 2007; 35: 1001–1004.
Leitges M, Mayr M, Braun U, Mayr U, Li C, Pfister G et al. Exacerbated vein graft arteriosclerosis in protein kinase Cdelta-null mice. J Clin Invest 2001; 108: 1505–1512.
Yamanouchi D, Kato K, Ryer EJ, Zhang F, Liu B . Protein kinase C delta mediates arterial injury responses through regulation of vascular smooth muscle cell apoptosis. Cardiovasc Res 2010; 85: 434–443.
Greene MW, Ruhoff MS, Burrington CM, Garofalo RS, Orena SJ . TNFalpha activation of PKCdelta, mediated by NFkappaB and ER stress, cross-talks with the insulin signaling cascade. Cell Signal 2010; 22: 274–284.
Yang H, Chen S, Tang Y, Dai Y . Interleukin-10 down-regulates oxLDL induced expression of scavenger receptor A and Bak-1 in macrophages derived from THP-1 cells. Arch Biochem Biophys 2011; 512: 30–37.
Konishi H, Yamauchi E, Taniguchi H, Yamamoto T, Matsuzaki H, Takemura Y et al. Phosphorylation sites of protein kinase C delta in H2O2-treated cells and its activation by tyrosine kinase in vitro. Proc Natl Acad Sci USA 2001; 98: 6587–6592.
Kato K, Yamanouchi D, Esbona K, Kamiya K, Zhang F, Kent KC et al. Caspase-mediated protein kinase C-delta cleavage is necessary for apoptosis of vascular smooth muscle cells. Am J Physiol Heart Circ Physiol 2009; 297: H2253–H2261.
Bouguerne B, Belkheiri N, Bedos-Belval F, Vindis C, Uchida K, Duran H et al. Antiatherogenic effect of bisvanillyl-hydralazone, a new hydralazine derivative with antioxidant, carbonyl scavenger, and antiapoptotic properties. Antioxid Redox Signal 2011; 14: 2093–2106.
Robbesyn F, Garcia V, Auge N, Vieira O, Frisach MF, Salvayre R et al. HDL counterbalance the proinflammatory effect of oxidized LDL by inhibiting intracellular reactive oxygen species rise, proteasome activation, and subsequent NF-kappaB activation in smooth muscle cells. FASEB J 2003; 17: 743–745.
Beckman JS, Minor RL, White CW, Repine JE, Rosen GM, Freeman BA . Superoxide dismutase and catalase conjugated to polyethylene glycol increases endothelial enzyme activity and oxidant resistance. J Biol Chem 1988; 263: 6884–6892.
Qi X, Mochly-Rosen D . The PKCdelta-Abl complex communicates ER stress to the mitochondria—an essential step in subsequent apoptosis. J Cell Sci 2008; 121 (Pt 6): 804–813.
Chiu SC, Chen SP, Huang SY, Wang MJ, Lin SZ, Harn HJ et al. Induction of apoptosis coupled to endoplasmic reticulum stress in human prostate cancer cells by n-butylidenephthalide. PLoS One 2012; 7: e33742.
Reyland ME . Protein kinase C isoforms: multi-functional regulators of cell life and death. Front Biosci 2009; 14: 2386–2399.
Liu B, Ryer EJ, Kundi R, Kamiya K, Itoh H, Faries PL et al. Protein kinase C-delta regulates migration and proliferation of vascular smooth muscle cells through the extracellular signal-regulated kinase 1/2. J Vasc Surg 2007; 45: 160–168.
Altenhofer S, Kleikers PW, Radermacher KA, Scheurer P, Rob Hermans JJ, Schiffers P et al. The NOX toolbox: validating the role of NADPH oxidases in physiology and disease. Cell Mol Life Sci 2012; 69: 2327–2343.
Stielow C, Catar RA, Muller G, Wingler K, Scheurer P, Schmidt HH et al. Novel Nox inhibitor of oxLDL-induced reactive oxygen species formation in human endothelial cells. Biochem Biophys Res Commun 2006; 344: 200–205.
Brodie C, Blumberg PM . Regulation of cell apoptosis by protein kinase c delta. Apoptosis 2003; 8: 19–27.
DeVries TA, Neville MC, Reyland ME . Nuclear import of PKCdelta is required for apoptosis: identification of a novel nuclear import sequence. EMBO J 2002; 21: 6050–6060.
Fujii T, Garcia-Bermejo ML, Bernabo JL, Caamano J, Ohba M, Kuroki T et al. Involvement of protein kinase C delta (PKCdelta) in phorbol ester-induced apoptosis in LNCaP prostate cancer cells. Lack of proteolytic cleavage of PKCdelta. J Biol Chem 2000; 275: 7574–7582.
Galvani S, Trayssac M, Auge N, Thiers JC, Calise D, Krell HW et al. A key role for matrix metalloproteinases and neutral sphingomyelinase-2 in transplant vasculopathy triggered by anti-HLA antibody. Circulation 2011; 124: 2725–2734.
Humphries MJ, Limesand KH, Schneider JC, Nakayama KI, Anderson SM, Reyland ME . Suppression of apoptosis in the protein kinase Cdelta null mouse in vivo. J Biol Chem 2006; 281: 9728–9737.
Vindis C, Elbaz M, Escargueil-Blanc I, Auge N, Heniquez A, Thiers JC et al. Two distinct calcium-dependent mitochondrial pathways are involved in oxidized LDL-induced apoptosis. Arterioscler Thromb Vasc Biol 2005; 25: 639–645.
Acknowledgements
We thank JC Thiers, C Fouré, A Matassa-Ohm for excellent technical help and Dr. V Gallet (SNCF Laboratory, Toulouse, France) for providing human serum. We are grateful to Dr. F Lezoualc’h for critical reading of the manuscript. These studies were supported by grants from INSERM and Toulouse 3 University to INSERM U1048 team 10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by Y Shi
Supplementary Information accompanies this paper on Cell Death and Disease website
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Larroque-Cardoso, P., Swiader, A., Ingueneau, C. et al. Role of protein kinase C δ in ER stress and apoptosis induced by oxidized LDL in human vascular smooth muscle cells. Cell Death Dis 4, e520 (2013). https://doi.org/10.1038/cddis.2013.47
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2013.47