Abstract
Kt/Vurea ratio is commonly used to assess the delivered dose of dialysis in maintenance hemodialysis (MHD) patients. This parameter only reflects the efficacy of dialytic treatments in removing small toxins, but not middle and protein-bound toxins. Erythrocyte glutathione transferase (e-GST), an enzyme devoted to cell depuration against a lot of large and small toxins, is overexpressed in uremic patients. Aim of the present study is to verify whether e-GST may represent a novel biomarker to assess the adequacy of different dialytic techniques complementary to Kt/Vurea parameter. Furthermore, it will be investigated whether e-GST could reflect the ‘average’ adequacy of multiple dialytic sessions and not of a single one treatment as it occurs for Kt/Vurea. One hundred and three MHD patients and 82 healthy subjects were tested. Fourty four patients were treated with standard bicarbonate hemodialysis (HD) and 59 patients were on online hemodiafiltration (HDF). In all MHD patients e-GST activity was 60% higher than in healthy controls. In HDF, e-GST activity was lower than in HD subgroup (8.2±0.4 versus 10.0±0.4 U/gHb, respectively). Single-pool Kt/Vurea and total weekly Kt/Vurea were higher in HDF than in HD, but no correlation was found between e-GST activity and Kt/Vurea data. e-GST, whose level is stable during the erythrocyte life-span, provides information on the long-term depurative efficacy of dialysis treatments.
Similar content being viewed by others
Main
Uremic syndrome is characterized by the accumulation of uremic toxins due to inadequate kidney function. In literature more than 90 compounds are identified as uremic toxins. The European Uremic Toxin (EUTox) Work Group proposed a practical classification based on physical–chemical characteristics that influence their dialytic removal:1 small solutes (<500 Da), with urea as a prototypal compound, ‘middle molecules’ (>500 Da) such as beta-2-microglobulin, and large solutes, which include an heterogeneous class of molecules such as small and middle protein-bound molecules that are bound to plasma proteins (these include for instance p-cresol, homocysteine and a series of reactive carbonyls such as 4-hydroxynonenal, malondialdehyde, methylglyoxal and so on), tissue proteins released by cell damage and products of protein damage by the reaction with reactive oxygen species and reducing sugars, and the products of their metabolism by proteolytic events, cross-linking and so on.2, 3, 4
An ideal dialytic therapy should remove all of these compounds. However, only small toxins are easily removed by all dialytic techniques, even if some improvements have been introduced by the use of more efficient dialyser membranes such as advanced high-flux and protein-leaking hemodialyser membranes, and treatment methods that are based for instance on hemodiafiltration (HDF) techniques.5, 6, 7
Despite this, the hemodialysis adequacy and dosing are usually discussed only in terms of Kt/Vurea, a mathematical model that takes into account the urea clearance in a single hemodialysis session.8, 9 Recent studies showed that Kt/Vurea in dialysis cannot represent correctly the removal of other solutes and fluid, indicating that this parameter alone should not be used as the sole indicator of dialysis adequacy.10, 11 Thus, other dialysis biomarkers have been proposed (i.e., p-cresol,12 beta-2-microglobulin,13 guanidine compounds,14 high-throughput molecular fingerprinting assays15), but their quantifications require complex and expensive procedures and again they only measure the efficiency of a single dialytic session. Thus, the identification of new clinical indicators able to reveal the degree of blood purification from small as well as large toxins in a wide range of dialytic sessions will be of medical interest.
Erythrocyte glutathione transferase (e-GST), an enzyme compartmentalized in the red cells and then non-dialyzable, could be ideal for this role. GSTs represent a super-family of ubiquitous enzymes devoted to cell protection16 by promoting the conjugation of glutathione with toxins of very different shapes.17, 18 Alternatively, GSTs may act as ligandins by binding and sequestering a variety of small or large toxic compounds and peptides. An example of this ligandin role is the specific binding of GSTP1-1 to Jun-kinase, a pro-apoptotic enzyme that becomes inactive when bound to GST.19 Human cytosolic GSTs are dimeric proteins grouped into seven different gene-independent classes termed Alpha, Mu, Pi, Theta, Omega, Sigma and Zeta. Human glutathione transferase P1-1 (hGSTP1-1) is a homodimeric intracellular protein of about 46 kDa expressed in different organs and cell types. The GSTP1-1 is the most abundant form of intra-erythrocyte transferase representing 95% of entire GST pool.20
In healthy subjects, the intra-cellular level of e-GST remains virtually constant during childhood and adult life,21 increasing only in two pathological conditions, that is hyperbilirubinemia and uremia.22, 23 No other pathologies have been reported to induce e-GST hyper-activity. We recently confirmed these results observing that the activity of e-GST increases from 5.8±0.4 U/gHb in healthy subjects to 10.2±0.5 U/gHb in maintenance hemodialysis (MHD) patients.24 This hyper-activity represents a defense reply against systemic toxicity of the uremic condition. For the first time a significant increase in e-GST activity has been also found in chronic kidney disease patients under conservative therapy with a positive correlation with disease severity weighted according to the five stages of chronic renal failure of ‘kidney disease outcomes quality initiative’ (K-DOQI) classification.24 Interestingly, patients belonging to the fourth stage display e-GST activity (12±1 U/gHb) higher than those under dialysis (10.2±0.4 U/gHb), confirming that e-GST may be a reasonable natural biomarker of blood toxicity,24 that is an endogenous probe whose concentration reflects the level of circulating toxins. The aim of the present study is to verify whether e-GST may represent a novel biomarker able to assess the adequacy of different dialytic techniques (i.e., standard bicarbonate hemodialysis (HD) and HDF) complementary to the Kt/Vurea parameter. Furthermore, it will be investigated whether e-GST could reflect the adequacy not of a single treatment but of many dialytic sessions accomplished during a few weeks. The possible correlation between e-GST activity and single-pool Kt/Vurea (spKt/Vurea) and total weekly Kt/Vurea will be also investigated. Results obtained open the way to further clinical studies on the use of e-GST as biosensor for long-time exposure to uremic toxicity and dialysis efficiency.
Results
GST hyper-activity in dialyzed patients
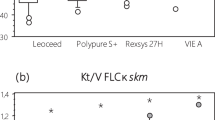
One hundred and eighty five healthy subjects and uremic patients have been involved in this study and some epidemiological parameters are shown in Table 1. Furthermore, the number of patients grouped for primary causes of end-stage renal disease (ESRD) (Table 1) did not differ between HD and HDF subgroups. On 82 healthy subjects (control group), e-GST activity was 5.6±0.4 U/gHb, a value very close to that reported in a previous investigation.24 For the 103 uremic patients their e-GST activity was 9.0±0.3 U/gHb (Figure 1a and Table 2).
e-GST activity in all the uremic patients (HD- and HDF group) and in the Control group. (a) aP<0.0001 e-GST activity in total uremic patients versus Control group. bP<0.0001 e-GST activity in HD group versus HDF group. (b) Relative increase in e-GST activity from the mean value of healthy subjects observed in HD group and in HDF group
On comparing the e-GST activities of the control group versus all uremic patients, we observed a significant statistically difference (P<0.0001) (Figure 1a). Moreover, we investigated whether the e-GST activity was related to different hemodialysis techniques (convective versus diffusive) and/or to dialytic dose.
First, we matched HDF and HD groups for e-GST and several parameters (Table 2). In the 59 HDF-group patients the mean spKt/Vurea and total weekly Kt/Vurea were 1.50±0.03 and 4.6±0.1 respectively; the mean e-GST activity was 8.2±0.4 U/gHb. For the 44 HD-group, the mean spKt/Vurea value was 1.30±0.05, the total weekly Kt/Vurea 3.9±0.1, whereas the mean e-GST activity of this group was 10.0±0.4 U/gHb. The difference in e-GST activity between the HD-group and HDF-group is better highlighted in Figure 1b, where the relative increase of e-GST (from the mean value of healthy subjects) is reported.
From statistical analysis, we found no differences for age, HD vintage, albumin, EPO dose, EPO resistance index (ERI) and high-sensitivity C-reactive protein (hs-CRP), between the two groups (Table 2). However, we observed statistical significant differences for e-GST activity (P=0.003), blood urea nitrogen (BUN)-predialysis (P=0.0001), spKt/Vurea (P=0.0002) and total weekly Kt/Vurea (P=0.0006) (Table 2).
In a second experimental step, we evaluated whether e-GST activity is related to the dialytic dose. For this purpose, all uremic patients were divided in two subgroups, using a cutoff⩾1.3 for Kt/Vurea, according to NFK-DOQI guidelines.25 In patients with spKt/Vurea<1.3, e-GST was 9.7±0.7 (S.D.=3.2), whereas in patients with spKt/Vurea⩾1.3 was 8.7±0.4 (S.D.=2.9), without any statistically significant difference (P=0.156) (Figure 2). In addition, we did not find any linear correlation between e-GST activity and sp Kt/Vurea values in all uremic patients (r2=0.0378; P=0.049). Other established markers for malnutrition, inflammation and dialysis efficiency showed slight or no correlation with e-GST, that is albumin (r2=0.0202, P=0.153), hs-CRP (r2=0.0336; P=0.064), BUN predialysis (r2=0.1906; P<0.001), BUN postdialysis (r2=0.0822; P=0.003). Furthermore, to assess whether the administration of EPO may influence the e-GST activity, we evaluated the possible correlation between e-GST and variables like EPO dose and ERI. We did not find any linear correlation between e-GST and EPO dose (r2=0.0199, P=0.139) or e-GST and ERI (r2=0.0396, P=0.0797).
Hyper-activity of e-GST is due to hyper-expression of the enzyme
Various factors may cause the hyper-activity of e-GST observed in uremic patients. For example, it is well known that the life-span of RBC is shorter in hemodialysis patients26 and that young RBC display somewhat higher GST activity than old RBC.27 Previous observations, however, showed that the proportion of young and old cells are the same, but e-GST was higher in hemodialysis patients than in healthy controls.23 This difference was particularly pronounced in young cells and decreased as cell age increased. Again, the supplementation with EPO, which might increase the number of young cells in circulation, was not found to interfere with the mean concentrations of e-GST in EPO-responsive patients.23 Thus, it may be concluded that the observed increased activity in uremic patients is not due to an increased proportion of young erythroid elements in the circulation.
Other factors may cause e-GST hyper-activity, that is the presence of intra-erythrocyte GST activators, post-translational enzyme modifications, overexpression or slower turnover break-down of this enzyme. Clarifying the origin of this hyper-activity will be essential to establish whether e-GST could be used as a biomarker for the adequacy of a single dialytic session or it reflects the dialytic efficiency of multiple dialytic sessions performed during several weeks. In fact, erythrocytes are enucleated cells and their enzyme biosynthesis does not occur in mature cells. Thus, although a post-translational activation or the presence of a specific enzyme activator could be a short-time responsiveness to an increased level of toxins, an overexpression of e-GST likely reflects a long-time-mediated exposition to toxins, which may be estimated on the basis of the erythrocytes survival (≈58.9 days for dialyzed patients).28 To solve this enigma, we compared the specific activity of e-GST purified with affinity chromatography from dialyzed patients with the one coming from healthy subjects. The similarity of the two values found in the fully purified samples (94±10 U/mg and 83±6 U/mg, respectively) suggests the increase of activity found in dialyzed patient to be due to a real increased level of this enzyme and not to enzyme activation (Figure 3a), confirming previous suggestions obtained by western blotting analysis.23 A further convincing evidence has been obtained using a very specific and selective inhibitor of e-GST, that is the dinitrosyl-diglutathionyl-iron complex. This compound binds with extraordinary affinity to all mammalian GSTs, with a KD of about 10−9 M29, 30 and causing a complete enzyme inhibition. This phenomenon is almost stoichiometric and allows a precise quantification of enzyme present in a given solution. As shown in Figure 3b the amount of DNDGIC necessary to inhibit 50% of e-GST purified from dialyzed patients (15 U/gHb) is about three times higher than that necessary for that from healthy subjects (5.6 U/gHb), indicating the presence of about three times higher concentration of e-GST in the dialyzed patients. Thus, e-GST hyper-activity reflects a true higher level of this protein in the erythrocyte. The occurrence of possible e-GST break-down during the erythrocyte life-span is never been described; on the contrary, an extraordinary stability of e-GST activity in intact erythrocytes has been reported.24 Thus, a reasonable (even if not definitive) explanation for the increased e-GST activity in dialyzed patients is that an overexpression of e-GST occurred in the maturation phase of the red cells. In this scenario e-GST may be considered a biosensor of average blood toxicity in a span of a few weeks. A convincing evidence that e-GST activity is not affected by a short-time variation of circulating toxins is reported in Figure 4 showing pre- and post-dialysis levels of e-GST of two patients (the first one under HD and the second one under HDF) measured during one week of therapy. In each patient, the e-GST activity is almost identical either in the pre and post dialysis as well as in the distinct dialytic sessions with a maximum variation of about 5% (average variation=4%) for the patient under HD and about 6% (average variation=3%) for the patient under HDF.
(a) Comparison between specific activities of e-GST purified by affinity chromatography from healthy controls (5.6 U/gHb) and hemodialysis patients (15 U/gHb), see Materials and Methods section. (b) The same e-GST samples used for experiment in (a) were mixed with variable amounts of DNDGIC and after 1 min incubation the residual activity was measured. Each point is the mean of three distinct measurements±S.E.M.
e-GST activity of two patients in distinct dialytic sessions during a week before (filled symbols) and after (open symbols) the hemodialysis treatment. (▪) diffusive dialysis; (●) convective dialysis. In the day 2, no dialysis has been performed. Each point represent the mean of three distinct activity measurements±S.E.M.
Discussion
All along nephrologists dose only few toxins to quantify the degree of renal dysfunction as well as to determine dialytic dose and adequacy in MHD patients using Kt/Vurea, as recommended by International guidelines. However, Kt/Vurea is an ‘urea-centric’ mathematical model commonly adopted to quantify the detoxification from a single compound in a single dialytic session. Curiously, doubts have arisen by considering urea as a true marker of the uremic disease as the EUTox group defined it as a ‘not necessarily toxic solute’.10 Indeed, uremic syndrome is more than urea accumulation and the toxic solutes that contribute to uremic illness are different from urea and probably most of them remain to be identified. As a consequence, adequate dose of dialysis is difficult to define because theoretically we should calculate the fractional removal of each single toxin and their intrinsic toxicity. Otherwise, even if nowadays Kt/Vurea provides a useful tool to avoid grossly inadequate dialysis and Kt/Vurea >1.3 is indicated by international guidelines as the ‘dose’ of dialysis to achieve, in the future the urea removal standard will be fundamentally flawed. Relatively recent studies on dialysis adequacy failed to demonstrate that increasing Kt/Vurea over 1.3 could decrease patient morbidity and improve survival.31, 32 Moreover, clinical studies have shown that a further limit of Kt/Vurea as a predictor of mortality, is that both terms of the ratio are predictors.33 Data presented in this paper suggest that e-GST may be an innovative tool able to measure the efficiency of a dialytic process complementary or alternative to the Kt/Vurea. In fact e-GST fulfills remarkable improvements and novelty elements: (a) it can be considered not as a classical biomarker, but more appropriately an endogenous biosensor of blood toxicity being naturally overexpressed when the toxin level increases; (b) its expression is reasonably linked not to the quantitative level of blood toxins nor to their size, but probably to their own specific toxicity; (c) contrary to the Kt/Vurea parameter, e-GST reflects the adequacy of multiple dialytic sessions within 1–2 months of life span of circulating erythrocytes; (d) spectrophotometric assay of e-GST activity is fast, requires only 0.05 ml of blood, and it is not expensive. As shown in Figure 3 data from the present study demonstrate that patients under convective hemodialysis express e-GST (8.2 U/gHb) significantly lower than that observed in patients under traditional diffusive hemodialysis (10.0 U/gHb), suggesting that the former group is exposed to a lower level of circulating toxins and thus to a more efficient dialytic therapy. This idea fully agree with recent observations, indicating an advantage of convective over pure diffusive strategies for patient survival.34 This e-GST variation observed in the two different hemodialytic treatments is not negligible; with e-GST activity in healthy subjects set as reference value, i.e., 5.6 U/gHb, the convective hemodialysis lowers the hyper-activity of e-GST observed in patients under diffusive hemodialysis by >43% (Figure 1b).
e-GST activity of patients under convective treatment (8.2 U/gHb) is, however, far from that expected from an ‘ideal’ dialysis that may be characterized by a GST value near that of the healthy group (5.6 U/gHb). Tentatively, a value <6 U/gHb could be the goal to be realized by means of future and more advanced dialysis procedures. In conclusion, e-GST seems to reveal toxicological aspects of uremic syndrome (Figure 1) wider than those of the urea-centric Kt/Vurea (Figure 2) explaining the absence of correlation between these two parameters. In this context it is not surprising that e-GST does not or poorly correlate with other established markers (albumin, hs-CRP, BUN predialysis and postdialysis), which reflect a short-term toxicity or the adequacy of a single dialytic session. As the erythrocyte is an enucleated cell, its enzymatic content is exclusively determined before or during its maturation and remains unchanged during the cell life-span, which is about 60 days in dialyzed patients.28 Data presented in this paper demonstrate that the increased e-GST activity found in dialyzed patients is likely due to an hyper-expression of the enzyme and not due to an enzymatic activation (Figure 3). Thus, e-GST activity must reflect reasonably a blood exposure to toxins during about 2 months and then the ‘average’ adequacy of multiple dialytic sessions. This property, also confirmed by the invariance of e-GST activity during distinct dialytic sessions within a week or before/after a single dialysis (Figure 4), displays analogy with HbA1c used as long-term marker for blood exposure to glucose35 and make e-GST a marker of uremic toxicity and dialytic adequacy very different from Kt/Vurea. A larger trial involving several hundreds of dialyzed patients is now in progress in a number of Italian dialysis centers to further confirm the relevance of e-GST in the clinical monitoring of ESRD patients.
Materials and Methods
Patients and study design
The study protocol complied with the declaration of Helsinki and a written fully informed consent was provided by all patients and healthy subjects before enrollment into the study. The present research is approved by the Ethical Committee of our Institution (Comitato Etico Indipendente dell’Azienda Ospedaliera Universitaria Policlinico Tor Vergata).
The study is a cross-sectional investigation of healthy subjects and MHD patients. Eighty-two healthy controls with normal renal function and no history of diabetes mellitus served as healthy controls. Blood samples were collected from the anticubital vein and stored into K-3-EDTA tubes at 4 °C for no more than 2 days.
One hundred and three uremic patients were enrolled. Inclusion criteria were: age between 18 and 80 years, hemodialytic therapy since 6 months at least and the same hemodialysis technique since 3 months. Blood samples were collected from the arterial site of the vascular access before the dialysis at the end of the long interdialytic interval. Samples were stored with the same modality as for the control group.
Exclusion criteria in both healthy controls and MHD patients were a clinical history of virus hepatitis B and C or serum alanine aminotransferase and/or aspartate aminotransferase twice the upper limit of normal values, morbid obesity, rheumatologic disorders (as systemic lupus erythematosus), hyperbilirubinemia (such as Gilbert’s syndrome), active cancer and pregnancy. Gender, mean age, HD vintage and cause of end-stage renal disease are shown in Table 1.
Clinical parameters
Hemoglobin (Hb) was determined with an automated hematology analyzer XE-2100 (Sysmex, Kobe, Japan). Albumin, BUN and hs-CRP measurements were performed by an automated method using Dimension VISTA 1500 (Siemens Healthcare Diagnostics, Milano, Italy).
EPO dose and ERI
In order to normalize the amount of EPO required depending on the severity of anemia, we calculated an ERI, defined as the weekly EPO dose divided by Hb level (g/dl). Both the EPO dose and ERI were divided by end-dialysis body weight to indicate the required EPO dose per kilogram of body weight. A ratio of 1 : 200 was used to convert darbepoetin alpha to the EPO equivalent dose (1 μg of darbepoetin alpha=200 IU of epoetin alpha or beta).36
Dialysis therapy
MHD patients were divided in two subgroups, based on dialysis technique: 44 out of 103 patients underwent to HD and 59 patients were on HDF therapy. HD patients were treated with 1.5–2.0 m2 surface area polysulphone or polyamide hollow-fiber hemodialysers, whereas 1.4–2.1 m2 polysulphone or polyamide hollow-fiber dialyser membranes were used in the HDF group. All patients underwent 4 h three times/week dialysis protocol, with a well-functioning native artero–venous fistula or a cuffed internal jugular indwelling venous catheter, as vascular access. All uremic patients were characterized according to sex, age and dialytic vintage; hemodialysis adequacy was assessed with spKt/Vurea and total weekly Kt/Vurea using the Daugirdas second-generation formula.37
e-GST activity
e-GST activity was determined with a spectrophotometric assay at 340 nm (37 °C), using a Modular P800 (Roche, Basel, Switzerland) automated apparatus recently described.24 Briefly, one volume (40 μl) of whole blood was diluted in 25 volumes (1 ml) of bi-distilled water and after 5 min introduced into the Modular P800, final volume containing 1 mM glutathione (GSH), 1 mM 1-chloro-2,4-dinitrobenzene (CDNB) in 0.1 M potassium phosphate buffer, pH 6.5. Results were expressed as enzyme units (U) per gram of Hb (U/gHb): one unit represents the amount of enzyme that catalyzes the conjugation of 1 μM of GSH to CDNB in 1 min at 37 °C. The Hb level was determined with an automated hematology analyzer XE-2100 (Dasit, Milano, Italy). To calculate Kt/Vurea, urea was assayed by nephelometric methods (BN IITM BNHTM nephelometer, Siemens Healthcare Diagnostics, Milano, Italy).
Purification of e-GST and its reaction with DNDGIC
e-GST purification from hemolyzed erythrocytes of healthy and dialyzed patients was performed with a single-step affinity chromatography method using S-hexylglutathione Sepharose 6B.38 Protein concentration was determined using the procedure described by Lowry et al.39 Dinitrosyl–diglutathionyl–iron complex (DNDGIC) was prepared as described previously by reacting S-nitrosoglutathione with ferrous sulphate in the presence of 10 mM GSH.29, 30 Its reaction with purified e-GST, from healthy or dialyzed subjects, was performed in 0.01 M potassium phosphate buffer, pH 7.0 by adding variable amounts of DNDGIC. After 1 min of incubation, the degree of inhibition was evaluated on aliquots with the standard assay procedure for GST activity.
Statistical analysis
All data were expressed as mean±S.E.M. P values reported in the text and in tables have been estimated on the basis of the mean±S.D. Unpaired t test was employed to compare the data between various groups; non parameter variables were analyzed by Mann–Whitney test. A value of P<0.05 was considered statistically significant. To study the linear relationship between e-GST activity and other variables, non parametric correlation (Spearman p) was used. Data were processed using statistical software MedCalc (Mariakerke, Belgium).
Abbreviations
- ADPKD:
-
autosomal dominant polycystic kidney disease
- BUN:
-
blood urea nitrogen
- CDNB:
-
1-chloro-2,4-dinitrobenzene
- hs-CRP:
-
high-sensitivity C-reactive protein
- DNDGIC:
-
dinitrosyl-diglutathionyl–iron complex
- e-GST:
-
erythrocyte glutathione transferase
- EPO:
-
erythropoietin
- ERI:
-
EPO resistance index
- ESRD:
-
end-stage renal disease
- GSH:
-
glutathione
- Hb:
-
hemoglobin
- HD:
-
standard bicarbonate hemodialysis
- HDF:
-
hemodiafiltration
- K-DOQI:
-
kidney disease outcomes quality initiative
- MHD:
-
maintenance hemodialysis
- spKt/Vurea:
-
single-pool Kt/Vurea
References
Vanholder R, De Smet R, Glorieux G, Argilè A, Baurmeister U, Brunet P et alFor the European Uremic Toxin Work Group. (EUTOX). Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Inter 2003; 63: 1934–1943.
Yavuz A, Tetta C, Ersoy FF, D'Intini V, Ratanarat R, De Cal M et al. Uremic toxins: a new focus on an old subject. Semin Dial 2005; 18: 203–211.
Galli F . Protein damage and inflammation in uremia and dialysis patients. Nephrol Dial Transplant 2007; 22 (Suppl 5): 20–36.
Jourde-Chiche N, Dou L, Cerini C, Dignat-George F, Vanholder R, Brunet P . Protein-bound toxins-update 2009. Semin Dial 2009; 22: 334–339.
De Smet R, Dhondt A, Eloot S, Galli F, Waterloos MA, Vanholder R . Effect of the super-flux cellulose triacetate dialyser membrane on the removal of non-protein-bound and protein-bound uraemic solutes. Nephrol Dial Transplant 2007; 22: 2006–2012.
Krieter DH, Hackl A, Rodriguez A, Chenine L, Moragues HL, Lemke HD et al. Protein-bound uraemic toxin removal in haemodialysis and post-dilution haemodiafiltration. Nephrol Dial Transplant 2010; 25: 212–218.
Galli F, Benedetti S, Buoncristiani U, Canestrai F, Piroddi M, Buoncristiani E et al. Glycoxidation and inflammatory markers in patients on treatment with PMMA-based protein-leaking dialysers. Kidney Int 2005; 67: 750–759.
Gotch FA, Sargent JA . A mechanistic analysis of the National Cooperative Dialysis Study (NCDS). Kidney Int 1985; 28: 526–534.
K/DOQI, National Kidney Foundation Clinical practice guidelines for nutrition in chronic renal failure. Am J Kidney Dis 2000; 35 (Suppl 2): S1–S140.
Basile C, Lomonte C . Kt/V urea does not tell it all. Nephrol Dial Transplant 2012; 0: 1–4.
Meyer TW, Sirich TL, Hostetter TH . Dialysis cannot be dosed. Semin Dial 2011; 24: 471–479.
De Smet R, Van Kaer J, Van Vlem B, De Cubber A, Brunet P, Lameire N et al. Toxicity of free p-cresol: a prospective and cross-sectional analysis. Clin Chem 2003; 49: 470–478.
Vanholder R, De Smet R, Vogeleere P, Ringoir S . Middle molecules: Toxicity and removal by hemodialysis and related strategies. Artif Organs 1995; 19: 1120–1125.
Eloot S, Torremans A, De Smet R, Marescau B, De Deyn PP, Verdonck P et al. Complex compartmental behavior of small water-soluble uremic retention solutes: Evaluation by direct measurements in plasma and erythrocytes. Am J Kidney Dis 2007; 50: 279–288.
Weissinger EM, Kaiser T, Meert N, De Smet R, Walden M, Mischak H et al. Proteomics: a novel tool to unravel the patho-physiology of uraemia. Nephrol Dial Transplant 2004; 19: 3068–3077.
Armstrong RN . Structure, catalytic mechanism, and evolution of the glutathione transferases. Chem Res Toxicol 1997; 10: 2–18.
Jakoby WB, Keen JH . A triple-threat in detoxification: the glutathione-S-transferase. Trends Biochem Sci 1997; 2: 223–229.
Jakoby WB . The gluthatione-S-transferase: a group of multifunctional detoxification proteins. Adv Enzymol 1978; 46: 383–414.
Adler V, Yin Z, Fuchs SY, Benezra M, Rosario L, Tew KD et al. Regulation of JNK signaling by GSTp. EMBO J 1999; 18: 1321–1334.
Awasthi YC, Sharma R, Singhal SS . Human glutathione S-transferase. Int J Biochem 1994; 26: 295–308.
Strange RC, Johnston JD, Coghill DR, Hume R . A comparison of erythrocyte glutathione-S-transferase activity from human foetuses and adults. Biochem J 1980; 188: 475–479.
Carmagnol F, Sinet PM, Rapin J, Jerome H . Glutathione-S-transferase of human red blood cells; assay, values in normal subjects and in two pathological circumstances: hyperbilirubinemia and impaired renal function. Clin Chim Acta 1981; 117: 209–217.
Galli F, Rovidati S, Benedetti S, Buoncristiani U, Covarelli C, Floridi A et al. Overexpression of erythrocyte glutathione-S-transferase in uremia and dialysis. Clin Chem 1999; 45: 1781–1788.
Dessì M, Noce A, Dawood KF, Galli F, Taccone-Gallucci M, Fabrini R et al. Erythrocyte glutathione transferase: a potential new biomarker in chronic kidney diseases which correlates with plasma homocysteine. Amino Acids 2012; 43: 347–354.
NKF-DOQI Clinical practice guidelines for hemodialysis adequacy. Am J Kidney Dis 1997; 30 (suppl 2): S17–S21.
Usberti M, Gerardi GM, Bufano G, Tira P, Micheli A, Albertini A et al. Effects of erythropoietin and vitamin e-modified dialyzers on plasma oxidant stress markers and red blood cell survival. Am J Kidney Dis 2002; 40: 590–599.
Fazi A, Accorsi A, Piatti E, Magnani M . Cell age dependent decay of human erythrocytes glutathione S-transferase. Mech Ageing Dev 1991; 58: 255–266.
Voss FE, Schollum JB, Coulter CV, Doyle TC, Duffull SB, Walker RJ . Red blood cell survival in long-term dialysis patients. Am J Kidney Dis 2011; 58: 591–598.
Lo Bello M, Nuccetelli M, Caccuri AM, Stella L, Parker MW, Rossjohn J et al. Human glutathione transferase P1-1 and nitric oxide carriers: a new role for an old enzyme. J Biol Chem 2001; 276: 42138–42145.
De Maria F, Pedersen JZ, Caccuri AM, Antonini G, Turella P, Stella L et al. The Specific interaction of dinitrosyl-diglutathionyl-iron complex, a natural NO carrier, with the glutathione transferase superfamily: suggestion for an evolutionary pressure in the direction of the storage of nitric oxide. J Biol Chem 2003; 278: 42283–42293.
Paniagua R, Amato D, Vonesh E, Correa-Rotter R, Ramos A, Moran J, Mujais S for the Mexican Nephrology Collaborative Study Group. Effects of increased peritoneal clearances on mortality rates in peritoneal dialysis: ADAMEX, a prospective, randomized, controlled trial. J Am Soc Nephrol 2002; 13: 1307–1320.
Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW et alHemodialysis (HEMO) Study Group. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med 2002; 347: 2010–2019.
Li Z, Lew NL, Lazarus JM, Lowrie EG . Comparing the urea reduction ratio and the urea product as outcome–based measures of hemodialysis dose. Am J Kidney Dis 2000; 35: 598–605.
Locatelli F, Manzoni C, Cavalli A, Di Filippo S . Can convective therapies improve dialysis outcomes? Curr Opin Nephrol Hypertens 2009; 18: 476–480.
Koenig RJ, Peterson CM, Jones RL, Saudek C, Lehrman M, Cerami A . Correlation of glucose regulation and hemoglobin HbA1c in diabetes mellitus. N Engl J Med 1976; 295: 417–420.
Locatelli F, Andrulli S, Memoli B, Maffei C, Del Vecchio L, Aterini S et al. Nutritional-inflammation status and resistance to erythropoietin therapy in haemodialysis patients. Nephrol Dial Tansplant 2006; 21: 991–998.
Daugirdas JT . Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol 1993; 4: 1205–1213.
Simons PC, Vander Jagt DL . Purification of glutathione S-transferases by glutathione-affinity chromatography. Methods Enzymol 1981; 77: 235–237.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ . Protein measurements with the Folin phenol reagent. J Biol Chem 1951; 193: 265–275.
Acknowledgements
We thank Professor Jens Z Pedersen for critical reading of the manuscript and Dr. Erica Del Grosso, Dr. Laura Morici and Dr. Renato Massoud for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Finazzi-Agro′
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Noce, A., Ferrannini, M., Fabrini, R. et al. Erythrocyte glutathione transferase: a new biomarker for hemodialysis adequacy, overcoming the Kt/Vurea dogma?. Cell Death Dis 3, e377 (2012). https://doi.org/10.1038/cddis.2012.112
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2012.112
Keywords
This article is cited by
-
Erythrocyte glutathione transferase in kidney transplantation: a probe for kidney detoxification efficiency
Cell Death & Disease (2018)
-
Is low-protein diet a possible risk factor of malnutrition in chronic kidney disease patients?
Cell Death Discovery (2016)
-
Erythrocyte glutathione transferase: a general probe for chemical contaminations in mammals
Cell Death Discovery (2016)
-
Erythrocyte glutathione transferase in uremic diabetic patients: additional data
Acta Diabetologica (2015)
-
Associations of GSTM1*0 and GSTA1*Agenotypes with the risk of cardiovascular death among hemodialyses patients
BMC Nephrology (2014)