Abstract
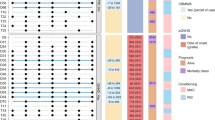
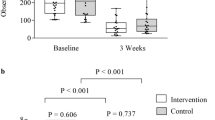
Hematopoietic cell transplantation (HCT) has become a standard treatment for many adult and pediatric conditions. Emerging evidence suggests that perturbations in the microbiota diversity increase recipients’ susceptibilities to gut-mediated conditions such as diarrhea, infection and acute GvHD. Probiotics preserve the microbiota and may minimize the risk of developing a gut-mediated condition; however, their safety has not been evaluated in the setting of HCT. We evaluated the safety and feasibility of the probiotic, Lactobacillus plantarum (LBP), in children and adolescents undergoing allogeneic HCT. Participants received once-daily supplementation with LBP beginning on day −8 or −7 and continued until day +14. Outcomes were compliance with daily administration and incidence of LBP bacteremia. Administration of LBP was feasible with 97% (30/31, 95% confidence interval (CI) 83–100%) of children receiving at least 50% of the probiotic dose (median 97%; range 50–100%). We did not observe any case of LBP bacteremia (0% (0/30) with 95% CI 0–12%). There were not any unexpected adverse events related to LBP. Our study provides preliminary evidence that administration of LBP is safe and feasible in children and adolescents undergoing HCT. Future steps include the conduct of an approved randomized, controlled trial through Children’s Oncology Group.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Mohty B, Mohty M . Long-term complications and side effects after allogeneic hematopoietic stem cell transplantation: an update. Blood Cancer J 2011; 1: e16.
Passweg JR, Halter J, Bucher C, Gerull S, Heim D, Rovo A et al. Hematopoietic stem cell transplantation: a review and recommendations for follow-up care for the general practitioner. Swiss Med Wkly 2012; 142: w13696.
Kamada N, Seo SU, Chen GY, Nunez G . Role of the gut microbiota in immunity and inflammatory disease. Nat Rev Immunol 2013; 13: 321–335.
Holler E, Butzhammer P, Schmid K, Hundsrucker C, Koestler J, Peter K et al. Metagenomic analysis of the stool microbiome in patients receiving allogeneic stem cell transplantation: loss of diversity is associated with use of systemic antibiotics and more pronounced in gastrointestinal graft-versus-host disease. Biol Blood Marrow Transplant 2014; 20: 640–645.
Levinson A, Pinkney K, Jin Z, Bhatia M, Kung AL, Foca MD et al. Acute gastrointestinal graft-vs-host disease is associated with increased enteric bacterial bloodstream infection density in pediatric allogeneic hematopoietic cell transplant recipients. Clin Infect Dis 2015; 61: 350–357.
Taur Y, Jenq RR, Perales MA, Littmann ER, Morjaria S, Ling L et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood 2014; 124: 1174–1182.
Taur Y, Xavier JB, Lipuma L, Ubeda C, Goldberg J, Gobourne A et al. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis 2012; 55: 905–914.
Docampo MD, Auletta JJ, Jenq RR . Emerging influence of the intestinal microbiota during allogeneic hematopoietic cell transplantation: control the gut and the body will follow. Biol Blood Marrow Transplant 2015; 21: 1360–1366.
de Vrese M, Schrezenmeir J . Probiotics, prebiotics, and synbiotics. Adv Biochem Eng Biotechnol 2008; 111: 1–66.
Anukam KC, Osazuwa EO, Osadolor HB, Bruce AW, Reid G . Yogurt containing probiotic Lactobacillus rhamnosus GR-1 and L. reuteri RC-14 helps resolve moderate diarrhea and increases CD4 count in HIV/AIDS patients. J Clin Gastroenterol 2008; 42: 239–243.
Bin-Nun A, Bromiker R, Wilschanski M, Kaplan M, Rudensky B, Caplan M et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight neonates. J Pediatr 2005; 147: 192–196.
Delia P, Sansotta G, Donato V, Frosina P, Messina G, De Renzis C et al. Use of probiotics for prevention of radiation-induced diarrhea. World J Gastroenterol 2007; 13: 912–915.
Hamad A, Fragkos KC, Forbes A . A systematic review and meta-analysis of probiotics for the management of radiation induced bowel disease. Clin Nutr 2013; 32: 353–360.
Honeycutt TC, El Khashab M, Wardrop RM III, McNeal-Trice K, Honeycutt AL, Christy CG et al. Probiotic administration and the incidence of nosocomial infection in pediatric intensive care: a randomized placebo-controlled trial. Pediatr Crit Care Med 2007; 8: 452–458.
Johnston BC, Goldenberg JZ, Vandvik PO, Sun X, Guyatt GH . Probiotics for the prevention of pediatric antibiotic-associated diarrhea. Cochrane Database Syst Rev 2011; 11: CD004827.
Osterlund P, Ruotsalainen T, Korpela R, Saxelin M, Ollus A, Valta P et al. Lactobacillus supplementation for diarrhoea related to chemotherapy of colorectal cancer: a randomised study. Br J Cancer 2007; 97: 1028–1034.
Szajewska H, Ruszczynski M, Radzikowski A . Probiotics in the prevention of antibiotic-associated diarrhea in children: a meta-analysis of randomized controlled trials. J Pediatr 2006; 149: 367–372.
Wolvers D, Antoine JM, Myllyluoma E, Schrezenmeir J, Szajewska H, Rijkers GT . Guidance for substantiating the evidence for beneficial effects of probiotics: prevention and management of infections by probiotics. J Nutr 2010; 140: 698S–712S.
Chapman CM, Gibson GR, Rowland I . Health benefits of probiotics: are mixtures more effective than single strains? Eur J Nutr 2011; 50: 1–17.
Klarin B, Johansson ML, Molin G, Larsson A, Jeppsson B . Adhesion of the probiotic bacterium Lactobacillus plantarum 299v onto the gut mucosa in critically ill patients: a randomised open trial. Crit Care 2005; 9: R285–R293.
McNaught CE, Woodcock NP, MacFie J, Mitchell CJ . A prospective randomised study of the probiotic Lactobacillus plantarum 299V on indices of gut barrier function in elective surgical patients. Gut 2002; 51: 827–831.
Saad N, Urdaci M, Vignoles C, Chaignepain S, Tallon R, Schmitter JM et al. Lactobacillus plantarum 299v surface-bound GAPDH: a new insight into enzyme cell walls location. J Microbiol Biotechnol 2009; 19: 1635–1643.
Wullt M, Johansson Hagslatt ML, Odenholt I, Berggren A . Lactobacillus plantarum 299v enhances the concentrations of fecal short-chain fatty acids in patients with recurrent clostridium difficile-associated diarrhea. Dig Dis Sci 2007; 52: 2082–2086.
Ducrotte P, Sawant P, Jayanthi V . Clinical trial: Lactobacillus plantarum 299v (DSM 9843) improves symptoms of irritable bowel syndrome. World J Gastroenterol 2012; 18: 4012–4018.
Kleerebezem M, Boekhorst J, van Kranenburg R, Molenaar D, Kuipers OP, Leer R et al. Complete genome sequence of Lactobacillus plantarum WCFS1. Proc Natl Acad Sci USA 2003; 100: 1990–1995.
Mangell P, Nejdfors P, Wang M, Ahrne S, Westrom B, Thorlacius H et al. Lactobacillus plantarum 299v inhibits Escherichia coli-induced intestinal permeability. Dig Dis Sci 2002; 47: 511–516.
Klarin B, Wullt M, Palmquist I, Molin G, Larsson A, Jeppsson B . Lactobacillus plantarum 299v reduces colonisation of Clostridium difficile in critically ill patients treated with antibiotics. Acta Anaesthesiol Scand 2008; 52: 1096–1102.
Gerbitz A, Schultz M, Wilke A, Linde HJ, Scholmerich J, Andreesen R et al. Probiotic effects on experimental graft-versus-host disease: let them eat yogurt. Blood 2004; 103: 4365–4367.
Jenq RR, Ubeda C, Taur Y, Menezes CC, Khanin R, Dudakov JA et al. Regulation of intestinal inflammation by microbiota following allogeneic bone marrow transplantation. J. Exp Med 2012; 209: 903–911.
Robin F, Paillard C, Marchandin H, Demeocq F, Bonnet R, Hennequin C . Lactobacillus rhamnosus meningitis following recurrent episodes of bacteremia in a child undergoing allogeneic hematopoietic stem cell transplantation. J Clin Microbiol 2010; 48: 4317–4319.
Mehta A, Rangarajan S, Borate U . A cautionary tale for probiotic use in hematopoietic SCT patients-Lactobacillus acidophilus sepsis in a patient with mantle cell lymphoma undergoing hematopoietic SCT. Bone Marrow Transplant 2013; 48: 461–462.
Van den Nieuwboer M, Brummer RJ, Guarner F, Morelli L, Cabana M, Claassen E . The administration of probiotics and synbiotics in immune compromised adults: is it safe? Benef Microbes 2015; 6: 3–17.
Castagnola E, Faraci M, Moroni C, Bandettini R, Caruso S, Bagnasco F et al. Bacteremias in children receiving hemopoietic SCT. Bone Marrow Transplant 2008; 41: S104–S106.
Castagnola E, Bagnasco F, Faraci M, Caviglia I, Caruso S, Cappelli B et al. Incidence of bacteremias and invasive mycoses in children undergoing allogeneic hematopoietic stem cell transplantation: a single center experience. Bone Marrow Transplant 2008; 41: 339–347.
Busca A, Saroglia EM, Giacchino M, Vai S, Vassallo E, Fagioli F et al. Analysis of early infectious complications in pediatric patients undergoing bone marrow transplantation. Support Care Cancer 1999; 7: 253–259.
Sencer SF, Zhou T, Freedman LS, Ives JA, Chen Z, Wall D et al. Traumeel S in preventing and treating mucositis in young patients undergoing SCT: a report of the Children's Oncology Group. Bone Marrow Transplant 2012; 47: 1409–1414.
Guddati AK, Kumar G, Ahmed S, Ali M, Kumar N, Hari P et al. Incidence and outcomes of Clostridium difficile-associated disease in hematopoietic cell transplant recipients. Int J Hematol 2014; 99: 758–765.
Jacobsohn DA, Vogelsang GB . Acute graft versus host disease. Orphanet J Rare Dis 2007; 2: 35.
Jacobsohn DA . Acute graft-versus-host disease in children. Bone Marrow Transplant 2008; 41: 215–221.
Acknowledgements
We thank the patients, families, physicians, nurses, research coordinators and all others who participated in the data collection for this trial. We also thank Probi AB, Irini Lazou Ahrén and Niklas Larsson for providing LBP and their scientific advice for this trial. This work was supported by the Tamarind Foundation to EJL and the All Children’s Research Foundation Pilot Grant to MN.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ladas, E., Bhatia, M., Chen, L. et al. The safety and feasibility of probiotics in children and adolescents undergoing hematopoietic cell transplantation. Bone Marrow Transplant 51, 262–266 (2016). https://doi.org/10.1038/bmt.2015.275
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2015.275
This article is cited by
-
Probiotic Strain Limosilactobacillus reuteri 29B is Proven Safe and Exhibits Potential Probiotic Traits in a Murine Vaginal Model
Probiotics and Antimicrobial Proteins (2023)
-
Anforderungen an die Infektionsprävention bei der medizinischen Versorgung von immunsupprimierten Patienten
Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz (2021)
-
Safety of Probiotics Among High-Risk Pediatric Hematopoietic Stem Cell Transplant Recipients
Infectious Diseases and Therapy (2019)
-
Intestinal microbiota: a potential target for the treatment of postmenopausal osteoporosis
Bone Research (2017)
-
Gut microbiota and hematopoietic stem cell transplantation: where do we stand?
Bone Marrow Transplantation (2017)