Abstract
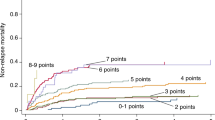
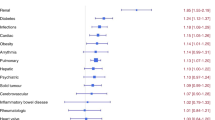
A recent validation analysis at our center among allogeneic hematopoietic cell transplant (HCT) recipients did not find the HCT-specific comorbidity index (HCT-CI) to clearly segregate patient's transplant-related risk. We hypothesized that the discriminating and predictive power of the HCT-CI for mortality could be improved by eliminating the assignment of categorical weights to comorbidities and instead replacing them with hazard ratios (HR) from a Fine and Gray adjusted regression model. This approach allowed us to look carefully at each component of the comorbidity index. We developed the modified comorbidity index (MCI) using a cohort of 444 adult allogeneic HCT recipients using a pure multiplicative model. Compared with low-risk patients, the HR for non-relapse mortality (NRM) using the HCT-CI was 1.3 (95% confidence intervals, 0.7–2.4) for intermediate risk and 1.6 (0.9–2.8) for high-risk patients, and with the MCI was 1.6 (0.9–2.8) and 2.7 (1.5–5.0), respectively. In conclusion, we are introducing the MCI which may have higher discriminating and predictive power for overall survival and NRM. Validation of the HCT-CI and the MCI in larger and separate cohorts of HCT recipients is still needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Sorror ML, Maris MB, Storer B, Sandmaier BM, Diaconescu R, Flowers C et al. Comparing morbidity and mortality of HLA-matched unrelated donor hematopoietic cell transplantation after nonmyeloablative and myeloablative conditioning: influence of pretansplantation comorbidities. Blood 2004; 204: 960–968.
Artz AS, Pollyea DA, Kocherginsky M, Stock W, Rich E, Odenike O et al. Performance status and comorbidity predict transplant-related mortality after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 2006; 12: 954–964.
Alamo J, Shahjahan M, Lazarus HM, de Lima M, Giralt SA . Comorbidity indices in hematopoietic stem cell transplantation: a new report card. Bone Marrow Transplant 2005; 36: 473–474.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, Storer B . Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2911–2919.
Sorror ML, Giralt S, Sandmaier BM, De Lima M, Shahjahan M, Maloney DG, Deeg HJ . Hematopoietic cell transplantation specific comorbidity index as an outcome predictor for patients with acute myeloid leukemia in first remission: combined FHCRC and MDACC experiences. Blood 2007; 110: 4606–4613.
Sorror ML, Sandmaier BM, Storer BE, Maris MB, Baron F, Maloney DG et al. Comorbidity and disease status based risk stratification of outcomes among patients with acute myeloid leukemia or myelodysplasia receiving allogeneic hematopoietic cell transplantation. J Clin Oncol 2007; 25: 4246–4254.
Majhail NS, Brunstein CG, McAvoy S, DeFor TE, Al-Hazzouri A, Setubal D et al. Does the hematopoietic-cell transplantation specific comorbidity index predict transplant outcomes? A validation study in a large cohort of umbilical cord blood and matched related donor transplants. Biol Blood Marrow Transplant 2008; 14: 985–992.
Brunstein CG, Barker JN, Weisdorf DJ, DeFor TE, Miller JS, Blazar BR et al. Umbilical cord blood transplantation after nonmyeloablative conditioning: impact on transplant outcomes in 110 adults with hematological disease. Blood 2007; 8: 3064–3070.
Barker JN, Weisdorf DJ, DeFor TE, Blazar BR, McGlave PB, Miller JS et al. Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood 2005; 105: 1343–1347.
Flynn CM, Hirsch B, Defor T, Barker JN, Miller JS, Wagner JE et al. Reduced intensity compared with high dose conditioning for allo transplantation in acute myeloid leukemia and myelodysplastic syndrome: a comparative clinical analysis. Am J Hematol 2007; 82: 867–872.
Majhail NS, Weisdorf DJ, Wagner JE, Defor TE, Brunstein CG, Burns LJ . Comparable results of umbilical cord blood and HLA-matched sibling donor hematopoietic stem cell transplantation after reduced-intensity preparative regimen for advanced Hodgkin lymphoma. Blood 2006; 107: 3804–3807.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Lin DY . Non-parametric inference for cumulative incidence functions in competing risks studies. Stat Med 1997; 16: 901–910.
Cox DR . Regression models and life tables. J R Stat Soc B 1972; 34: 187–220.
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Harrell FE, Caoliff RM, Pryor DB, Lee LK, Rosati RA . Evaluating the yield of medical tests. J Am Med Assoc 1982; 247: 2543–2546.
Efron E, Tibshirani RJ . An Introduction to the Bootstrap. Chapman & Hall, Inc.: New York, NY, USA, 1993.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
DeFor, T., Majhail, N., Weisdorf, D. et al. A modified comorbidity index for hematopoietic cell transplantation. Bone Marrow Transplant 45, 933–938 (2010). https://doi.org/10.1038/bmt.2009.275
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2009.275
Keywords
This article is cited by
-
Stellenwert der Stammzelltransplantation in der Therapie kutaner T‑Zell-Lymphome
Der Hautarzt (2017)
-
Cutaneous Lymphoma—Inpatient Considerations
Current Dermatology Reports (2017)
-
Up-to-date tools for risk assessment before allogeneic hematopoietic cell transplantation
Bone Marrow Transplantation (2016)
-
Predicting early post-chemotherapy adverse events in patients with hematological malignancies: a retrospective study
Supportive Care in Cancer (2016)
-
Prediction of non-relapse mortality in recipients of reduced intensity conditioning allogeneic stem cell transplantation with AML in first complete remission
Leukemia (2015)