Abstract
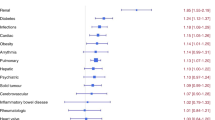
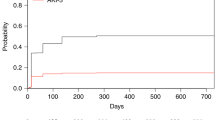
Various complications can influence hematopoietic cell transplantation (HCT) outcomes. Renal complications can occur during the early to late phases of HCT along with various factors. However, studies focusing on fatal renal complications (FRCs) are scarce. Herein, we analyzed 36,596 first allogeneic HCT recipients retrospectively. Overall, 782 patients died of FRCs at a median of 108 (range, 0–3,440) days after HCT. The cumulative incidence of FRCs was 1.7% and 2.2% at one and five years, respectively. FRCs were associated with older age, male sex, non-complete remission (non-CR), lower performance status (PS), and HCT comorbidity index (HCT-CI) associated with renal comorbidity in multivariate analysis. The risk factors within 100 days included older age, multiple myeloma, PS, and HCT-CI comorbidities (psychiatric disturbance, hepatic disease, obesity, and renal disease). Older age and male sex were risk factors between 100 days and one year. After one year, HCT-CI was associated with the presence of diabetes and prior solid tumor; total body irradiation was identified as a risk factor. Non-CR was a common risk factor in all three phases. Furthermore, acute and chronic graft-versus-host disease, reactivation of cytomegalovirus, and relapse of underlying disease also affected FRCs. Systematic follow-up may be necessary based on the patients’ risk factors and post-HCT events.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data of this study are not publicly available due to ethical restrictions that it exceeds the scope of the recipient/donor’s consent for research use in the registry.
References
Gutierrez-Garcia G, Villarreal J, Garrote M, Rovira M, Blasco M, Suarez-Lledo M, et al. Impact of severe acute kidney injury and chronic kidney disease on allogeneic hematopoietic cell transplant recipients: a retrospective single center analysis. Bone Marrow Transpl. 2020;55:1264–1271. https://doi.org/10.1038/s41409-020-0843-3.
Kanduri SR, Cheungpasitporn W, Thongprayoon C, Bathini T, Kovvuru K, Garla V, et al. Incidence and mortality of acute kidney injury in patients undergoing hematopoietic stem cell transplantation: a systematic review and meta-analysis. QJM. 2020;113:621–632. https://doi.org/10.1093/qjmed/hcaa072.
Renaghan AD, Jaimes EA, Malyszko J, Perazella MA, Sprangers B, Rosner MH. Acute kidney injury and CKD associated with hematopoietic stem cell transplantation. Clin J Am Soc Nephrol. 2020;15:289–297. https://doi.org/10.2215/CJN.08580719.
Farhadfar N, Dias A, Wang T, Fretham C, Chhabra S, Murthy HS, et al. Impact of pretransplantation renal dysfunction on outcomes after allogeneic hematopoietic cell transplantation. Transpl Cell Ther. 2021;27:410–422. https://doi.org/10.1016/j.jtct.2021.02.030.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–2919. https://doi.org/10.1182/blood-2005-05-2004.
Wu NL, Hingorani S, Cushing-Haugen KL, Lee SJ, Chow EJ. Late kidney morbidity and mortality in hematopoietic cell transplant survivors. Transpl Cell Ther. 2021;27:434.e431–434.e436. https://doi.org/10.1016/j.jtct.2021.02.013.
Kersting S, Hene RJ, Koomans HA, Verdonck LF. Chronic kidney disease after myeloablative allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2007;13:1169–1175. https://doi.org/10.1016/j.bbmt.2007.06.008.
Miyata M, Ichikawa K, Matsuki E, Watanabe M, Peltier D, Toubai T. Recent advances of acute kidney injury in hematopoietic cell transplantation. Front Immunol. 2021;12:779881 https://doi.org/10.3389/fimmu.2021.779881.
Madsen K, Pelletier K, Cote G, Kitchlu A, Chen S, Mattsson J, et al. Acute kidney injury within 100 days post allogeneic hematopoietic cell transplantation is associated with increased risk of post-transplant complications and poor transplant outcomes. Bone Marrow Transpl. 2022;57:1411–1420. https://doi.org/10.1038/s41409-022-01744-0.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A, et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP System. Int J Hematol. 2007;86:269–274. https://doi.org/10.1532/IJH97.06239.
Atsuta Y. Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol. 2016;103:3–10. https://doi.org/10.1007/s12185-015-1894-x.
Sullivan KM, Agura E, Anasetti C, Appelbaum F, Badger C, Bearman S, et al. Chronic graft-versus-host disease and other late complications of bone marrow transplantation. Semin Hematol. 1991;28:250–259.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–828.
Jagus D, Lis K, Niemczyk L, Basak GW. Kidney dysfunction after hematopoietic cell transplantation-Etiology, management, and perspectives. Hematol Oncol Stem Cell Ther. 2018;11:195–205. https://doi.org/10.1016/j.hemonc.2018.07.004.
Abramson MH, Gutgarts V, Zheng J, Maloy MA, Ruiz JD, Scordo M, et al. Acute kidney injury in the modern era of allogeneic hematopoietic stem cell transplantation. Clin J Am Soc Nephrol. 2021;16:1318–1327. https://doi.org/10.2215/CJN.19801220.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–458. https://doi.org/10.1038/bmt.2012.244.
Ellis MJ, Parikh CR, Inrig JK, Kanbay M, Patel UD. Chronic kidney disease after hematopoietic cell transplantation: a systematic review. Am J Transpl. 2008;8:2378–2390. https://doi.org/10.1111/j.1600-6143.2008.02408.x.
Kagoya Y, Kataoka K, Nannya Y, Kurokawa M. Pretransplant predictors and posttransplant sequels of acute kidney injury after allogeneic stem cell transplantation. Biol Blood Marrow Transpl. 2011;17:394–400. https://doi.org/10.1016/j.bbmt.2010.07.010.
Fuji S, Takano K, Mori T, Eto T, Taniguchi S, Ohashi K, et al. Impact of pretransplant body mass index on the clinical outcome after allogeneic hematopoietic SCT. Bone Marrow Transpl. 2014;49:1505–1512. https://doi.org/10.1038/bmt.2014.178.
Bhatt VR, Wang T, Chen K, Kitko CL, MacMillan ML, Pidala JA, et al. Chronic graft-versus-host disease, nonrelapse mortality, and disease relapse in older versus younger adults undergoing matched allogeneic peripheral blood hematopoietic cell transplantation: a center for international blood and marrow transplant research analysis. Transpl Cell Ther. 2022;28:34–42. https://doi.org/10.1016/j.jtct.2021.10.002.
Guilfoyle R, Demers A, Bredeson C, Richardson E, Rubinger M, Szwajcer D, et al. Performance status, but not the hematopoietic cell transplantation comorbidity index (HCT-CI), predicts mortality at a Canadian transplant center. Bone Marrow Transpl. 2009;43:133–139. https://doi.org/10.1038/bmt.2008.300.
Kurosawa S, Yakushijin K, Yamaguchi T, Atsuta Y, Nagamura-Inoue T, Akiyama H, et al. Recent decrease in non-relapse mortality due to GVHD and infection after allogeneic hematopoietic cell transplantation in non-remission acute leukemia. Bone Marrow Transpl. 2013;48:1198–1204. https://doi.org/10.1038/bmt.2013.42.
Kroger N, Shimoni A, Schilling G, Schwerdtfeger R, Bornhauser M, Nagler A, et al. Unrelated stem cell transplantation after reduced intensity conditioning for patients with multiple myeloma relapsing after autologous transplantation. Br J Haematol. 2010;148:323–331. https://doi.org/10.1111/j.1365-2141.2009.07984.x.
Patriarca F, Einsele H, Spina F, Bruno B, Isola M, Nozzoli C, et al. Allogeneic stem cell transplantation in multiple myeloma relapsed after autograft: a multicenter retrospective study based on donor availability. Biol Blood Marrow Transpl. 2012;18:617–626. https://doi.org/10.1016/j.bbmt.2011.07.026.
Buchbinder D, Khera N. Psychosocial and financial issues after hematopoietic cell transplantation. Hematol Am Soc Hematol Educ Program. 2021;2021:570–577. https://doi.org/10.1182/hematology.2021000292.
Mishkin AD, Shapiro PA, Reshef R, Lopez-Pintado S, Mapara MY. Standardized semi-structured psychosocial evaluation before hematopoietic stem cell transplantation predicts patient adherence to post-transplant regimen. Biol Blood Marrow Transpl. 2019;25:2222–2227. https://doi.org/10.1016/j.bbmt.2019.06.019.
Ferraz FTP, Marra AR, Hamerschlak N, de Souza Durao Junior M. The use of low doses of methotrexate during peri-cell infusion period may be a risk factor for acute kidney injury in patients subjected to hematopoietic stem cell transplantation. Ann Hematol. 2020;99:627–633. https://doi.org/10.1007/s00277-020-03928-4.
Carrero JJ, Hecking M, Chesnaye NC, Jager KJ. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol. 2018;14:151–164. https://doi.org/10.1038/nrneph.2017.181.
Lopes JA, Jorge S, Neves M. Acute kidney injury in HCT: an update. Bone Marrow Transpl. 2016;51:755–762. https://doi.org/10.1038/bmt.2015.357.
Hingorani S. Chronic kidney disease in long-term survivors of hematopoietic cell transplantation: epidemiology, pathogenesis, and treatment. J Am Soc Nephrol. 2006;17:1995–2005. https://doi.org/10.1681/ASN.2006020118.
Jo T, Arai Y, Kondo T, Kitano T, Hishizawa M, Yamashita K, et al. Chronic kidney disease in long-term survivors after allogeneic hematopoietic stem cell transplantation: retrospective analysis at a single institute. Biol Blood Marrow Transpl. 2017;23:2159–2165. https://doi.org/10.1016/j.bbmt.2017.08.016.
Kal HB, van Kempen-Harteveld ML. Renal dysfunction after total body irradiation: dose-effect relationship. Int J Radiat Oncol Biol Phys. 2006;65:1228–1232. https://doi.org/10.1016/j.ijrobp.2006.02.021.
Saddadi F, Hakemi M, Najafi I, Moghadam K, Ghavamzadeh A, Jahani M, et al. Chronic kidney disease after hematopoietic cell transplantation: frequency, risk factors, and outcomes. Transpl Proc. 2009;41:2895–2897. https://doi.org/10.1016/j.transproceed.2009.07.093.
Skinner R, Kaplan R, Nathan PC. Renal and pulmonary late effects of cancer therapy. Semin Oncol. 2013;40:757–773. https://doi.org/10.1053/j.seminoncol.2013.09.009.
Bodge MN, Reddy S, Thompson MS, Savani BN. Preparative regimen dosing for hematopoietic stem cell transplantation in patients with chronic kidney disease: analysis of the literature and recommendations. Biol Blood Marrow Transpl. 2014;20:908–919. https://doi.org/10.1016/j.bbmt.2014.02.013.
Foster GG, Grant MJ, Thomas SM, Cameron B, Raiff D, Corbet K, et al. Treatment with foscarnet after allogeneic hematopoietic cell transplant (Allo-HCT) is associated with long-term loss of renal function. Biol Blood Marrow Transpl. 2020;26:1597–1606. https://doi.org/10.1016/j.bbmt.2020.05.007.
Shorr RI, Longo WL, Oberley TD, Bozdech MJ, Walker DL. Cytomegalovirus-associated tubulointerstitial nephritis in an allogeneic bone marrow transplant recipient. Ann Intern Med. 1987;107:351–352. https://doi.org/10.7326/0003-4819-107-2-351.
Swanson KJ, Djamali A, Jorgenson MR, Misch EA, Ghaffar A, Zhong W, et al. Cytomegalovirus nephritis in kidney transplant recipients: epidemiology and outcomes of an uncommon diagnosis. Transpl Infect Dis. 2021;23:e13702 https://doi.org/10.1111/tid.13702.
Wanchoo R, Stotter BR, Bayer RL, Jhaveri KD. Acute kidney injury in hematopoietic stem cell transplantation. Curr Opin Crit Care. 2019;25:531–538. https://doi.org/10.1097/MCC.0000000000000657.
Chang A, Hingorani S, Kowalewska J, Flowers ME, Aneja T, Smith KD, et al. Spectrum of renal pathology in hematopoietic cell transplantation: a series of 20 patients and review of the literature. Clin J Am Soc Nephrol. 2007;2:1014–1023. https://doi.org/10.2215/CJN.01700407.
Hingorani SR, Seidel K, Lindner A, Aneja T, Schoch G, McDonald G. Albuminuria in hematopoietic cell transplantation patients: prevalence, clinical associations, and impact on survival. Biol Blood Marrow Transpl. 2008;14:1365–1372. https://doi.org/10.1016/j.bbmt.2008.09.015.
Hingorani S, Gooley T, Pao E, Sandmaier B, McDonald G. Urinary cytokines after HCT: evidence for renal inflammation in the pathogenesis of proteinuria and kidney disease. Bone Marrow Transpl. 2014;49:403–409. https://doi.org/10.1038/bmt.2013.197.
Penack O, Peczynski C, Koenecke C, Polge E, Sanderson R, Yakoub-Agha I, et al. Organ complications after CD19 CAR T-cell therapy for large B cell lymphoma: a retrospective study from the EBMT transplant complications and lymphoma working party. Front Immunol. 2023;14:1252811 https://doi.org/10.3389/fimmu.2023.1252811.
Khan I, Khan N, Wolfson N, Djebabria K, Rehman MEU, Anwer F. Safety of CAR-T cell therapy in patients with renal failure/acute kidney injury: focused review. Clin Hematol Int. 2023;5:122–129. https://doi.org/10.1007/s44228-023-00037-7.
Acknowledgements
The authors are grateful to the physicians and data managers at the centers who contributed valuable transplantation data to the JSTCT. We would also like to thank all members of the Transplant Registry Unified Management Committee at the JSTCT for their dedicated data management.
Author information
Authors and Affiliations
Contributions
RY designed the study, analyzed the data, and wrote the manuscript. HK, KY and AS designed the study, provided advice on the methods, and wrote the manuscript. NU, AJ, WT, TN, MT, TE, HO, KI, KM, YKatayama, YKanda, MS, and TK collected data and revised the manuscript. MO and TF collected data, revised the manuscript, and was responsible for data management at the JSTCT. YA managed the unified registry database and revised the manuscript. HN designed the study, advised on the methods, revised the manuscript, and was responsible for the JSTCT Transplantation Complications Working Group. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yanagisawa, R., Koyama, H., Yakushijin, K. et al. Analysis of risk factors for fatal renal complications after allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 59, 325–333 (2024). https://doi.org/10.1038/s41409-023-02172-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02172-4