Abstract
Background:
Breast cancer is a leading cause of cancer death in women. Sleep has been linked with mortality among cancer-free population; however, its association with survival among women with breast cancer is understudied.
Methods:
Breast cancer patients (N=3682) reported their average sleep duration post diagnosis. Subsamples also provided their pre-diagnosis sleep duration (n=1949) and post-diagnosis sleep difficulties (n=1353). Multivariate Cox models estimated hazard ratios (HR) and confidence intervals (CI) of all-cause, breast cancer, and non-breast cancer mortality.
Results:
At diagnosis, the mean age was 64.9 years and 91.7% were stage I or II. Women sleeping ⩾9 h per night post diagnosis had a strong higher risk of all-cause (multivariate HRs: MV-HR=1.37, CI=1.10–1.71), breast cancer (MV-HR=1.46, CI=1.02–2.07), and non-breast cancer mortality (MV-HR=1.34, CI=1.01–1.79), compared to women sleeping 8 h per night. Increased sleep duration post diagnosis (vs unchanged) and regular sleep difficulties (vs rare/none) were associated with a strong elevated risk of all-cause mortality (MV-HRincreased duration=1.35, CI=1.04–1.74; MV-HRregular difficulties=1.49, CI=1.02–2.19) and a moderate greater risk of breast cancer and non-breast cancer mortality.
Conclusions:
Various facets of sleep were associated with higher all-cause mortality risk. If replicated, these findings support evaluation of breast cancer patients’ sleep duration and difficulties to identify those at risk for poorer outcomes.
Similar content being viewed by others
Main
Breast cancer is the most common cancer in women worldwide (Center et al, 2011). In 2016, ∼246 660 new cases and 40 450 deaths occurred in the USA (American Cancer Society, 2016a). Regardless of disease stage and position on the cancer trajectory, from diagnosis, through treatment and survivorship, women with breast cancer are likely to report poor sleep quality, in a higher proportion than what is generally reported among the general population (Savard and Morin, 2001; Fiorentino and Ancoli-Israel, 2006; Colagiuri et al, 2011; Mosher and Duhamel, 2012) and by patients with other cancer sites (Garrett et al, 2011; Savard et al, 2011). Further, they experience shorter sleep duration compared with healthy, age-matched women (Silberfarb et al, 1993; Carpenter et al, 2004; Fiorentino and Ancoli-Israel, 2006). Disrupted sleep among cancer patients may be related to their emotional response to diagnosis and treatment side effects (e.g., pain, fatigue; Savard and Morin, 2001; Trudel-Fitzgerald et al, 2013) and will frequently be reported for several years following diagnosis and treatment (Savard et al, 2011; Zhou and Recklitis, 2014).
There is increasing interest in better understanding the role of sleep in carcinogenesis (Erren et al, 2016). For instance, some studies have suggested that short and long sleep duration are associated with increased cancer incidence (Jiao et al, 2013; Luojus et al, 2014; Xiao et al, 2016), though others have revealed null findings (Sturgeon et al, 2012; Girschik et al, 2013; Vogtmann et al, 2013; Qian et al, 2015) or inverse associations (Sigurdardottir et al, 2012; Zhao et al, 2013). Similarly, the emerging literature on sleep quality (e.g., difficulties falling/staying asleep, early awakening) and cancer risk has been mixed (Kripke et al, 2002; Sigurdardottir et al, 2013; Erren et al, 2015; Fang et al, 2015; Sen et al, 2016). With regard to mortality, self-reported sleep duration (Cappuccio et al, 2010; Shen et al, 2016), changes in sleep duration (Ferrie et al, 2007) and poor sleep quality (Dew et al, 2003) are associated with increased risk of all-cause death among the general population. However, less is known about their role in cancer survival. In a recent research where self-reported sleep characteristics were collected 7.5 years (median) before cancer diagnosis, short sleep duration, alone or combined with frequent snoring, was related to increased breast cancer mortality, whereas sleep quality was unrelated (Phipps et al, 2016). However, given the role of cancer-related factors (e.g., psychological distress, side effects of treatments) in insomnia development (Savard and Morin, 2001) and the sustained high rates of insomnia among breast cancer patients in the first year following diagnosis (Savard et al, 2011), considering the role of sleep characteristics after breast cancer diagnosis in relation to future mortality risk is warranted. Preliminary actigraph data from advanced stage breast cancer patients suggested that poor sleep efficiency assessed up to 7 years post diagnosis was associated with cancer-specific mortality over a 10-year follow-up period (Palesh et al, 2014). Albeit informative, these studies have not considered mortality unrelated to breast cancer, an important outcome on its own. To our knowledge, no prior epidemiological study has examined the extent to which self-reported sleep duration or difficulties assessed the first years following a breast cancer diagnosis, as well as changes in sleep duration from pre- to post diagnosis are related to all-cause, breast cancer and non-breast cancer mortality over up to 30 years of follow-up. Therefore, we investigated these associations in a large cohort of women with non-metastatic breast cancer. Specifically, we hypothesised that shorter and longer sleep duration, increase and decrease in sleep duration, as well as sleep difficulties, would be related to higher mortality risk.
Materials and methods
Participants
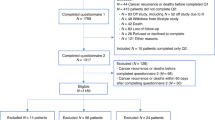
The Nurses’ Health Study comprises 121 700 female nurses who were enroled in 1976 (ages 30–55 years; Willett et al, 1987). They completed biennial questionnaires on demographic characteristics, lifestyle, medical history, and newly diagnosed medical conditions, with a response rate of >85% per questionnaire (Bao et al, 2016). All women who reported having a diagnosis on biennial questionnaires were asked for permission to review their pathology reports and medical records by a study physician to confirm the diagnosis and assess tumour characteristics (e.g., stage). Women who reported their sleep duration within the 4 years following an invasive breast cancer diagnosis (N=3767) were eligible for this study; questions were assessed in 1986, 2000, 2002, and 2008. We excluded participants who reported a cancer before their breast cancer diagnosis (except non-melanoma skin cancer; n=49) or stage IV diagnosis given the low 5-year relative survival (American Cancer Society, 2016b; n=36), yielding an analytic sample of 3682 cases. To explore the association of changes in sleep duration from pre- to post diagnosis with mortality, a subsample of women was identified (n=1949) who completed multiple questionnaires (e.g., 1986 and 2000) assessing sleep and diagnosed with breast cancer between two time points. Another subsample consisted of women who completed the sleep difficulties measure, only queried in 2000, in the 4 years following their diagnosis (n=1353). The study protocol was approved by the institutional review board of the Brigham and Women’s Hospital in Boston, MA, and the human investigations were performed after approval. Informed consent was obtained from all participants.
Measures
To assess average sleep duration, participants were queried about their ‘total hours of actual sleep in a 24-hour period’ with the following responses: ⩽5, 6, 7, 8, 9, 10, or ⩾11 h. In this cohort, self-reported average time spent sleeping has been found highly correlated with sleep duration as assessed by sleep diaries (Spearman r=0.79; P<0.0001) and reproducible over time assessments (sleep duration reported in 2000 and 2002 within a 1 h deviation: Cohen’s κ statistic=0.81; Patel et al, 2004). Because of small numbers, participants who reported ⩽5 or 6 h of sleep were grouped together for the current analyses, as were those with ⩾9 h of sleep. When comparing sleep duration before vs after diagnosis, women were categorised as sleeping either ⩾1 h less (decrease), ⩾1 h more (increase), or no change. Sleep difficulties were assessed using the following question: ‘How much of the time during the past 4 weeks did you have difficulty falling asleep or staying asleep?’, with responses ranging from ‘all of the time’ to ‘none of the time.’ In this study, categories were collapsed to regularly (all or most of the time), occasionally (a good bit or some of the time), and rarely/never (a little or none of the time).
On the basis of similar prior work conducted in this cohort and other samples (Kwan et al, 2013; Patel et al, 2004; Phipps et al, 2016; Xiao et al, 2016), relevant covariates included demographics (marital status (married or in a relationship, divorced, separated, or widowed), highest attained educational level (registered nurse (RN), bachelor, graduate degree), census tract income (continuous, in $)), cancer- and health-related variables (year of diagnosis (continuous), age at diagnosis (continuous), time between date of diagnosis and report of sleep (continuous)), stage (I, II, III), type of surgery (lumpectomy, mastectomy), chemotherapy (yes/no), radiation therapy (yes/no), hormone therapy (yes/no), prevalent diabetes or heart disease (yes/no), hormone use and reproductive history (oral contraceptive use (OC; ever/never), number of pregnancies (continuous), family history of breast cancer (yes/no), menopause status (pre-/postmenopausal), postmenopausal hormone use (PMH, never/past/current user)), and other behavioural variables (body mass index (BMI, kg m−2; ⩽25, 25.1–28.9, ⩾29), alcohol consumption (g per day; ⩽6/>6; Kwan et al, 2013), pack-years of smoking (continuous), caffeine (mg per day; quintiles), calories intake (kcal per day; quintiles), physical activity (metabolic equivalent task, MET-h per week; 3, 3–8.9, 9–14.9, 15–23.9, ⩾24)) (Holmes et al, 2005). For exploratory analyses, a composite binary score of depression was created using a Boolean OR operator approach (Pan et al, 2011) based on self-reported depressive symptoms (Ware and Sherbourne, 1992), physician-diagnosed depression, and antidepressant use whenever these information was available between 1986 and 2008. Cancer-related variables (i.e., year of diagnosis, age at diagnosis, stage, and treatments) were extracted from participants’ medical records. Nurses’ educational level was assessed on the 1992 questionnaire. All other covariates were self-reported on the same questionnaire in which women completed the sleep duration measurement (i.e., within 4 years post diagnosis).
Deaths were reported by next of kin and postal authorities or identified through the National Death Index, leading to 98% mortality follow-up (Rich-Edwards et al, 1994). Physicians ascertained cause of death from death certificates, supplemented as needed by medical records. Underlying cause of death was assigned according to the International Classification of Diseases, Eighth Revision (ICD-8; World Health Organization, 1967).
Statistical analyses
Cox proportional hazards regression models were used to assess the hazard ratios (HR) and 95% confidence intervals (CI) of mortality among breast cancer patients, from date of diagnosis to the end of follow-up (June 2012) or death, whichever came first. The relationship of sleep variables (i.e., post-diagnosis sleep duration, change in sleep duration from pre- to post diagnosis, and post-diagnosis sleep difficulties) with mortality was examined in three sets of nested models. An initial model adjusted for cancer- and health-related variables (listed above). Given that information on cancer treatment was only available for 54.9–66.5% of the analytic sample (N=3682), we also included in this first model a binary missing indicator for each oncologic treatment (yes/no). We then added demographics and hormone-related variables including reproductive history and the fully adjusted model included behaviour-related covariates. To assess the non-linear association of sleep duration and difficulties with mortality outcomes, we calculated P-values for non-linear trend across categories of sleep duration and difficulties, using a quadratic term for the sleep variables. In the models using changes from pre- to post diagnosis as the exposure, we further adjusted for pre-diagnosis sleep duration. Sleep variables were assessed in relation to all-cause death, breast cancer death, and non-breast cancer death as distinct outcomes of interest. Because only one subtype of death could occur for each participant (i.e., breast cancer vs non-breast cancer death), a competing risks framework was also used (Wang et al, 2016): using the cause-specific proportional hazards models, we tested for heterogeneity to assess whether the associations of sleep with both breast cancer and non-breast cancer death were statistically different. Kaplan–Meier curves were also implemented to depict the relation of sleep duration categories with all-cause, breast cancer, and non-breast cancer mortality.
Stratified analyses explored potential effect modifiers of the association between sleep duration and mortality and the likelihood ratio tests were performed, when relevant, to verify statistical significance. Specifically, stratification by age at diagnosis (n>65 years=1736 vs n⩽65 years=1946), as well as post-diagnosis physical activity levels (using the median; n⩽8.5 MET-h per week=1843 vs n>8.5 MET-h per week=1839), snoring (nnever to occasionally=2061 vs na few nights per week to every night=1208), and depression status (ndepressed=559 vs nnon-depressed=2319) was examined. In the subsample of women who completed both the sleep duration and sleep difficulties item in 2000 (n=1353), models using sleep duration as the exposure were stratified by sleep difficulties (nregularly/occasionally=550 vs nrarely/never=803) given prior work suggesting an interaction effect on health-related outcomes (Carroll et al, 2015).
In distinct sensitivity analyses we excluded: (1) women diagnosed 1 and 2 year(s), before the sleep assessment, separately, to minimise effects of various oncologic treatments on sleep (n1-year lag=1126; n2-year lag=1971); (2) women who died 1 year following the sleep assessment to adjust for advanced disease that could impact sleep and survival and to account for reverse causation (i.e., undiagnosed morbidity/advanced disease might influence sleep subsequently and also directly affect mortality; n=77); (3) women categorised as depressed (n=559). Additional sensitivity analyses adjusted for sleep difficulties in models using sleep duration as the exposure and vice versa; supplemental models were further adjusted for prior history of shift work (Lin et al, 2015), snoring (Phipps et al, 2016), and sleep/anxiety medication (Kripke et al, 2002). Because results from all sensitivity analyses were largely similar to our main analyses, for the sake of parsimony only the main models are presented here. All analyses were conducted using SAS software version 9.4 (Cary, NC, USA) with a two-sided P-value of 0.05.
Results
At the time of diagnosis, women were on average 64.9 years old (s.d.=9.3) and almost all (88.3%) postmenopausal. At the time of sleep measure completion (on average 1.7-year post diagnosis, s.d.=1.1), the majority were married (73.2%), had an RN degree as their highest attained educational level (72.8%), and few reported diagnoses of diabetes or heart disease (13.3%). Nearly a quarter reported a family history of breast cancer (22.6%), and most had an early stage cancer (stages I or II: 91.7%). The distribution of variables across sleep duration categories is presented in Table 1.
Among the complete sample of 3682 women, there were 976 deaths, including 412 breast cancer and 564 non-breast cancer deaths, over the follow-up period (median 11 years between diagnosis and death). Compared to women who reported sleeping 8 h per night on average, those who slept ⩾9 h had a strong higher risk of all-cause (HR=1.45, CI=1.16–1.80), breast cancer (HR=1.49, CI=1.05–2.10), and non-breast cancer mortality (HR=1.40, CI=1.05–1.87) in the initial models adjusting for cancer- and health-related variables (Table 2). The strength of the relationship was fairly robust to the inclusion of demographics, hormone-, and behaviour-related variables in the multivariate models (MV-HRall-cause=1.37, CI=1.10–1.71 (Figure 1); MV-HRbreast cancer=1.46, CI=1.02–2.07 (Supplementary Figure 1); MV-HRnon-breast cancer=1.34, CI=1.01–1.79 (Supplementary Figure 2). No statistical association was observed between the other sleep duration categories and any cause of mortality (Table 2), although the estimates mirrored a U-shaped association with shorter sleep duration being associated with a small elevated risk of mortality. Accordingly, the P-values for the test of non-linearity were statistically or marginally significant in all fully adjusted models (P⩽0.12).
Table 3 displays the associations between change in sleep duration from pre- to post diagnosis and mortality (n=1949; 381 all-cause, 132 breast cancer, 249 non-breast cancer deaths). Women whose sleep duration increased after diagnosis were at a strong greater risk of all-cause mortality (MV-HR=1.35, CI=1.04–1.74) than those who reported no change. Breast cancer and non-breast cancer death were associated with sleep duration increases with a similar magnitude (MV-HRbreastcancer=1.29, CI=0.84–2.00; MV-HRnon-breastcancer=1.32, CI=0.96–1.82; competing risk analyses, P=0.97), but power was more limited. Compared to women who reported no change, those with at least 1 h decrease in sleep duration did not clearly exhibit a greater mortality risk, except for non-breast cancer mortality (MV-HRall-cause=1.26, CI=0.97–1.65; MV-HRbreast cancer=0.89, CI=0.55–1.45; MV-HRnon-breast cancer=1.42, CI=1.02–1.96; competing risk analyses, P=0.09).
The relationship of sleep difficulties with mortality was only strong for all-cause deaths in the subsample of 1353 participants (Table 4; 366 all-cause, 119 breast cancer, and 247 non-breast cancer deaths). Specifically, compared to women who reported rare or no sleep difficulties, those who regularly struggled falling or staying asleep had a greater all-cause mortality risk (MV-HR=1.49, CI=1.02–2.19). Although breast cancer death was suggestively related to experiencing regular sleep difficulties (MV-HR=1.78, CI=0.94–3.36), non-breast cancer death was not associated (MV-HR=1.38, CI=0.85–2.26) and these two associations were not statistically different (competing risk analyses, P=0.68). No associations were noted between occasional sleep difficulties and mortality, and none of the P-values for non-linear trend were statistically significant (Table 4).
Stratified analyses revealed that neither age at diagnosis, nor levels of physical activity or snoring post diagnosis were effect modifiers of the association between sleep duration and mortality; null results were also noted for the interaction of sleep difficulties with sleep duration (results not shown). However, among women with post-diagnosis depression status information (n=2878), differences emerged among short sleepers: those with ⩽6 h of sleep per night who were non-depressed post diagnosis (n=2319; 152 breast cancer deaths) had a strong reduced breast cancer mortality risk (MV-HRnon-depressed=0.48, CI=0.30–0.76), whereas those who were depressed (n=559; 48 breast cancer deaths) had a suggestively higher risk (MV-HRdepressed=2.30, CI=0.99–5.31, Pinteraction<0.01), compared to their respective counterparts who slept 8 h per night. The impact of depression status was only observed with breast cancer death for women who slept ⩽6 h per night; no statistical interaction effects were found for sleep duration of 7 or 9 h, nor other causes of death.
Discussion
We found that women with breast cancer who sleep at least 9 h have a 37, 46, and 34% greater risk of all-cause, breast cancer, and non-breast cancer mortality, respectively, than those who sleep 8 h; no associations were observed for sleep durations <8 h. An increase in sleep duration from pre- to post diagnosis, compared to no change, was associated with a 35% higher risk of all-cause death. Furthermore, women who reported regular sleep difficulties had a 49% increased risk of all-cause mortality, compared to women without such frequent difficulties.
Overall, research has been inconsistent in relating sleep with incident breast cancer and very limited as it relates to breast cancer survival. The increased mortality observed among long sleepers is consistent with recent meta-analyses that demonstrated an association between sleep duration, and all-cause and cardiovascular death in the general population (Cappuccio et al, 2010; Shen et al, 2016). However, the elevated breast cancer mortality risk for longer duration (⩾9 h) is particularly novel. Various mechanisms of the long sleep duration–mortality relationship have been proposed, including sleep fragmentation, lack of physiological challenge (e.g., exercise), depression, and underlying disease processes (e.g., sleep apnoea, heart disease; Grandner and Drummond, 2007). Several of these mechanistic factors may actually serve as confounders/effect modifiers (e.g., depression, sleep apnoea, fatigue) rather than being true mediators (e.g., lack of physiological challenge, shortened photoperiod) (Stamatakis and Punjabi, 2007). In the current study, sleep fragmentation was indirectly assessed by adjusting for sleep difficulties in sensitivity analyses, whereas physical activity and prevalent diabetes/heart disease, and snoring (as a proxy for sleep apnoea) were considered as confounders and effect modifiers. Further models stratified by depression status post diagnosis and sensitivity analyses excluded women who were depressed when the sleep measures were queried. Thus, the robustness of our findings for all mortality outcomes supports the possible role of long sleep duration on mortality among breast cancer patients. Despite adjustment for health behaviours and cancer-related factors, which tended to be less favourable among women of this sample reporting ⩾9 h per night compared to their counterparts (e.g., greater alcohol intake, lower proportion of ER+ or PR+ receptors), long sleep could duration could still reflect an underlying health condition. Nonetheless, by corroborating results obtained from non-cancer/healthier populations, these results are consistent with prior literature suggesting that the mechanism of elevated risk among long sleepers is not limited to a single organ system or condition; rather it may impair health function globally (Kripke et al, 2002; Patel et al, 2004).
Short sleep duration was not statistically associated with all mortality outcomes in the overall sample, although the estimates mirrored the U-shaped association that has been observed among varied populations (Cappuccio et al, 2010; Shen et al, 2016) and additional trend analyses suggested such non-linear association. Unlike recent work (Phipps et al, 2016), snoring did not alter the relationship of short sleep duration with mortality, which could be related to the timing of assessment (pre- vs post-cancer diagnosis). However, a strong relationship for short sleep was noted among non-depressed vs depressed women. Of note, the number of deaths per level of sleep duration was relatively small in these stratified analyses (models with depressed women: ndeaths=8–36), leading to less stable estimates with wider CIs. Hence, the moderating impact of depression in the relationship of sleep duration with mortality should be interpreted cautiously and warrants replication. Moreover, increased sleep duration from pre- to post diagnosis was associated with 38% elevated all-cause mortality risk. Such additional hours of sleep, regardless of pre-diagnosis sleep duration, may reflect the patient’s psychological and/or physiological response to the cancer diagnosis and treatments. For instance, fatigue is a common side effect of cancer treatment, thus patients are often told to rest in order to recuperate (Ancoli-Israel et al, 2001). Although napping seems beneficial in the short term, such behaviour may disrupt the sleep-wake schedule over time and serve as a precipitating factor for the development of insomnia (Savard and Morin, 2001; Trudel-Fitzgerald et al, 2013), a sleep disorder that may continue to impact health function well after the patient has ended treatment (Zhou and Recklitis, 2014).
One of the most commonly reported complaints in oncology is poor sleep quality, seen in up to 70% of non-metastatic breast cancer patients within the first months following diagnosis (Fiorentino and Ancoli-Israel, 2006; Savard et al, 2011; Palesh et al, 2013). Chronically poor sleep may influence cancer outcomes through impaired immune function (Sephton and Spiegel, 2003; Lange et al, 2010), metabolic pathways leading to obesity (Mullington et al, 2009; Buxton et al, 2012), and altered melatonin release (Blask, 2009). The current results identified a statistically higher risk of all-cause mortality in women reporting regular sleep difficulties compared to those who reported little or none. These novel findings suggest that beyond sleep duration, sleep difficulties should be considered to fully understand how patients’ health may be impacted. Two previous prospective cohort studies documented no association between sleep quality and breast cancer incidence (Girschik et al, 2013; Vogtmann et al, 2013), whereas recent work suggested that experiencing several, but not single, insomnia symptoms was related to increased risk (Sen et al, 2016). As deficient sleep- and age-related physical declines are often intertwined (Zee and Turek, 2006), poor sleep may exacerbate underlying diseases processes leading to worse health outcomes in breast cancer patients, whereas cancer-free individuals may not be affected to the same extent.
The current study has some limitations. First, because the assessment of sleep variables was self-reported, and the study design is observational, it is impossible to conclude whether sleep duration and difficulties are causally related to future mortality risk in breast cancer patients (Stamatakis and Punjabi, 2007; Kurina et al, 2013). The relationship might also be bidirectional, where declining health may foster longer sleep, as the individual is less able/willing to get out of bed (Grandner and Drummond, 2007). However, our sample did not encompass stage IV cancer cases and our main results were largely unchanged in the sensitivity analyses addressing reverse causation, thus lowering the likelihood of this issue. Next, the majority of the sample were Non-Hispanic White of similar socioeconomic status, limiting the generalisability of the results. Furthermore, using missing indicators for each oncologic treatment may yield biased estimates, although models without such indicators suggested similar increased risk among the subset of women with treatment information. Finally, additional confounders/mediators (e.g., sleep apnoea, altered immune functioning, shortened light exposure, fatigue; Grandner and Drummond, 2007) were not available for these analyses, but should be considered in future work.
To our knowledge, this is the first prospective study to explore the effects of self-reported sleep duration, changes in sleep duration from pre- to post diagnosis, and sleep difficulties, all assessed within 4 years after diagnosis (mean of 1.7-year post diagnosis), on future mortality risk in non-metastatic breast cancer patients. This novel research conducted among a large sample of women using a prospective design with up to 30 years of follow-up suggests that longer sleep duration (⩾9 h), increased sleep duration from pre- to post diagnosis, and sleep difficulties are associated with all-cause mortality. From a research perspective, the mechanisms underscoring these associations should be explored. If these results are replicated in future work, it will be important to evaluate breast cancer patients for long and changing sleep duration, in addition to sleep difficulties in the clinical setting, to identify patients who may be at risk for poor outcomes.
Change history
25 April 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
American Cancer Society (2016a) Cancer Facts & Figures 2016. American Cancer Society: Atlanta.
American Cancer Society (2016b) Learn about Cancer: Breast Cancer. American Cancer Society.
Ancoli-Israel S, Moore PJ, Jones V (2001) The relationship between fatigue and sleep in cancer patients: a review. Eur J Cancer Care (Engl) 10: 245–255.
Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, Chavarro JE (2016) Origin, methods, and evolution of the three Nurses' Health Studies. Am J Public Health 106: 1573–1581.
Blask DE (2009) Melatonin, sleep disturbance and cancer risk. Sleep Med Rev 13: 257–264.
Buxton OM, Cain SW, O'connor SP, Porter JH, Duffy JF, Wang W, Czeisler CA, Shea SA (2012) Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med 4: 129ra43.
Cappuccio FP, D'elia L, Strazzullo P, Miller MA (2010) Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep 33: 585–592.
Carpenter JS, Elam JL, Ridner SH, Carney PH, Cherry GJ, Cucullu HL (2004) Sleep, fatigue, and depressive symptoms in breast cancer survivors and matched healthy women experiencing hot flashes. Oncol Nurs Forum 31: 591–5598.
Carroll JE, Irwin MR, Stein Merkin S, Seeman TE (2015) Sleep and multisystem biological risk: a population-based study. PLoS One 10: e0118467.
Center M, Siegel R, Jemal A (2011) Global Cancer Facts & Figures. American Cancer Society: Atlanta. 1–52.
Colagiuri B, Christensen S, Jensen AB, Price MA, Butow PN, Zachariae R (2011) Prevalence and predictors of sleep difficulty in a national cohort of women with primary breast cancer three to four months postsurgery. J Pain Symptom Manage 42: 710–720.
Dew MA, Hoch CC, Buysse DJ, Monk TH, Begley AE, Houck PR, Hall M, Kupfer DJ, Reynolds CF 3rd (2003) Healthy older adults' sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med 65: 63–73.
Erren TC, Morfeld P, Foster RG, Reiter RJ, Gross JV, Westermann IK (2016) Sleep and cancer: synthesis of experimental data and meta-analyses of cancer incidence among some 1 500 000 study individuals in 13 countries. Chronobiol Int 33: 325–350.
Erren TC, Slanger TE, Gross JV, Reiter RJ (2015) Melatonin, sleep, and prostate cancer in elderly men: study, hypothesis development, and Icelandic options. Eur Urol 67: 195–197.
Fang HF, Miao NF, Chen CD, Sithole T, Chung MH (2015) Risk of cancer in patients with insomnia, parasomnia, and obstructive sleep apnea: a nationwide nested case-control study. J Cancer 6: 1140–1147.
Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, Marmot MG (2007) A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep 30: 1659–1666.
Fiorentino L, Ancoli-Israel S (2006) Insomnia and its treatment in women with breast cancer. Sleep Med Rev 10: 419–429.
Garrett K, Dhruva A, Koetters T, West C, Paul SM, Dunn LB, Aouizerat BE, Cooper BA, Dodd M, Lee K, Wara W, Swift P, Miaskowski C (2011) Differences in sleep disturbance and fatigue between patients with breast and prostate cancer at the initiation of radiation therapy. J Pain Symptom Manage 42: 239–250.
Girschik J, Heyworth J, Fritschi L (2013) Self-reported sleep duration, sleep quality, and breast cancer risk in a population-based case-control study. Am J Epidemiol 177: 316–327.
Grandner MA, Drummond SP (2007) Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med Rev 11: 341–360.
Holmes MD, Chen WY, Feskanich D, Kroenke CH, Colditz GA (2005) Physical activity and survival after breast cancer diagnosis. JAMA 293: 2479–2486.
Jiao L, Duan Z, Sangi-Haghpeykar H, Hale L, White DL, El-Serag HB (2013) Sleep duration and incidence of colorectal cancer in postmenopausal women. Br J Cancer 108: 213–221.
Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR (2002) Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 59: 131–136.
Kurina LM, Mcclintock MK, Chen JH, Waite LJ, Thisted RA, Lauderdale DS (2013) Sleep duration and all-cause mortality: a critical review of measurement and associations. Ann Epidemiol 23: 361–370.
Kwan ML, Chen WY, Flatt SW, Weltzien EK, Nechuta SJ, Poole EM, Holmes MD, Patterson RE, Shu XO, Pierce JP, Caan BJ (2013) Postdiagnosis alcohol consumption and breast cancer prognosis in the after breast cancer pooling project. Cancer Epidemiol Biomarkers Prev 22: 32–41.
Lange T, Dimitrov S, Born J (2010) Effects of sleep and circadian rhythm on the human immune system. Ann NY Acad Sci 1193: 48–59.
Lin X, Chen W, Wei F, Ying M, Wei W, Xie X (2015) Night-shift work increases morbidity of breast cancer and all-cause mortality: a meta-analysis of 16 prospective cohort studies. Sleep Med 16: 1381–1387.
Luojus MK, Lehto SM, Tolmunen T, Erkkila AT, Kauhanen J (2014) Sleep duration and incidence of lung cancer in ageing men. BMC Public Health 14: 295.
Mosher CE, Duhamel KN (2012) An examination of distress, sleep, and fatigue in metastatic breast cancer patients. Psychooncology 21: 100–107.
Mullington JM, Haack M, Toth M, Serrador JM, Meier-Ewert HK (2009) Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. Prog Cardiovasc Dis 51: 294–302.
Palesh O, Aldridge-Gerry A, Ulusakarya A, Ortiz-Tudela E, Capuron L, Innominato PF (2013) Sleep disruption in breast cancer patients and survivors. J Natl Compr Canc Netw 11: 1523–1530.
Palesh O, Aldridge-Gerry A, Zeitzer JM, Koopman C, Neri E, Giese-Davis J, Jo B, Kraemer H, Nouriani B, Spiegel D (2014) Actigraphy-measured sleep disruption as a predictor of survival among women with advanced breast cancer. Sleep 37: 837–842.
Pan A, Okereke OI, Sun Q, Logroscino G, Manson JE, Willett WC, Ascherio A, Hu FB, Rexrode KM (2011) Depression and incident stroke in women. Stroke 42: 2770–2775.
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB (2004) A prospective study of sleep duration and mortality risk in women. Sleep 27: 440–444.
Phipps AI, Bhatti P, Neuhouser ML, Chen C, Crane TE, Kroenke CH, Ochs-Balcom H, Rissling M, Snively BM, Stefanick ML, Treggiari MM, Watson NF (2016) Pre-diagnostic sleep duration and sleep quality in relation to subsequent cancer survival. J Clin Sleep Med 12: 495–503.
Qian X, Brinton LA, Schairer C, Matthews CE (2015) Sleep duration and breast cancer risk in the Breast Cancer Detection Demonstration Project follow-up cohort. Br J Cancer 112: 567–571.
Rich-Edwards JW, Corsano KA, Stampfer MJ (1994) Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol 140: 1016–1019.
Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM (2011) Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. J Clin Oncol 29: 3580–3586.
Savard J, Morin CM (2001) Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol 19: 895–908.
Sen A, Opdahl S, Strand LB, Vatten LJ, Laugsand LE, Janszky I (2016) Insomnia and the risk of breast cancer: the HUNT study. Psychosom Med e-pub ahead of print 19 October 2016 doi:10.1097/PSY.0000000000000417.
Sephton S, Spiegel D (2003) Circadian disruption in cancer: a neuroendocrine-immune pathway from stress to disease? Brain Behav Immun 17: 321–328.
Shen X, Wu Y, Zhang D (2016) Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Sci Rep 6: 21480.
Sigurdardottir LG, Valdimarsdottir UA, Fall K, Rider JR, Lockley SW, Schernhammer E, Mucci LA (2012) Circadian disruption, sleep loss, and prostate cancer risk: a systematic review of epidemiologic studies. Cancer Epidemiol Biomarkers Prev 21: 1002–1011.
Sigurdardottir LG, Valdimarsdottir UA, Mucci LA, Fall K, Rider JR, Schernhammer E, Czeisler CA, Launer L, Harris T, Stampfer MJ, Gudnason V, Lockley SW (2013) Sleep disruption among older men and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev 22: 872–879.
Silberfarb PM, Hauri PJ, Oxman TE, Schnurr P (1993) Assessment of sleep in patients with lung cancer and breast cancer. J Clin Oncol 11: 997–1004.
Stamatakis KA, Punjabi NM (2007) Long sleep duration: a risk to health or a marker of risk? Sleep Med Rev 11: 337–339.
Sturgeon SR, Luisi N, Balasubramanian R, Reeves KW (2012) Sleep duration and endometrial cancer risk. Cancer Causes Control 23: 547–553.
Trudel-Fitzgerald C, Savard J, Ivers H (2013) Which symptoms come first? Exploration of temporal relationships between cancer-related symptoms over an 18-month period. Ann Behav Med 45: 329–337.
Vogtmann E, Levitan EB, Hale L, Shikany JM, Shah NA, Endeshaw Y, Lewis CE, Manson JE, Chlebowski RT (2013) Association between sleep and breast cancer incidence among postmenopausal women in the Women's Health Initiative. Sleep 36: 1437–1444.
Wang M, Spiegelman D, Kuchiba A, Lochhead P, Kim S, Chan AT, Poole EM, Tamimi R, Tworoger SS, Giovannucci E, Rosner B, Ogino S (2016) Statistical methods for studying disease subtype heterogeneity. Stat Med 35: 782–800.
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30: 473–483.
Willett WC, Green A, Stampfer MJ, Speizer FE, Colditz GA, Rosner B, Monson RR, Stason W, Hennekens CH (1987) Relative and absolute excess risks of coronary heart disease among women who smoke cigarettes. N Engl J Med 317: 1303–1309.
World Health Organization (1967) International Statistical Classification of Diseases, Injuries, and Causes of Death, Eighth Revision. Geneva.
Xiao Q, Signorello LB, Brinton LA, Cohen SS, Blot WJ, Matthews CE (2016) Sleep duration and breast cancer risk among black and white women. Sleep Med 20: 25–29.
Zee PC, Turek FW (2006) Sleep and health: everywhere and in both directions. Arch Intern Med 166: 1686–1688.
Zhao H, Yin JY, Yang WS, Qin Q, Li TT, Shi Y, Deng Q, Wei S, Liu L, Wang X, Nie SF (2013) Sleep duration and cancer risk: a systematic review and meta-analysis of prospective studies. Asian Pac J Cancer Prev 14: 7509–7515.
Zhou ES, Recklitis CJ (2014) Insomnia in adult survivors of childhood cancer: a report from project REACH. Support Care Cancer 22: 3061–3069.
Acknowledgements
We would like to thank the participants and the staff of the Nurses' Health Study for their valuable contributions as well as the following American state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, WY. The Nurses’ Health Study is supported by grants UM1 CA186107 and P01 CA87969 by the National Institute of Health. CTF received a postdoctoral fellowship from the Canadian Institutes of Health Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors assume full responsibility for analyses and interpretation of these data.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Trudel-Fitzgerald, C., Zhou, E., Poole, E. et al. Sleep and survival among women with breast cancer: 30 years of follow-up within the Nurses’ Health Study. Br J Cancer 116, 1239–1246 (2017). https://doi.org/10.1038/bjc.2017.85
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.85
Keywords
This article is cited by
-
A scoping review of web-based, interactive, personalized decision-making tools available to support breast cancer treatment and survivorship care
Journal of Cancer Survivorship (2024)
-
Sleep duration and mortality among breast cancer survivors in the Western New York Exposures and Breast Cancer (WEB) Study
Cancer Causes & Control (2024)
-
Sleep and cancer recurrence and survival in patients with resected Stage III colon cancer: findings from CALGB/SWOG 80702 (Alliance)
British Journal of Cancer (2023)
-
Circadian rhythm disrupting behaviours and cancer outcomes in breast cancer survivors: a systematic review
Breast Cancer Research and Treatment (2023)
-
Sleep disturbance in adults with untreated primary brain tumors: prevalence and impact on quality of life
Sleep and Biological Rhythms (2023)