Abstract
Background:
Dinaciclib is a potent inhibitor of cell cycle and transcriptional cyclin-dependent kinases. This Phase 1 study evaluated the safety, tolerability and pharmacokinetics of various dosing schedules of dinaciclib in advanced solid tumour patients and assessed pharmacodynamic and preliminary anti-tumour activity.
Methods:
In part 1, patients were enrolled in escalating cohorts of 2-h infusions administered once every 3 weeks, utilising an accelerated titration design until a recommended phase 2 dose (RP2D) was defined. In part 2, 8- and 24-h infusions were evaluated. Pharmacokinetic parameters were determined for all schedules. Pharmacodynamic effects were assessed with an ex vivo stimulated lymphocyte proliferation assay performed in whole blood.
Effects of dinaciclib on retinoblastoma (Rb) phosphorylation and other CDK targets were evaluated in skin and tumour biopsies. In addition to tumour size, metabolic response was evaluated by 18F-fluorodeoxyglucose-positron emission tomography.
Results:
Sixty-one patients were enrolled to parts 1 and 2. The RP2Ds were 50, 7.4 and 10.4 mg m−2 as 2- 8- and 24-hour infusions, respectively. Dose-limiting toxicities included pancytopenia, neutropenic fever, elevated transaminases, hyperuricemia and hypotension. Pharmacokinetics demonstrated rapid distribution and a short plasma half-life. Dinaciclib suppressed proliferation of stimulated lymphocytes. In skin and tumour biopsies, dinaciclib reduced Rb phosphorylation at CDK2 phospho-sites and modulated expression of cyclin D1 and p53, suggestive of CDK9 inhibition. Although there were no RECIST responses, eight patients had prolonged stable disease and received between 6 and 30 cycles. Early metabolic responses occurred.
Conclusions:
Dinaciclib is tolerable at doses demonstrating target engagement in surrogate and tumour tissue.
Similar content being viewed by others
Main
Cyclin-dependent kinases (CDKs) are critical regulators of cell cycle progression and RNA transcription (Malumbres, 2014). Cyclin-dependent kinases 4, 6, 2 and 1 are core components of the cell cycle machinery and govern the transition between cell cycle phases. Cyclin D-CDK4/6 complexes and cyclin E-CDK2 complexes sequentially phosphorylate the retinoblastoma protein (Rb) to achieve G1 progression and the G1/S transition. Cyclin A-CDK2 and cyclin B-CDK1 complexes control S/G2 and M phase progression, respectively (Shapiro, 2006). Other family members, including CDKs 7, 9 and 12, phosphorylate the C-terminal domain (CTD) of RNA polymerase II and regulate transcriptional initiation, elongation and processing (Eick and Geyer, 2013). CDK5 has been primarily associated with neuronal function (Kawauchi, 2014), but has also been shown to regulate RAS-RAL signalling (Feldmann et al, 2010). The universal dysregulation of CDK activity in human cancer has supported longstanding interest in the development of CDK inhibitors as antineoplastic agents (Malumbres and Barbacid, 2009). Compounds currently in development fall into two classes: (1) selective inhibitors of the G1 CDKs 4 and 6 (Sherr et al, 2016); and (2) less selective inhibitors that target CDKs 1 and 2, as well as the transcriptional CDKs and/or CDK5 (Asghar et al, 2015).
Dinaciclib (MK-7965, formerly SCH727965) is a novel, potent, small-molecule inhibitor of CDKs that has been shown to inhibit CDK2, CDK5, CDK1, CDK9 with 50% inhibitory concentration (IC50) values of 1, 1, 3, and 4 nmol l−1, respectively, in biochemical assays (Parry et al, 2010; Paruch et al, 2010). Recently, CDK12 inhibition by dinaciclib has also been demonstrated (Johnson et al, 2016). In multiple tumour cell lines, dinaciclib suppresses Rb phosphorylation and bromodeoxyuridine (BrdU) incorporation, consistent with inhibition of cell cycle progression (Parry et al, 2010; Feldmann et al, 2011; Fu et al, 2011). These effects are associated with apoptosis by a variety of mechanisms, including cell cycle disruption via combined inhibition of CDKs 1 and 2 (Cai et al, 2006), effects on the expression and stability of the anti-apoptotic protein MCL1 via inhibition of CDKs 9 and 2 (Booher et al, 2014; Choudhary et al, 2015; Gregory et al, 2015), and in the case of melanoma cells, on modulation of wild-type p53 function via inhibition of CDK9 (Desai et al, 2013). Additionally, in in vitro experiments, dinaciclib produces prolonged cellular effects evident at 24 h that have been observed even after short 2-h exposures (Parry et al, 2010).
In vivo, dinaciclib has produced tumour growth inhibition and regression in xenograft models of diverse origin, using both continuous and intermittent schedules at doses below the maximally tolerated level. Efficacy in these models was associated with modulation of Rb phosphorylation in skin, as well as reversible, mechanism-based effects on hematologic parameters (Parry et al, 2010). In addition to bone marrow, preclinical toxicology studies also demonstrated findings in the gastrointestinal tract and lymphoid system, consistent with effects on cellular proliferation.
Here, we report results from a phase 1 study that was designed to determine the safety and tolerability of dinaciclib administered as a 2-, 8-, or 24-h intravenous (i.v.) infusion once every 3 weeks. This intermittent schedule was chosen based on the propensity for apoptotic effects in vitro and tumour regressions in vivo with brief, intermittent exposures, and on the anticipated rest period required for recovery from anti-proliferative toxicities. The study also evaluated pharmacokinetics (PK) and pharmacodynamics (PD), as well as evidence of anti-tumour activity in patients with advanced malignancies.
Materials and Methods
Study design
This was a three-part phase 1 trial evaluating dinaciclib administered intravenously every 3 weeks (NCT00871910;P04630). Part 1 (2-h infusions) and part 2 (8- and 24-h infusions) were nonrandomised, open-label, dose-escalation studies of dinaciclib using an accelerated titration design (Simon et al, 1997). Primary objectives were to evaluate the safety and tolerability, including the maximum administered dose (MAD) and dose-limiting toxicities (DLTs), as well as the pharmacodynamic effects of dinaciclib in an ex vivo lymphocyte stimulation assay (Nemunaitis et al, 2013). Secondary objectives were to determine the PK of single doses of dinaciclib, assess Rb protein phosphorylation in skin and/or tumour biopsies, and to evaluate tumour metabolic changes and preliminary evidence of anti-tumour activity. Part 3 was previously reported and determined that dinaciclib may be safely coadministered with aprepitant (Zhang et al, 2012). The protocol was approved by the Institutional Review Boards of the University of Texas Health Science Center San Antonio and the Dana-Farber/Harvard Cancer Center. The trial was conducted in accordance with good clinical practice and complied with the World Medical Association Declaration of Helsinki concerning written informed consent, which was obtained from all patients, and the protection of rights of human subjects.
Patients
Eligible patients were ⩾18 years of age with a histologically confirmed malignancy refractory to conventional treatment and evaluable by computed tomography (CT) scan or magnetic resonance imaging (MRI). Other inclusion criteria included an Eastern Cooperative Oncology Group (ECOG) performance status ⩽2; adequate organ and bone marrow function; willingness to use appropriate contraception for participants of childbearing age; and written informed consent. Patients were excluded if they had symptomatic brain metastases or primary central nervous system malignancy; had previous radiation to greater than 25% of the total bone marrow, radiation therapy within the previous 4 weeks, or continued toxicity from prior therapy; had received chemotherapy, biologic therapy, hormone therapy, or investigational therapies within 4 weeks, or mitomycin, nitrosourea, nilutamide, or bicalutamide within 6 weeks; had serious or uncontrolled infections or known HIV; were pregnant; or had any clinically significant condition that could prevent study completion.
Treatment and dose escalation
For part 1 (2-h infusions every 21 days) the starting dose was 1.85 mg m−2, and doubled in sequential patients until two patients experienced grade 2 toxicity, or DLT was observed. Intra-individual dose escalation was not allowed. Cohorts had at least three patients if the trigger for expansion was grade 2 toxicity, or at least six patients if the trigger was a DLT. If no additional toxicity occurred, subsequent doses were escalated in 40% increments in three-patient cohorts until the MAD was reached. If ⩾2 patients experienced DLT in one cohort, at least six patients were evaluated in the previous cohort. The highest dose tested below the MAD was considered the recommended phase 2 dose (RP2D) and was defined as the dose with an incidence of DLTs occurring in ⩽33% of patients. Dose-limiting toxicities were defined as any grade 3 or 4 hematologic toxicity lasting 1 week or longer, or as any grade 3 or 4 non-hematologic toxicity. Manageable nausea and vomiting, fatigue, anorexia, anaemia, alopecia, alkaline phosphatase changes, fever without neutropenia, or local reactions were not included in the determination of DLT.
In part 2, the first dose for 8-h infusions was the RP2D from part 1; due to DLTs, the dose was de-escalated until a dose level with no more than one DLT in six evaluable patients was reached. For 24-h infusions, the dose determined for the 8-h infusion was used as the first dose, with subsequent dose escalations in 40% increments. Dose modifications were permitted based on laboratory and clinical assessments on the day of treatment. Patients requiring delays were assessed weekly until dosing was resumed or the patient discontinued.
Toxicity, safety, and tolerability assessments
All treated patients were assessed for safety, including adverse events (AEs), complete blood count, laboratory assessments, vital signs, 12-lead electrocardiogram, and physical examination. Adverse events were defined and graded according to the NCI Common Terminology Criteria for Adverse Events (CTCAE, v3.0), and were recorded from enrolment until 3 weeks after the last dose.
Pharmacokinetic assessments
Pre- and post-dose 5 ml blood samples were collected at pre-specified time points in cycle 1, cycle 2, and cycle 3, during and after infusions. Plasma concentrations were determined using HPLC tandem mass spectrometry (LC-MS/MS) performed at Charles River Laboratory (Senneville, Quebec, Canada), and were used to determine PK parameters including maximum concentration (Cmax), time to maximum concentration (Tmax), area under the concentration–time curve to the final measurable sampling time (AUC[tf]), from 0 to 24 h (AUC[0–24 h]), and extrapolated to infinity (AUC[l]), as well as terminal phase half-life (t1/2), clearance (CL), and volume of distribution (Vd).
Ex vivo lymphocyte stimulation assay
As a biomarker for dinaciclib activity, whole blood samples for an ex vivo lymphocyte proliferation assay were obtained pre- and post-dose, as previously described (Nemunaitis et al, 2013; Supplementary Methods).
Assessment of CDK targets
Skin punch biopsies were obtained from the thigh, forearm or upper arm to assess Rb phosphorylation. Additionally, some patients were co-enrolled to a Dana-Farber Cancer Institute protocol permitting analysis of skin and tumour biopsies for other CDK targets. Skin biopsies were collected up to 7 days before dosing and at the end of the infusion. Phosphorylation of Rb was determined by immunohistochemistry in the proliferative keratinocyte layer, as previously described (Haddad et al, 2004; Leonard et al, 2012; Supplementary Methods). Additional analyses were performed for p27Kip1, cyclin D1, p53, and Ki-67. Data were quantified using Aperio image analysis or scored manually, and percent positively staining cells determined. When melanoma biopsies were complicated by melanin deposits, immunohistochemistry was also performed using a Texas red secondary antibody (Vulcan Fast Red, Biocare Medical, Pacheco, CA, USA).
Anti-tumour activity assessments
Computed tomography or MRI was obtained within 4 weeks before treatment initiation, after every 2 cycles, and 3 weeks after the final dose. Tumour response was assessed using Response Evaluation Criteria in Solid Tumors (RECIST) v. 1.0 (Therasse et al, 2000). Metabolic response of tumours to dinaciclib was measured using 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET)/CT scans performed at screening and on day 8 of cycle 1. The maximum standard uptake value (SUVmax) percentage change in lesions was determined. A 30% reduction relative to pre-treatment was classified as a response (Young et al, 1999).
Statistical analysis
Means, standard deviations and coefficients of variation were calculated using noncompartmental methods with WinNonlin software (V5.2, Pharsight, Cary, NC, USA) for derived PK parameters. For stimulated lymphocyte proliferation, pre- and post-treatment percent BrdU incorporation were compared. For skin biopsies, the percentage change in positively staining nuclei was determined for each sample; results for a particular phospho-protein or protein were averaged across the sample set and the degree of change post- compared to pre-treatment was evaluated with a paired t-test. For tumour biopsies, the percentage of positively staining cells pre- and post-treatment was compared for each antibody.
Results
Baseline characteristics and patient disposition
Thirty-five patients were treated in part 1 and 26 patients in part 2, with 16 and 10 patients receiving 8- and 24-h infusions, respectively (Table 1). Patients were heavily pre-treated with good performance status. Most patients (67%) discontinued treatment due to disease progression. Discontinuations also occurred because of symptomatic deterioration, withdrawal of consent for unrelated reasons or for AEs.
Determination of MAD and RP2D
Dose-limiting toxicities are summarised by dose level in Supplementary Table 1. In part 1, patients were administered escalating doses of dinaciclib ranging from 1.85 to 58 mg m−2. The first DLT occurred at 29.6 mg m−2, where one of six patients experienced non-neutropenic bacterial sepsis. A single patient experienced a DLT of neutropenic fever at the 41.4 mg m−2 dose level. The MAD was 58 mg m−2 with two of four patients experiencing DLT, including one patient with pancytopenia and pneumonia and one patient with neutropenic fever. An intermediate dose level of 50 mg m−2 was next evaluated; one of the initial six patients experienced a dose-limiting increase in aspartate aminotransferase (AST), which resolved by day 8. The patient continued treatment with a dose reduction. Nine additional patients were treated at the 50 mg m−2 dose level (for 15 total). Three patients experienced DLTs in the expansion cohort, including hypotension, elevated AST and uric acid, and elevated alanine aminotransferase (ALT). Therefore, 50 mg m−2 met the pre-specified RP2D definition, with 4 of 15 patients (<33%) experiencing DLT.
In part 2, patients received an 8- or 24-h i.v. infusion of dinaciclib starting at the part 1 RP2D of 50 mg m−2. There were two DLTs in two patients treated at the 50 mg m−2 dose level. The 8-h infusion was de-escalated from 50 mg m−2 to 41.4 mg m−2, 29.6 mg m−2, 14.8 mg m−2, and finally 7.4 mg m−2. DLTs after 8-h infusions included neutropenia with or without fever, hypotension, syncope, and elevated transaminases; no DLTs occurred at the 7.4 mg m−2 dose level. For 24-h infusions, the initial dose was 7.4 mg m−2, increased 40% to 10.4 mg m−2 and then to 14.6 mg m−2, which was the MAD with DLTs occurring in two of three patients; one patient had hyperbilirubinemia and another had delirium while also taking pregabalin. The 10.4 mg m−2 dose was the highest safe dinaciclib dose administered as a 24-h i.v. infusion with no DLTs in the three patients treated at this dose level or at the 7.4 mg m−2 dose level. Overall, DLTs were observed at lower doses with 8- and 24-h infusions vs 2-h infusions.
Safety and tolerability
Treatment-related AEs occurring in at least three patients, as well as all grade 3 or 4 AEs, are summarised in Table 2. Among the 35 patients over eight dose levels in part 1, the most common treatment-related AEs were nausea (23 (66%)), vomiting (23 (66%)), neutropenia (18 (51%)), diarrhoea (16 (46%)), and fatigue (13 (37%)). The most common grade 3 or 4 treatment-related AEs were neutropenia (16 (46%)), leukopenia (6 (17%)), increased AST (3 (9%)), increased ALT (2 (6%)), hyperuricemia (2 (6%)), and febrile neutropenia (2 (6%)). Among the fifteen patients treated at the RP2D of 50 mg m−2, the most common treatment-related AEs were nausea (12 (80%)), vomiting (11 (73%)), fatigue (9 (60%)), neutropenia (9 (60%)), and diarrhoea (8 (53%)), and the most common grade 3 or 4 treatment-related AEs were neutropenia (8 (53%)), increased AST (3 (20%)), increased ALT (2 (13%)), hyperuricemia (2 (13%)), and leukopenia (2 (13%)).
At doses of 41.4 mg m−2 and above, acute neutropenia was observed in some patients within 4–6 h post-dose on day 1. This was followed by a rapid recovery, often followed by a second nadir at day 8 with a slower recovery. These results were suggestive of abrupt destruction of circulating neutrophils on day 1 and more conventional marrow suppression on day 8 (Supplementary Figure 1).
In part 2, among the 16 patients treated with 8-h infusions, the most frequent treatment-related AEs were fatigue (8 (50%)), diarrhoea (7 (44%)), nausea (7 (44%)), neutropenia (7 (44%)), and vomiting (6 (38%)); the most frequent grade 3 or 4 treatment-related AEs were neutropenia (6 (38%)), febrile neutropenia (2 (13%)), and hypotension (2 (13%)). For the 10 patients treated with 24-h infusions, the most common treatment-related AEs were increased AST (2 (20%)), increased alkaline phosphatase (2 (20%)), fatigue (2 (20%)), and nausea (2 (20%)). The only grade 3 or 4 treatment-related AE reported in more than one patient in this cohort was fatigue (2 (20%)).
Seventeen (47%) patients in part 1 and 10 (38%) patients in part 2 experienced serious AEs (SAEs). The most common SAEs occurring in two or more patients in either part 1 or part 2 of the study were neutropenia (4 (11%) in part 1; 2 (8%) in part 2), febrile neutropenia (2 (6%) in part 1; 2 (8%) in part 2), hyperbilirubinemia (3 (8%)) in part 1), hypotension (3 (8%) in part 1; 3 (12%) in part 2), bacterial sepsis (2 (6%) in part 1), and increased AST (2 (6%) in part 1). Eight deaths occurred among patients before study treatment was discontinued. One patient enrolled at the 29.6 mg m−2 dose level in part 1 died of gram-negative sepsis; other events were all related to progressive disease.
Pharmacokinetics
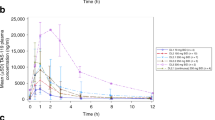
Among the 35 patients in Part 1, dinaciclib rapidly distributed with Tmax achieved between 1 and 2 h after the initiation of the 2-h infusion, and eliminated with a t1/2 of 1.4–3.3 h (Table 3, Supplementary Figure 2A). Dose- normalised PK parameters were determined across the doses, suggesting dose-related increases in exposure (Supplementary Figure 2B). In part 2, PK for the 16 patients who had dinaciclib administered over 8 h demonstrated a Tmax of 4–8 h after the start of the infusion followed by a rapid elimination phase (Table 3, Supplementary Figure 2B). When dinaciclib was administered over 24 h, Tmax was achieved 6–24 h after the start of the infusion and also displayed a rapid elimination phase (Table 3, Supplementary Figure 2C). For both 8-h and 24-h infusion groups, the t1/2 and CL could not be estimated due to the sampling schedule. At similar doses, with increasing infusion time (2, 8, and 24 h) the total exposure (AUC) remained similar, whereas Cmax was lower with longer infusion times. Based on the PK findings, dinaciclib CL appears to be dose-independent.
Decreases in absolute neutrophil were found to correlate with dinaciclib exposure, with Cmax 360 ng ml−1 and AUC 944 ng.hr ml−1 associated with a 50% reduction compared to baseline. The percent decrease in ANC increased as dose and systemic exposure to dinaciclib increased, with neutropenia observed frequently at doses of 29.6 mg m−2 or higher (Supplementary Figure 3).
Ex vivo lymphocyte proliferation
Inhibition of lymphocyte proliferation in whole blood stimulated with PHA was used as an indicator of dinaciclib activity. Pharmacodynamic reductions in BrdU incorporation were observed in 24 of 35 patients enrolled in part 1 of the study, with reduction of PHA-stimulated BrdU incorporation to <5% at at least one post-dose time point observed in 23 of these patients. Results for samples from individual patients collected over time are shown in Figure 1. Reductions to <5% BrdU incorporation were observed at plasma concentrations ∼200 ng ml−1, achieved at doses ⩾7.4 mg m−2. Additionally, there was a prolongation of inhibition of lymphocyte proliferation with increasing dose, with a sustained PD effect through 8 h reproducibly achieved at doses ⩾29.6 mg m−2. Similar data were obtained from patients who received 8-h infusions, with suppression of lymphocyte proliferation also achieved at doses ⩾7.4 mg m−2; PD effects were noted at 1-h and sustained through the duration of the infusion at doses ⩾14.8 mg m−2 (Supplementary Figure 4).
Ex vivo assay of phytohemagglutinin (PHA)-stimulated lymphocyte proliferation. (A) BrdU incorporation of lymphocytes obtained from representative patients before and after 2-h dinaciclib infusions. BrdU=bromodeoxyuridine; D=day. (B) Relationship between percent BrdU uptake relative to baseline and dinaciclib plasma concentration in patients treated with 2-h infusions. Two additional samples with plasma concentrations >2000 and 3000 ng ml−1 demonstrated no BrdU uptake and are not plotted. Symbols indicate the time after the start of infusion when the sample was procured.
Assessment of CDK targets in skin and tumour biopsies
Based on the results of the ex vivo lymphocyte proliferation assay, we focused our analysis of skin biopsies procured pre- and post-treatment for patients who received 2-h infusions enrolled to dose levels of 29.6 mg m−2 and above. Figure 2A shows the average % decline in positively stained nuclei for multiple phosphorylated forms of Rb, total Rb and Ki-67.
CDK targets assessed in skin biopsies of patients before and after intravenous infusions of dinaciclib>29.6 mg m−2. (A) Quantification of the percent decline in number of keratinocytes staining positively for expression of various forms of phosphorylated Rb, total Rb and Ki-67 in post- compared to pre-treatment samples. (B) Quantification of the percent decline or increase in number of keratinocytes staining positively for expression of p27Kip1, cyclin D1 and p53 in post- compared to pre-treatment samples. In (A) and (B), the number of paired samples analysed is indicated above or below the bar. ***P<0.0001; **P<0.01; *P<0.05 in paired t-tests. (C) Representative micrographs from pre- and post-treatment samples demonstrating reduced staining for Rb [pT356], relatively unchanged staining of total Rb and Rb [S807/S811] and increased staining of p53 in post-treatment samples.
Among the samples tested, the greatest decline in staining occurred for Rb at sites likely phosphorylated by both CDK4 and CDK2, including T356 and S795 (Zarkowska and Mittnacht, 1997), demonstrating approximately 25 and 19% reductions, respectively. Decreased staining at sites typically considered to be CDK4-specific sites, including S249/T252, S807/S811 and S780 (Kitagawa et al, 1996; Zarkowska and Mittnacht, 1997; Brantley and Harbour, 2000) was more modest, as was the change in total Rb, all of which demonstrated<11% reduction. These results are suggestive of preferential CDK2 inhibition by dinaciclib in skin. Figure 2B shows the average changes in staining for p27Kip1, cyclin D1 and p53 staining post-treatment. Whereas p27Kip1 levels were relatively stable, levels of cyclin D1 decreased and those of p53 increased after dinaciclib exposure, effects consistent with inhibition of CDK9 (Alonso et al, 2003; Demidenko and Blagosklonny, 2004; Chen et al, 2010; Desai et al, 2013). Representative micrographs are shown in Figure 2C.
Among the samples collected from patients treated with 8-h infusions, the degree of changes of these markers was overall similar to that observed after 2-h infusions (Supplementary Figure 5). Notably, these changes did not translate to evidence of reduced proliferation, with no substantial reduction in Ki-67 staining post-treatment (Figure 2A). Similarly, there was no clear association with clinical outcome. The two patients who remained on trial longest (22 and 30 cycles) had the steepest declines in phospho- Rb [T356] of 90 and 78%, respectively. Nonetheless, although the majority of the eight patients who remained on trial for at least six cycles showed substantial decline in T356 staining and/or increased p53 expression, these trends were also present among patients whose best response was PD.
Pre- and post-treatment tumour biopsies were obtained among three patients with metastatic melanoma (Figure 3). The results among these tumour pairs similarly demonstrate reduced expression of Rb phosphorylated at T356 and S795, and overall preserved expression of Rb phosphorylated at other sites and of total Rb. Increases in p27Kip1 and p53 post-treatment occurred in two samples. These findings are suggestive of dinaciclib- mediated inhibition of CDK2 and CDK9 in tumour cells (Sheaff et al, 1997; Vlach et al, 1997; Alonso et al, 2003; Demidenko and Blagosklonny, 2004).
CDK targets assessed in paired tumour biopsies from three patients with metastatic melanoma. Post-treatment biopsies were obtained within 24 h after the end of the infusion. (A) Quantification and representative micrographs from a patient treated with 50 mg m−2 over 2 h. Most notable changes in the post-treatment sample are reduced Rb [pT356], unchanged expression of other phospho-Rb forms, and increased expression of p27Kip1 and slight induction of p53. (B) Quantification and representative micrographs from a patient treatment with 29.6 mg m−2 over 2 h, with similar changes, including reduced Rb [pS795]. (C) Quantification and representative micrographs from a patient treated with 14.8 mg m−2 over 8 h, again demonstrating similar pharmacodynamic changes, most notably with reduced Rb [pT356] and Rb [pS795].
Anti-tumour response
No complete or partial RECIST responses were observed. Stable disease was achieved for at least six treatment cycles in eight patients, extending to 30 treatment cycles in a patient with castrate-resistant prostate cancer (Supplementary Table 2). Data from FDG-PET/CT scans pre-treatment and on day 8 of cycle 1 were available for 12 out of 15 patients treated at the RP2D of 50 mg m−2. In these patients, the FDG-PET/CT response rate was 16.7% (2 out of 12; one-sided 95% CI: 0.03, 1.00; two-sided 95% CI: 0.021, 0.484). Metabolic changes in tumours at day 8, shown in Supplementary Figure 6, were not routinely predictive of prolonged stable disease.
Discussion
This trial has established the RP2D of dinaciclib as 50 mg m−2 administered as a 2-h i.v. infusion every 21 days. Escalation was limited by hematologic toxicity, including pancytopenia and neutropenic fever. Additional dose-limiting events included hypotension, elevated transaminases and hyperuricemia.
Neutropenia was the most common hematologic toxicity associated with dinaciclib and occurred acutely, often with recovery within 48 h. This phenomenon may possibly be related to abrupt depletion of short half-life MCL1 mRNA and protein levels in neutrophils as a consequence of CDK9 inhibition, compromising neutrophil survival (Dzhagalov et al, 2007). Such destruction could be accompanied by changes in metabolic parameters, including elevated uric acid and transaminases, which may also rapidly resolve. Following recovery, reduced neutrophil count was also noted mid-cycle, typical of agents that affect proliferation of the marrow stem cell population.
A 2-h infusion of dinaciclib has also been evaluated in patients with solid tumours on a day 1, 8, 15 schedule; in this trial the MAD was 14 mg m−2 and RP2D defined at 12 mg m−2, with escalation limited by hypotension and hyperuricemia that complicated the initial infusions (Nemunaitis et al, 2013). While these events occurred among patients in the current study, and scored as DLTs among the expanded group of patients enrolled at 50 mg m−2, they did not limit escalation through the lower dose levels. Dinaciclib-induced hypotension may be a component of cytokine-release syndrome, which has been observed in patients with solid tumours or hematologic malignancies treated with the CDK inhibitor flavopiridol (Phelps et al, 2009; Ramaswamy et al, 2012). The profound effects of these agents on cellular transcription may alter cytokine production accounting for such events. Development of cytokine release syndrome with associated hypotension may be erratic and not strictly dose-dependent, and may explain the ability to escalate dinaciclib to a substantially higher dose in the current study. Neutropenia was far less common in the weekly study with grade ⩾3 events occurring in only 10% of subjects. While 50 mg m−2 would not be expected to be tolerable on a weekly schedule, it is conceivable that an intermediate dose level would have been acceptable if a larger number of patients had been evaluated. The weekly study utilised an accelerated titration design through 1.32 mg m−2, after which a 3+3 design was employed; alternative statistical modelling may have ultimately resulted in a higher RP2D on this schedule (Cook et al, 2015). Additionally, we have found that concomitant intravenous fluids and steroid administration can ameliorate dinaciclib-induced hypotension, so that aggressive supportive measures are likely to permit the routine administration of doses higher than 12 mg m−2. Such supportive measures may also include anti-diarrhoeal agents and additional anti-emetics, including aprepitant, which does not significantly alter dinaciclib PK parameters (Zhang et al, 2012).
The plasma half-life associated with 2-h dinaciclib infusions is short, prompting us to evaluate longer infusions designed to extend target coverage and ameliorate toxicity. Although Cmax and the percentage of patients with severe neutropenia were reduced with longer infusions, other toxicities occurred including elevated liver function tests, neurologic events, hypotension, fatigue and nausea that required doses in the 7.4–10.4 mg m−2 range for tolerability; these toxicities precluded future development of these schedules.
Dinaciclib resulted in a sustained reduction in BrdU incorporation of PHA-stimulated lymphocytes in response to administration of doses ⩾29.6 mg m−2, although the actual dose required to achieve this effect may be lower since whole blood was diluted approximately 1 : 5 in the assay conditions. Consistent with dose-dependent effects, the degree of reduction in BrdU incorporation was greater in response to 29 mg m−2 in this study compared to reductions noted in the weekly study after administration of 12 mg m−2 (Nemunaitis et al, 2013).
We further assessed G1 CDK inhibition by dinaciclib by assessing Rb phosphorylation in skin and tumour biopsies. Although several models for CDK-mediated Rb phosphorylation have been proposed, with controversy over the existence of CDK4 and CDK2-selective sites (Kitagawa et al, 1996; Zarkowska and Mittnacht, 1997; Brantley and Harbour, 2000; Narasimha et al, 2014), we found that dinaciclib preferentially reduced phosphorylation of T356 and S795 in keratinocytes and tumour cells, and similar to results in the weekly study did not substantially reduce Rb phosphorylation at S807/S811 (Nemunaitis et al, 2013), results most consistent with CDK2 inhibition. Phosphorylation at T356 may be particularly important for the release of E2F transcription factors and S phase progression (Burke et al, 2010; Macdonald and Dick, 2012) and has been shown to predict reduced survival in HPV-negative squamous cell carcinoma of the head and neck, reflective of the proliferative potential afforded when this site is phosphorylated (Beck et al, 2015). Increased p27Kip1 post-treatment is consistent with stabilisation mediated by CDK2 inhibition (Sheaff et al, 1997; Vlach et al, 1997), but may not have occurred in all samples because CDKN1B transcription may be compromised by CDK9 inhibition (Jiang et al, 2003). CDK9 inhibition also affects transcription of both CCND1 and hDM2, so that reduced cyclin D1 and increased p53 in skin and tumour were expected consequences when this target is engaged.
Despite these changes in keratinocytes and tumour, there was little effect on proliferation, measured by Ki-67 staining. Ki-67 may be expressed during all phases of the cell cycle (Gerdes et al, 1984) and therefore may not have accurately assessed mid-G1 arrest in tumour cells; mitotic markers may have been preferable. Additionally, as preclinical experiments point to a propensity for dinaciclib to induce cell death (Parry et al, 2010; Desai et al, 2013) markers of apoptosis will be important to assess in tumour biopsies procured in future trials. Baseline levels of anti-apoptotic proteins, including MCL1 and Bcl-xL, may predict response to dinaciclib and will also merit evaluation (Booher et al, 2014).
Although preliminary evidence points to inhibition of CDK2 and CDK9 in keratinocytes, these pharmacodynamic effects did not correlate with clinical outcome, suggesting limitations of the use of surrogate proliferating tissue. The melanoma patients who underwent tumour biopsies achieved SD as the best response, but evaluation of more patients will be required to determine whether these PD changes relate to efficacy. Of note, in cell line experiments, induction of cell death correlated with near complete suppression of BrdU incorporation (Parry et al, 2010). The incomplete suppression of Rb phosphorylation we observed may have been adequate to achieve some degree of tumour growth inhibition, but not apoptotic effects, perhaps accounting for the lack of objective responses observed.
While no RECIST responses occurred, day 8 metabolic changes by PET/CT occurred in some patients, although such early changes did not necessarily translate to prolonged stable disease. Perhaps early effects demonstrating target engagement or reduced tumour metabolic activity could be maintained if more continuous dosing were possible. Approximately 10% of heavily pre-treated patients enrolled did achieve stable disease lasting>6 months, also suggestive of preliminary anti-tumour activity.
Nevertheless, the toxicity profile, incomplete target inhibition and paucity of objective responses in solid tumours are characteristic of the class of CDK inhibitors that target the cell cycle CDKs 1 and 2 and transcriptional CDKs (Shapiro, 2006). These agents have typically shown greater efficacy in trials of hematologic malignancies, and weekly dinaciclib has demonstrated activity in both CLL and multiple myeloma (Flynn et al, 2015; Kumar et al, 2015). This is in contrast to the selective CDK4/6 inhibitors, palbociclib, ribociclib and abemaciclib, all orally bioavailable agents that can be administered at least 3 of every 4 weeks (or in the case of abemaciclib, continuously), are better tolerated, have produced evidence of more complete target engagement (Leonard et al, 2012) and have demonstrated meaningful clinical efficacy in solid tumours with prolonged tumour growth inhibition or partial response, related to the biological effects of cell cycle arrest and senescence (Sherr et al, 2016).
Additional trials will be required to determine whether dinaciclib will have any role in the solid tumour armamentarium. Dinaciclib has been evaluated in small randomised trials of breast and lung cancer (Mita et al, 2014; Stephenson et al, 2014), confirming tolerability of the 50 mg m−2 dose level and demonstrating partial responses in two of seven patients with hormone receptor-positive breast cancer. Considering that CCNE1 amplification or other means of CDK2 activation (Taylor-Harding et al, 2015; Herrera-Abreu et al, 2016) comprise mechanisms of resistance to selective CDK4/6 inhibitors, the demonstration of CDK2 inhibitory activity may position dinaciclib for use upon acquired resistance to these agents. Alternatively, the effects of CDK1/2 and CDK12 inhibition on DNA repair pathways and the compromise of transcription mediated by CDK9 inhibition suggest several combinatorial strategies with DNA damaging agents (Johnson and Shapiro, 2011), BCL2 family targeted agents (Booher et al, 2014) or epigenetic modulators (Jang et al, 2005; Baker et al, 2015) in future studies that may lead to approaches with more pronounced clinical activity.
Change history
26 October 2017
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alonso M, Tamasdan C, Miller DC, Newcomb EW (2003) Flavopiridol induces apoptosis in glioma cell lines independent of retinoblastoma and p53 tumor suppressor pathway alterations by a caspase-independent pathway. Mol Cancer Ther 2: 139–150.
Asghar U, Witkiewicz AK, Turner NC, Knudsen ES (2015) The history and future of targeting cyclin-dependent kinases in cancer therapy. Nat Rev Drug Discov 14: 130–146.
Baker EK, Taylor S, Gupte A, Sharp PP, Walia M, Walsh NC, Zannettino AC, Chalk AM, Burns CJ, Walkley CR (2015) BET inhibitors induce apoptosis through a MYC independent mechanism and synergise with CDK inhibitors to kill osteosarcoma cells. Sci Rep 5: 10120.
Beck TN, Kaczmar J, Handorf E, Nikonova A, Dubyk C, Peri S, Lango M, Ridge JA, Serebriiskii IG, Burtness B, Golemis EA, Mehra R (2015) Phospho-T356RB1 predicts survival in HPV-negative squamous cell carcinoma of the head and neck. Oncotarget 6: 18863–18874.
Booher RN, Hatch H, Dolinski BM, Nguyen T, Harmonay L, Al-Assaad AS, Ayers M, Nebozhyn M, Loboda A, Hirsch HA, Zhang T, Shi B, Merkel CE, Angagaw MH, Wang Y, Long BJ, Lennon XQ, Miselis N, Pucci V, Monahan JW, Lee J, Kondic AG, Im EK, Mauro D, Blanchard R, Gilliland G, Fawell SE, Zawel L, Schuller AG, Strack P (2014) MCL1 and BCL-xL levels in solid tumors are predictive of dinaciclib-induced apoptosis. PLoS One 9: e108371.
Brantley MA, Harbour JW (2000) Inactivation of retinolbastoma protein in uveal melanoma by phosphorylation of sites in the COOH-terminal region. Cancer Res 60: 4320–4323.
Burke JR, Deshong AJ, Pelton JG, Rubin SM (2010) Phosphorylation-induced conformational changes in the retinoblastoma protein inhibit E2F transactivation domain binding. J Biol Chem 285: 16286–16293.
Cai D, Latham VM Jr, Zhang X, Shapiro GI (2006) Combined depletion of cell cycle and transcriptional cyclin-dependent kinase activities induces apoptosis in cancer cells. Cancer Res 66: 9270–9280.
Chen R, Chubb S, Cheng T, Hawtin RE, Gandhi V, Plunkett W (2010) Responses in mantle cell lymphoma cells to SNS-032 depend on the biological context of each cell line. Cancer Res 70: 6587–6597.
Choudhary GS, Tat TT, Misra S, Hill BT, Smith MR, Almasan A, Mazumder S (2015) Cyclin E/Cdk2-dependent phosphorylation of Mcl-1 determines its stability and cellular sensitivity to BH3 mimetics. Oncotarget 6: 16912–16925.
Cook N, Hansen AR, Siu LL, Abdul Razak AR (2015) Early phase clinical trials to identify optimal dosing and safety. Mol Oncol 9: 997–1007.
Demidenko ZN, Blagosklonny MV (2004) Flavopiridol induces p53 via initial inhibition of Mdm2 and p21 and, independently of p53, sensitizes apoptosis-reluctant cells to tumor necrosis factor. Cancer Res 64: 3653–3660.
Desai BM, Villanueva J, Nguyen TT, Lioni M, Xiao M, Kong J, Krepler C, Vultur A, Flaherty KT, Nathanson KL, Smalley KS, Herlyn M (2013) The anti-melanoma activity of dinaciclib, a cyclin-dependent kinase inhibitor, is dependent on p53 signaling. PLoS One 8: e59588.
Dzhagalov I St, John A, He YW (2007) The antiapoptotic protein Mcl-1 is essential for the survival of neutrophils but not macrophages. Blood 109: 1620–1626.
Eick D, Geyer M (2013) The RNA polymerase II carboxy-terminal domain (CTD) code. Chem Rev 113: 8456–8490.
Feldmann G, Mishra A, Bisht S, Karikari C, Garrido-Laguna I, Rasheed Z, Ottenhof NA, Dadon T, Alvarez H, Fendrich V, Rajeshkumar NV, Matsui W, Brossart P, Hidalgo M, Bannerji R, Maitra A, Nelkin BD (2011) Cyclin-dependent kinase inhibitor Dinaciclib (SCH727965) inhibits pancreatic cancer growth and progression in murine xenograft models. Cancer Biol Ther 12: 598–609.
Feldmann G, Mishra A, Hong SM, Bisht S, Strock CJ, Ball DW, Goggins M, Maitra A, Nelkin BD (2010) Inhibiting the cyclin-dependent kinase CDK5 blocks pancreatic cancer formation and progression through the suppression of Ras-Ral signaling. Cancer Res 70: 4460–4469.
Flynn J, Jones J, Johnson AJ, Andritsos L, Maddocks K, Jaglowski S, Hessler J, Grever MR, Im E, Zhou H, Zhu Y, Zhang D, Small K, Bannerji R, Byrd JC (2015) Dinaciclib is a novel cyclin-dependent kinase inhibitor with significant clinical activity in relapsed and refractory chronic lymphocytic leukemia. Leukemia 29: 1524–1529.
Fu W, Ma L, Chu B, Wang X, Bui MM, Gemmer J, Altiok S, Pledger WJ (2011) The cyclin-dependent kinase inhibitor SCH 727965 (dinacliclib) induces the apoptosis of osteosarcoma cells. Mol Cancer Ther 10: 1018–1027.
Gerdes J, Lemke H, Baisch H, Wacker HH, Schwab U, Stein H (1984) Cell cycle analysis of a cell prolfieration-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J Immunol 133: 1710–1715.
Gregory GP, Hogg SJ, Kats LM, Vidacs E, Baker AJ, Gilan O, Lefebure M, Martin BP, Dawson MA, Johnstone RW, Shortt J (2015) CDK9 inhibition by dinaciclib potently suppresses Mcl-1 to induce durable apoptotic responses in aggressive MYC-driven B- cell lymphoma in vivo. Leukemia 29: 1437–1441.
Haddad RI, Weinstein LJ, Wieczorek TJ, Bhattacharya N, Raftopoulos H, Oster MW, Zhang X, Latham VM Jr, Costello R, Faucher J, DeRosa C, Yule M, Miller LP, Loda M, Posner MR, Shapiro GI (2004) A phase II clinical and pharmacodynamic study of E7070 in patients with metastatic, recurrent, or refractory squamous cell carcinoma of the head and neck: modulation of retinoblastoma protein phosphorylation by a novel chloroindolyl sulfonamide cell cycle inhibitor. Clin Cancer Res 10: 4680–4687.
Herrera-Abreu MT, Palafox M, Asghar U, Rivas MA, Cutts RJ, Garcia-Murillas I, Pearson A, Guzman M, Rodriguez O, Grueso J, Bellet M, Cortés J, Elliott R, Pancholi S, Baselga J, Dowsett M, Martin LA, Turner NC, Serra V (2016) Early adaptation and acquired resistance to CDK4/6 inhibition in estrogen receptor-positive breast cancer. Cancer Res 76: 2301–2313.
Jang MK, Mochizuki K, Zhou M, Jeong HS, Brady JN, Ozato K (2005) The bromodomain protein Brd4 is a positive regulatory component of P-TEFb and stimulates RNA polymerase II-dependent transcription. Mol Cell 19: 523–534.
Jiang J, Matranga CB, Cai D, Latham VM, Zhang X, Lowell AM, Martelli F, Shapiro GI (2003) Flavopiridol-induced apoptosis during S phase requires E2F-1 and inhibition of cyclin A-dependent kinase activity. Cancer Res 63: 7410–7422.
Johnson N, Shapiro GI (2011) Cyclin-dependent kinases (cdks) and the DNA damage response: rationale for cdk inhibitor-chemotherapy combinations as an anticancer strategy for solid tumors. Expert Opin Ther Targets 14: 1199–1212.
Johnson SF, Cruz C, Greifenberg AK, Dust S, Stover DG, Chi D, Primack B, Cao S, Bernhardy AJ, Coulson R, Lazaro JB, Kochupurakkal B, Sun H, Unitt C, Moreau LA, Sarosiek KA, Scaltriti M, Juric D, Baselga J, Richardson AL, Rodig SJ, D’Andrea AD, Balmaña J, Johnson N, Geyer M, Serra V, Lim E, Shapiro GI (2016) CDK12 inhibition reverses de novo and acquired PARP inhibitor resistance in BRCA wild-type and mutated models of triple-negative breast cancer. Cell Rep 17: 2367–2381.
Kawauchi T (2014) Cdk5 regulates multiple cellular events in neural development, function and disease. Dev Growth Differ 56: 335–348.
Kitagawa M, Higashi H, Jung HK, Suzuki-Takahashi I, Ikeda M, Tamai K, Kato JY, Segawa K, Yoshida E, Nishimura S, Taya Y (1996) The consensus motif for phosphorylation by cyclin D1-cdk4 is different from that for phosphorylation by cyclin A/E-cdk2. EMBO J 15: 7060–7069.
Kumar SK, LaPlant B, Chng WJ, Zonder J, Callander N, Fonseca R, Fruth B, Roy V, Erlichman C, Stewart AK Mayo Phase 2 Consortium (2015) Dinaciclib, a novel CDK inhibitor, demonstrates encouraging single-agent activity in patients with relapsed multiple myeloma. Blood 125: 443–448.
Leonard JP, LaCasce AS, Smith MR, Noy A, Chirieac LR, Rodig SJ, Yu JQ, Vallabhajosula S, Schoder H, English P, Neuberg DS, Martin P, Millenson MM, Ely SA, Courtney R, Shaik N, Wilner KD, Randolph S, Van den Abbeele AD, Chen-Kiang SY, Yap JT, Shapiro GI (2012) Selective CDK4/6 inhibition with tumor responses by PD0332991 in patients with mantle cell lymphoma. Blood 119: 4597–4607.
Macdonald JI, Dick FA (2012) Posttranslational modifications of the retinoblastoma tumor suppressor protein as determinants of function. Genes Cancer 3: 619–633.
Malumbres M (2014) Cyclin-dependent kinases. Genome Biol 15: 122.
Malumbres M, Barbacid M (2009) Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer 9: 153–166.
Mita MM, Joy AA, Mita A, Sankhala K, Jou YM, Zhang D, Statkevich P, Zhu Y, Yao SL, Small K, Bannerji R, Shapiro CL (2014) Randomized phase II trial of the cyclin- dependent kinase inhibitor dinaciclib (MK-7965) versus capecitabine in patients with advanced breast cancer. Clin Breast Cancer 14: 169–176.
Narasimha AM, Kaulich M, Shapiro GS, Choi YJ, Sicinski P, Dowdy SF (2014) Cyclin D activates the Rb tumor suppressor by mono-phosphorylation. Elife 3: e02872.
Nemunaitis JJ, Small KA, Kirschmeier P, Zhang D, Zhu Y, Jou YM, Statkevich P, Yao SL, Bannerji R (2013) A first-in-human, phase 1, dose-escalation study of dinaciclib, a novel cyclin-dependent kinase inhibitor, administered weekly in subjects with advanced malignancies. J Transl Med 11: 259.
Parry D, Guzi T, Shanahan F, Davis N, Prabhavalkar D, Wiswell D, Seghezzi W, Paruch K, Dwyer MP, Doll R, Nomeir A, Windsor W, Fischmann T, Wang Y, Oft M, Chen T, Kirschmeier P, Lees EM (2010) Dinaciclib (SCH 727965), a novel and potent cyclin- dependent kinase inhibitor. Mol Cancer Ther 9: 2344–2353.
Paruch K, Dwyer MP, Alvarez C, Brown C, Chan TY, Doll RJ, Keertikart K, Knutson C, McKittrick B, Rivera J, Rossman R, Tucker G, Fischmann T, Hruza A, Madison V, Nomeir AA, Wang Y, Kirschmeier P, Lees E, Parry D, Sgambellone N, Seghezzi W, Schultz L, Shanahan F, Wiswell D, Xu X, Zhou Q, James RA, Paradkar VM, Park H, Rokosz LR, Stauffer TM, Guzi TJ (2010) Discovery of dinaciclib (SCH 727965): a potent and selective inhibitor of cyclin-dependent kinases. ACS Med Chem Lett 1: 204–208.
Phelps MA, Lin TS, Johnson AJ, Hurh E, Rozewski DM, Farley KL, Wu D, Blum KA, Fischer B, Mitchell SM, Moran ME, Brooker-McEldowney M, Heerema NA, Jarjoura D, Schaaf LJ, Byrd JC, Grever MR, Dalton JT (2009) Clinical response and pharmacokinetics from a phase 1 study of an active dosing schedule of flavopiridol in relapsed chronic lymphocytic leukemia. Blood 113: 2637–2645.
Ramaswamy B, Phelps MA, Baiocchi R, Bekaii-Saab T, Ni W, Lai JP, Wolfson A, Lustberg ME, Wei L, Wilkins D, Campbell A, Arbogast D, Doyle A, Byrd JC, Grever MR, Shah MH (2012) A dose-finding, pharmacokinetic and pharmacodynamic study of a novel schedule of flavopiridol in patients with advanced solid tumors. Invest New Drugs 30: 629–638.
Shapiro GI (2006) Cyclin-dependent kinase pathways as targets for cancer treatment. J Clin Oncol 24: 1770–1783.
Sheaff RJ, Groudine M, Gordon M, Roberts JM, Clurman BE (1997) Cyclin E-cdk2 is a regulator of p27Kip1. Genes Dev 11: 1464–1478.
Sherr CJ, Beach D, Shapiro GI (2016) Targeting CDK4 and CDK6: from discovery to therapy. Cancer Discov 6: 353–367.
Simon R, Freidlin B, Rubinstein L, Arbuck SG, Collins J, Christian MC (1997) Accelerated titration designs for phase I clinical trials in oncology. J Natl Cancer Inst 89: 1138–1147.
Stephenson JJ, Nemunaitis J, Joy AA, Martin JC, Jou YM, Zhang D, Statkevich P, Yao SL, Zhu Y, Zhou H, Small K, Bannerji R, Edelman MJ (2014) Randomized phase 2 study of the cyclin-dependent kinase inhibitor dinaciclib (MK-7965) versus erlotinib in patients with non-small cell lung cancer. Lung Cancer 83: 219–223.
Taylor-Harding B, Aspuria PJ, Agadjanian H, Cheon DJ, Mizuno T, Greenberg D, Allen JR, Spurka L, Funari V, Spiteri E, Wang Q, Orsulic S, Walsh C, Karlan BY, Wiedemeyer WR (2015) Cyclin E1 and RTK/RAS signaling drive CDK inhibitor resistance via activation of E2F and ETS. Oncotarget 6: 696–714.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92: 205–216.
Vlach J, Hennecke S, Amati B (1997) Phosphorylation-dependent degradation of the cyclin-dependent kinase inhibitor p27. EMBO J 16: 5334–5344.
Young H, Baum R, Cremerius U, Herholz K, Hoekstra O, Lammertsma AA, Pruim J, Price P (1999) Measurement of clinical and subclinical tumour response using [18F]- fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET Study Group. Eur J Cancer 35: 1773–1782.
Zarkowska T, Mittnacht S (1997) Differential phosphorylation of the retinoblastoma protein by G1/S cyclin-dependent kinases. J Biol Chem 272: 12738–12746.
Zhang D, Mita M, Shapiro GI, Poon J, Small K, Tzontcheva A, Kantesaria B, Zhu Y, Bannerji R, Statkevich P (2012) Effect of aprepitant on the pharmacokinetics of the cyclin-dependent kinase inhibitor dinaciclib in patients with advanced malignancies. Cancer Chemother Pharmacol 70: 891–898.
Acknowledgements
Medical writing and/or editorial assistance was provided by Amy O. Johnson-Levonas, PhD and Sheila Erespe, MS (both of Merck & Co., Inc., Kenilworth, NJ, USA) as well as Kakuri Omari, PhD and Joseph Abrajano, PhD of Integrus Scientific, a division of Medicus International New York. This assistance was funded by Merck & Co., Inc., Kenilworth, NJ, USA. This research was supported by Merck & Co., Inc., Kenilworth, NJ, USA. Research core and programme infrastructure was funded by Cancer Center Support Grants P30 CA054174 and P30 CA006516 to the Institute for Drug Development, Cancer Therapy and Research Center at University of Texas Health Science Center San Antonio and the Dana-Farber/Harvard Cancer Center, respectively. Work on the skin and tumour biopsies was in part funded by R01 CA090687 (GIS), and philanthropic funds from the Piccolo family to the Early Drug Development Center of the Dana-Farber Cancer Institute.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
JP, KAS, Y-MJ, PK, DZ, YZ, PS, and RB are present or former employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA. JMC has served as a consultant for Agios, received grants from Merck & Co., Inc., and received travel/ accommodations from Roche and Bristol Myers Squibb (BMS). LRC has served as a consultant for Wilcox & Savage, Medical Science Affiliates, and Shook, Hardy & Bacon, and has given expert testimony for Shook, Hardy & Bacon, and has received royalties from Springer. SR has served as a member of the board for Perkin Elmer Inc., has received grants from BMS, and has received payment for lectures from BMS. GIS has received consultant fees from Lilly, Pfizer, G1 Therapuetics, Vertex, and EMD Serono. His institution has received grants from Lilly and Pfizer. An SRA related to immunohistochemical staining of skin and tumour biopsies, under which there will be payment from Merck to the Brigham and Women’s Hospital for work completed, will be executed in relation to this work. All other authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Mita, M., Mita, A., Moseley, J. et al. Phase 1 safety, pharmacokinetic and pharmacodynamic study of the cyclin-dependent kinase inhibitor dinaciclib administered every three weeks in patients with advanced malignancies. Br J Cancer 117, 1258–1268 (2017). https://doi.org/10.1038/bjc.2017.288
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2017.288
Keywords
This article is cited by
-
A nano-cocktail of the PARP inhibitor talazoparib and CDK inhibitor dinaciclib for the treatment of triple negative breast cancer
Cancer Nanotechnology (2024)
-
Targeting CDK1 in cancer: mechanisms and implications
npj Precision Oncology (2023)
-
CDK9 inhibitors in multiple myeloma: a review of progress and perspectives
Medical Oncology (2022)
-
LncRNA TROJAN promotes proliferation and resistance to CDK4/6 inhibitor via CDK2 transcriptional activation in ER+ breast cancer
Molecular Cancer (2020)
-
PES1 promotes BET inhibitors resistance and cells proliferation through increasing c-Myc expression in pancreatic cancer
Journal of Experimental & Clinical Cancer Research (2019)