Abstract
Background:
Application of curative therapy for hepatocellular carcinoma is crucially dependent on underlying liver function. Using the recently described ALBI grade we examined the long-term impact of liver dysfunction on survival of early-stage hepatocellular carcinoma (HCC) patients.
Methods:
This cohort study comprised 2559 HCC patients from different geographic regions, all treated with curative intent. We also examined the relation between indocyanine green (ICG) clearance and ALBI score. Survival was measured from the date of treatment to the date of death or last follow-up.
Results:
The ALBI score correlated well with ICG clearance. Among those undergoing surgical resection, patients with ALBI grade-1 (good liver function) survived approximately twice as long as those with ALBI grade-2 (less good liver function), although more than 90% of these patients were classified as Child–Pugh (C-P) grade A. In the cohort receiving ablative therapies, there was a similar difference in survival between ALBI grade-1 and grade-2. Cox regression analysis confirmed that the ALBI score along with age, gender, aetiology and tumour factors (AFP, tumour size/number and vascular invasion) independently influenced survival in HCC patients receiving curative treatments.
Conclusions:
The ALBI score represents a simple approach to the assessment of liver function in patients with HCC. After potentially curative therapy, those with ALBI grade-1 survived approximately twice as long as those with ALBI grade-2. These data suggest that ALBI grade-1 patients are appropriately treated with surgical resection whereas ALBI grade-2 patients may, where the option exists, be more suitable for liver transplantation or the less invasive curative ablative therapies.
Similar content being viewed by others
Main
The prognosis of patients with hepatocellular carcinoma (HCC) is influenced by several factors, the primary ones being related to the tumour itself and the underlying liver function, the latter usually being characterised by the Child–Pugh (C-P) score (Bruix and Sherman, 2005; European Association For The Study Of The Liver-European Organisation For Research and Treatment Of Cancer, 2012). Although potentially curative therapies for HCC are usually reserved for patients with C-P grade ‘A’ chronic liver disease (Bruix and Sherman, 2005; European Association For The Study Of The Liver-European Organisation For Research and Treatment Of Cancer, 2012), it is recognised that, within this single grade, there is a wide variation in the degree of hepatic reserve (Schneider, 2004; Seyama and Kokudo, 2009; Fan, 2010; Vauthey et al, 2010). For this reason, additional more sophisticated quantitative measures of liver function such as indocyanine green (ICG) clearance (Hemming et al, 1992) and hepatic venous pressure gradient (HVPG) measurements (Bruix et al, 1996; Thalheimer et al, 2004; Berzigotti et al, 2015) have been advocated. Such tests have been used predominantly to identify those patients in whom liver resection can be safely undertaken (i.e., to avoid periprocedural, ‘short-term’ mortality because of post-hepatectomy liver failure).
We have recently suggested that a new model, known as ‘ALBI’, can accurately assess liver (dys)function in patients with HCC and identify two distinct prognostic categories among C-P ‘A’ patients (Johnson et al, 2014). A simple formula, involving only albumin and bilirubin, generates an ‘ALBI score’ (ranging from −5 to 0.5, with higher scores representing worse liver function) and defined ranges are then applied to calculate a grade, from 1 to 3, with ‘one’ representing the best liver function and ‘three’ the worst (Johnson et al, 2014). In the first part, we provide evidence that the ALBI score can identify two distinct prognostic groups among C-P ‘A’ patients undergoing surgical resection or ablative therapies with curative intent and that can significantly affect long-term survival. In the second part of the present study, we examine how ICG clearance and HVPG correlate with the ALBI score. Such observations may have significant implications for surgical practice, specifically the choice between transplantation and surgical resection in circumstances under which both such options are available.
Materials and methods
The study is based on large individual patient cohorts recruited from major HCC centres as part of an international collaboration. Centres were chosen so as to generate a data set that reflected typical patients who undergo treatment with curative intent both in terms of the therapeutic options applied and the aetiology of the associated liver diseases.
Treatments were considered potentially curative if patients underwent surgical resection, radiofrequency ablation (RFA), microwave ablation (MWA) or, as in Western cohorts, liver transplantation. The latter was not offered at the Japanese and Hong Kong centres. The cohorts comprised 1072 patients from Japan where the aetiology was mainly chronic HCV infection, 738 from Hong Kong, where the aetiology was mainly chronic HBV infection, and 749 from the United Kingdom, Spain and Germany, merged under ‘Europe’, where the aetiology was mainly chronic HCV or alcohol abuse. Aetiology, treatment and other clinical characteristics of the cohorts are shown in Table 1. Aetiology is classified as HCV, HBV, HCV/HBV co-infection and ‘other’. The latter comprises alcoholic and fatty-liver disease, primary biliary cirrhosis, haemochromatosis and cryptogenic cirrhosis.
Of those undergoing surgical resection, 94.3% were graded as C-P ‘A’ by local investigators. The criteria for surgical resection in Eastern patients (Hong Kong and Japan) were: a 15-min ICG retention rate of <30%; single HCC, or not more than 3 HCCs, located in the same segment; <85 years of age; and absence of extrahepatic metastasis. The European centres in Spain, Germany, Birmingham and Newcastle followed BCLC guidelines for resection. The extent of surgical resection (major or minor) was available for the Hong Kong cohort only (Strasberg, 2005). Transplantation was undertaken according to the modified Milan Criteria. Within the guidelines listed above, the final treatment decision was based on a multidisciplinary team consensus in all regions. In the Japanese and Hong Kong cohorts, data were collected to permit assessment of changes in the ALBI score at 1, 3 and 6 months following resection and the degree of fibrosis (graded F0–F4) (Knodell et al, 1981) was available in all.
For patients undergoing surgical resection or liver transplantation, all patients had histological confirmation of the diagnosis; for those undergoing ablative therapies the diagnosis was based on internationally recommended criteria (Bruix and Sherman, 2005; European Association For The Study Of The Liver-European Organisation For Research and Treatment Of Cancer, 2012). Recurrence was assessed by serial imaging and AFP assessment, confirmed by biopsy in cases of doubt.
Correlation of the ALBI score with ICG clearance and HVPG was studied. Indocyanine green was presented as percentage retention at 15 min. Hepatic venous pressure gradient was measured in the 53 UK patients using a balloon occlusion catheter positioned in the right hepatic vein according to the technique described by Bosch et al (2009).
Post treatment antiviral therapies
After curative therapy, those Japanese HCV patients without specific contraindications (35% of the total HCV cohort) received conventional interferon-based antiviral therapy. Among those with HBV-related disease, 87% received a nucleoside analogue (lamivudine or, since 2102, entecavir). In Hong Kong, 15% of patients with HBV-related HCC received lamivudine. Very few (<5%) of the European patients received any form of antiviral therapy treatment. The cohorts were recruited before the availability of directly acting antivirals (DAAs) and there were few HBV-related cases.
The ALBI score
The ALBI score is a simple and objective measure of liver function and is applicable to HCC at all stages of chronic liver disease unlike the C-P score that is conventionally restricted to patients with cirrhosis. It is based on serum bilirubin and albumin and was derived from, and subsequently validated by, rigorous statistical analysis of over 6000 patients with HCC (Johnson et al, 2014).
The score is calculated from the formula,

Where bilirubin is in μmol l−1 and albumin in g l−1.
Specific cutoffs are then applied to generate three prognostic groups: ALBI score ⩽ −2.60 (ALBI grade-1), > −2.60 to ⩽−1.39 (ALBI grade-2) and ALBI score > −1.39 (ALBI grade-3).
The score and grade can be readily calculated from a ‘heat map’ given in the original publication (Johnson et al, 2014).
Statistical methods
All statistical analyses were undertaken using Stata IC 12 (StataCorp., TX, USA). Survival was measured from the time of treatment that was typically within 1 month of diagnosis. For continuous variables with extreme skewness, an appropriate transformation was applied. Correlations between the ALBI score and each of HVPG and ICG were analysed using the pairwise correlation coefficient (r). The ALBI score and grade was calculated for each cohort according to Johnson et al (2014) and discrimination between the grades was assessed by fitting Kaplan–Meier (KM) curves. The log-rank test was used to compare the survival distributions between the different grades. Cox regression models were fitted to derive hazard ratios and for testing the effect of ALBI on survival after adjusting for other factors in a multivariable model.
Results
Overall (Hong Kong, Japan and Europe), the 90-day mortality was <3% (breakdown of this result according to ALBI grade is shown in Table 1). Based on histological examination of resected HCC cases, 51.9% of Japanese and 44.2% of Hong Kong cases had fibrosis stage 4 (cirrhosis); the figures for ‘severe’ fibrosis (stage ⩾3) were 79% and 57.5% respectively (Table 1). Of the patients in the European cohort, 75% had stage 3 and 4 fibrosis. In a multivariable Cox regression model that included age, gender, tumour size, tumour number, AFP and vascular invasion, the ALBI score remained a strong predictor of survival (P<0.0001), even after adjusting for tumour-related factors (Supplementary Table 1). Within the entire group of 2559 patients, classification according to ALBI resulted in three clear and non-overlapping groups with median survival figures of 106.3 (95% CI 96.3, 122.7), 53.7 (95% CI 48.2, 58.6) and 26.9 (95% CI 20.4, 33.4) months in ALBI grade-1, -2 and -3 respectively (Figure 1).
Patients undergoing orthotopic liver transplantation
There was no significant difference in survival between the three ALBI grades after liver transplantation (log-rank test, P=0.68). At 5 years, survival for ALBI grade-1, -2 and -3 were 73.4% (95% CI 59.9, 83.1%), 67.3% (95% CI 58.1, 74.9%) and 73.3% (95% CI 58.0, 83.8%) respectively (Supplementary Figure 1).
Patients undergoing hepatic resection
Among the C-P grade A patients, two clear and non-overlapping ALBI subgroups emerged in each of the Japanese (log-rank test, P<0.0001), Hong Kong (log-rank test, P<0.0001) and European (log-rank test, P=0.0477) cohorts respectively (Figure 2). Survival was approximately twice as long in the ALBI grade-1 patients as in the ALBI grade-2 patients (Figure 2). For instance, ALBI grade-1 patients had median survival of 122.7 (95% CI 96.3, 148.7), not reached (or 5-year survival at 72.8%, 95% CI 66.5, 78.0) and 71.1 months (95% CI 59.0, 120.4) in the Japanese, Hong Kong and European patients respectively, whereas ALBI grade-2 survival was 71.2 (95% CI 56.2, 82.4), 44.5 (95% CI 28.6) and 42.3 months (95% CI 25.0, 69.5) in the same cohorts. The hazard ratio in ALBI grade-2 was twice that of ALBI grade-1 (Table 2). The better survival in ALBI grade-1 patients persisted in the subgroup of patients without tumour recurrence (Supplementary Figures 2a and b).
Among the Hong Kong patients, we assessed the impact of the ALBI grade according to the extent of resection. From those who underwent surgical resection (n=463), 263 and 200 received minor and major (three hepatic segments or more) resections respectively (Strasberg, 2005). In these patients, a clear distinction between ALBI grade-1 and grade-2 persisted (log-rank test, P=0.0002 and 0.0236 respectively) (Supplementary Figures 3a and b). Following resection, in both Japan and Hong Kong, there was a modest decrease in liver function (as assessed by ALBI) at 1 month followed by a return towards the preoperative score at 3 and 6 months (Supplementary Figure 4).
Patients undergoing RFA or MWA
Among those undergoing curative ablative therapies, ALBI grade-1 patients survived significantly longer than ALBI grade-2 in the Japanese, Hong Kong and European cohorts (log-rank test, P=0.0222, 0.0068 and 0.0011 respectively). In those cohorts, ALBI grade-1 median survivals were 84.2 (95% CI 63.8), 89.3 (95% CI 66.7, 115.8) and 56.5 months (95% CI 36.0, 69.2), whereas for ALBI grade-2 these were 56.1 (95% CI 48.6, 72.4), 59.2 (95% CI 47.2, 64.1) and 30.2 months (95% CI 27.4, 34.3) (Figure 3). The corresponding hazard ratios are also shown in Table 2. Patients with ALBI grade-3 showed the least survival in all three cohorts.
Survival by aetiology in patients undergoing curative treatment
When patients undergoing curative treatment were classified according to viral status, it was apparent that HBV-positive patients had a significantly better prognosis than HCV-positive patients in the Japanese, Hong Kong and European cohorts (log rank test, P<0.0001, 0.0056 and 0.0029 respectively) (Supplementary Figure 5). In the same order of cohorts, HBV-HCC median survival stood at 135.9 (95% CI 82.4, 168.1), 114.7 (95% CI 87.5) and not reached (or 5-year survival at 75.9%, 95% CI 61.7, 85.4), whereas HCV–HCC survival was 67.3 (95% CI 60.4, 74.5), 44.7 (95% CI 34.0, 69.8) and 71.9 months (95% CI 52.8, 90.2). In all, 68% of HBV–HCC patients fell into the ALBI grade-1 category as compared with only 33% of the HCV–HCC patients (Supplementary Table 2). It was notable that the survival curves only separated at between 2 and 3 years. Severe fibrosis or cirrhosis (F3 and F4) was more common in the HCV patients (82.2%) than in the HBV patients (65.2%) (Supplementary Table 3).
Median survival, 5-year survival and hazard ratio figures for all of the above are summarised in Table 2 and Supplementary Table 4).
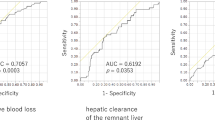
Correlation of ICG clearance and HVPG with ALBI score
Because of skewness of the ICG distribution, an appropriate transformation was used, in this case, the square root of each value. Among the patients with measured ICG, a strong positive correlation was observed with the ALBI score (r=0.6423, n=1346, P<0.0001; Figure 4A). There was also a positive correlation between HVPG and the ALBI score (r=0.55, n=52, P<0.0001; Figure 4B).
Discussion
International guidelines suggest that curative treatments, other than liver transplantation, should be confined to those with grade A C-P score in order to avoid the short-term complications associated with poor liver function (Schneider, 2004; Bruix and Sherman, 2005; Seyama and Kokudo, 2009; Fan, 2010; Vauthey et al, 2010; European Association For The Study Of The Liver-European Organisation For Research and Treatment Of Cancer, 2012). Such guidelines are refined by estimation of serum bilirubin and HVPG or ICG clearance (Hemming et al, 1992; Bruix et al, 1996; Thalheimer et al, 2004), whereas HVPG is often substituted for by ‘clinical evidence of portal hypertension’ (Berzigotti et al, 2015; Roayaie et al, 2015).
The present data confirm, and greatly extend, our original report that within C-P A grade there are two distinct subgroups as classified by the ALBI score. In all regions, among resected patients, survival was about twice as long among those with ALBI grade-1 than for those with ALBI grade-2. The overall survival results are remarkably consistent across regions. The rather worse survival in the European patients may be attributable to different practices when liver transplantation is an option. As expected, very few patients (<1%) with ALBI grade-3 were subjected to surgical resection. Similar results were obtained for those undergoing ablative therapies with curative intent. The degree of discrimination within C-P A is all the more remarkable for the fact that none of the clinical features related to the tumour itself that are perceived to influence survival (AFP, vascular invasion and tumour size) are taken into account. This implies that a very significant fraction of the mortality in HCC after potentially curative therapies, even in C-P ‘A’ patients, is attributable to liver dysfunction. The observation that clear separation between survivals curves of ALBI grade-1 and ALBI grade-2 persists in those patients without HCC recurrence (Supplementary Figure 2) may be taken to imply that much of the increased mortality in ALBI grade-2 is related to liver failure. There was little change in liver function after resection at 6 months, but we suspect that had more prolonged follow-up been available, separation between ALBI grade-1 and ALBI grade-2 would have become apparent. The observation that surgical resection and ablative therapies, but not transplant, are affected by the ALBI score would be expected if ALBI reflects liver function.
Our data also demonstrate a further advantage of the ALBI grade over the C-P scoring system in that it is equally applicable to HCC patients without cirrhosis. The ALBI score gave clear discrimination in each grade despite the fact that among patients with HBV-related HCC only 47.2% had cirrhosis (fibrosis stage 4) and even among the HCV patients the figure was only 56.6%. Conventionally, the C-P scoring system is restricted to patients with cirrhosis.
There is controversy concerning how to decide, in an individual patient, whether the most appropriate treatment is transplantation or surgical resection (where that option exists) (Michel et al, 1997; Sarasin et al, 1998; Figueras et al, 2000; Schwartz et al, 2007). It is widely agreed that transplantation is the preferred choice among patients with C-P B or C because such patients clearly have a higher risk of death from the associated liver disease. However, as noted above, we show that even within C-P ‘A’ there is a major difference in mortality between ALBI grade-1 and ALBI grade-2. Such information may influence the decision to transplant or resect: resection being, perhaps, more appropriate in ALBI grade-1 and transplantation in ALBI grade-2. We cannot be certain about the impact of postoperative antiviral therapy on our results. Current evidence suggests that rates of recurrence/development of ‘new’ tumours are probably decreased but definitive evidence is still awaited (Lok, 2012; Urata et al, 2012; Kim and Gores, 2013; Yin et al, 2013).
The ability to assess liver dysfunction accurately with the ALBI score before treatment may permit explanation of the findings of Franssen et al (2014) that HBV-positive patients survive significantly longer than those who are HCV positive. Analysis of our large international data set confirmed this finding and suggested that this may be attributable to differences in underlying liver function. More patients in the HBV-positive group in all regions were ALBI grade-1. This is consistent with the general consensus (and as shown in our results here; Supplementary Table 3) that HCC arises largely in the cirrhotic (or at least severely fibrotic) liver in HCV-positive patients, whereas it may also arise in the HBV-positive livers before the stage of cirrhosis has been reached (Shiratori et al, 1995; Grando-Lemaire et al, 1999; Kumar et al, 2007; Schuppan and Afdhal, 2008).
All the above interpretations assume that the ALBI score is a valid measure of liver dysfunction. Our initial publication provided circumstantial evidence that this was the case. Here, we adduce three further pieces of supportive evidence. Firstly, there was a positive correlation with ICG clearance, an objective test of liver function widely used in preoperative assessment. Secondly, in a smaller data set, there was also a correlation with HVPG, another parameter used in preoperative assessment. Finally, we hypothesised that in patients undergoing liver transplantation, preoperative liver function, as defined by the ALBI score, would have no impact on survival and, indeed, this was the case.
We now have objective evidence that the ALBI score assesses liver function in HCC patients. Although it is conventionally considered that assessment of liver function before resection is important to exclude patients who might develop liver failure if too large a resection is undertaken, we show here that the liver function also has a major impact on long-term survival. Such observations may have major implications for decisions as to whether surgery or liver transplantation is undertaken in HCC patients with compromised liver function.
Change history
29 March 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Berzigotti A, Reig M, Abraldes JG, Bosch J, Bruix J (2015) Portal hypertension and the outcome of surgery for hepatocellular carcinoma in compensated cirrhosis: a systematic review and meta analysis. Hepatology 61: 526–536.
Bosch J, Abraldes JG, Berzigotti A, García-Pagan JC (2009) The clinical use of HVPG measurements in chronic liver disease. Nat Rev Gastroenterol Hepatol 6: 573–582.
Bruix J, Castells A, Bosch J, Feu F, Fuster J, Garcia-Pagan JC, Visa J, Bru C, Rodes J (1996) Surgical resection of hepatocellular carcinoma in cirrhotic patients: prognostic value of preoperative portal pressure. Gastroenterology 111: 1018–1022.
Bruix J, Sherman M (2005) Management of hepatocellular carcinoma. Hepatology 42: 1208–1236.
European Association For The Study Of The Liver-European Organisation For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56: 908–943.
Fan ST (2010) Liver functional reserve estimation: state of the art and relevance for local treatments. J Hepatobiliary Pancreat Sci 17: 380–384.
Figueras J, Jaurrieta E, Valls C, Ramos E, Serrano T, Rafecas A, Fabregat J, Torras J (2000) Resection or transplantation for hepatocellular carcinoma in cirrhotic patients: outcomes based on indicated treatment strategy. J Am Coll Surg 190: 580–587.
Franssen B, Alshebeeb K, Tabrizian P, Marti J, Pierobon ES, Lubezky N, Roayaie S, Florman S, Schwartz ME (2014) Differences in surgical outcomes between hepatitis B-and hepatitis C–related hepatocellular carcinoma: a retrospective analysis of a single North American center. Ann Surg 260: 650–658.
Grando-Lemaire V, Guettier C, Chevret S, Beaugrand M, Trinchet J-C (1999) Hepatocellular carcinoma without cirrhosis in the West: epidemiological factors and histopathology of the non-tumorous liver. Groupe d'Etude et de Traitement du Carcinome Hépatocellulaire. J Hepatol 31: 508–513.
Hemming AW, Scudamore CH, Shackleton CR, Pudek M, Erb SR (1992) Indocyanine green clearance as a predictor of successful hepatic resection in cirrhotic patients. Am J Surg 163: 515–518.
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, O'beirne J, Fox R, Skowronska A, Palmer D (2014) Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 57: 9151.
Kim WR, Gores GJ (2013) Recurrent hepatocellular carcinoma: it's the virus!. J Clin Oncol 31: 3621–3622.
Knodell RG, Ishak KG, Black WC, Chen TS, Craig R, Kaplowitz N, Kiernan TW, Wollman J (1981) Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology 1: 431–435.
Kumar M, Kumar R, Hissar SS, Saraswat MK, Sharma BC, Sakhuja P, Sarin SK (2007) Risk factors analysis for hepatocellular carcinoma in patients with and without cirrhosis: a case-control study of 213 hepatocellular carcinoma patients from India. J Gastroenterol Hepatol 22: 1104–1111.
Lok AS (2012) Does antiviral therapy prevent recurrence of hepatitis B virus–related hepatocellular carcinoma after curative liver resection? JAMA 308: 1922–1924.
Michel J, Suc B, Montpeyroux F, Hachemanne S, Blanc P, Domergue J, Mouiel J, Gouillat C, Ducerf C, Saric J, Le Treut YP, Fourtanier G, Escat J (1997) Liver resection or transplantation for hepatocellular carcinoma? Retrospective analysis of 215 patients with cirrhosis. J Hepatol 26: 1274–1280.
Roayaie S, Jibara G, Tabrizian P, Park JW, Yang J, Yan L, Schwartz M, Han G, Izzo F, Chen M (2015) The role of hepatic resection in the treatment of hepatocellular cancer. Hepatology 62 (2): 440–451.
Sarasin FP, Giostra E, Mentha G, Hadengue A (1998) Partial hepatectomy or orthotopic liver transplantation for the treatment of resectable hepatocellular carcinoma? A cost-effectiveness perspective. Hepatology 28: 436–442.
Schneider PD (2004) Preoperative assessment of liver function. Surg Clin North Am 84: 355–373.
Schuppan D, Afdhal NH (2008) Liver cirrhosis. Lancet 371: 838–851.
Schwartz M, Roayaie S, Konstadoulakis M (2007) Strategies for the management of hepatocellular carcinoma. Nat Clin Pract Oncol 4: 424–432.
Seyama Y, Kokudo N (2009) Assessment of liver function for safe hepatic resection. Hepatol Res 39: 107–116.
Shiratori Y, Shiina S, Imamura M, Kato N, Kanai F, Okudaira T, Teratani T, Tohgo G, Toda N, Ohashi M (1995) Characteristic difference of hepatocellular carcinoma between hepatitis B-and C-viral infection in Japan. Hepatology 22: 1027–1033.
Strasberg SM (2005) Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 12: 351–355.
Thalheimer U, Mela M, Patch D, Burroughs AK (2004) Targeting portal pressure measurements: a critical reappraisal. Hepatology 39: 286–290.
Urata Y, Kubo S, Takemura S, Uenishi T, Kodai S, Shinkawa H, Sakae M, Kaneda K, Ohata K, Nozawa A (2012) Effects of antiviral therapy on long-term outcome after liver resection for hepatitis B virus-related hepatocellular carcinoma. J Hepatobiliary -Pancreat Sci 19: 685–696.
Vauthey JN, Dixon E, Abdalla EK, Helton WS, Pawlik TM, Taouli B, Brouquet A, Adams RB (2010) Pretreatment assessment of hepatocellular carcinoma: expert consensus statement. HPB (Oxford) 12: 289–299.
Yin J, Li N, Han Y, Xue J, Deng Y, Shi J, Guo W, Zhang H, Wang H, Cheng S (2013) Effect of antiviral treatment with nucleotide/nucleoside analogs on postoperative prognosis of hepatitis B virus–related hepatocellular carcinoma: A two-stage longitudinal clinical study. J Clin Oncol 48: 5896.
Acknowledgements
Author contributions
Study concept and design: PJJ, HT, JO’B, TK and PBSL; acquisition of data: HT, PBSL, CCC, JO’B, SB, HR, WY, TT, MI, AV, NS, SLC, BS and DM; analysis and interpretation of data: SB, HT, PBSL, JO’B, FM and RPF; drafting of the manuscript: PJJ, SB, HT and PBSL; critical revision of the manuscript for important intellectual content: all; statistical analysis: SB, RF and FM; obtained funding: none; administrative, technical or material support: none; study supervision: PJJ.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Toyoda, H., Lai, P., O'Beirne, J. et al. Long-term impact of liver function on curative therapy for hepatocellular carcinoma: application of the ALBI grade. Br J Cancer 114, 744–750 (2016). https://doi.org/10.1038/bjc.2016.33
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.33
Keywords
This article is cited by
-
Clinical Utility of Albumin Bilirubin Grade as a Prognostic Marker in Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization: a Systematic Review and Meta-analysis
Journal of Gastrointestinal Cancer (2023)
-
Albumin-Bilirubin Score at Post-Hepatectomy Hepatocellular Carcinoma Recurrence: Impact on Survival and Association with Post-Hepatectomy Liver Failure
Journal of Gastrointestinal Surgery (2023)
-
Novel combined fibrosis-based index predicts the long-term outcomes of hepatocellular carcinoma after hepatic resection
International Journal of Clinical Oncology (2022)
-
Microwave ablation versus surgical resection for subcapsular hepatocellular carcinoma: a propensity score–matched study of long-term therapeutic outcomes
European Radiology (2022)
-
Comparison of Survival Outcomes in Transarterial Ethanol Ablation and Liver Resection for Solitary Hepatocellular Carcinoma ≤ 5 cm in Patients Stratified by Liver Function
CardioVascular and Interventional Radiology (2022)