Abstract
Background:
Ethnic differences in cancer symptom awareness and barriers to seeking medical help in the English population are not fully understood. We aimed to quantify these differences, to help develop more effective health campaigns, tailored to the needs of different ethnic groups.
Methods:
Using a large national data set (n=38 492) of cross-sectional surveys that used the Cancer Research UK Cancer Awareness Measure, we examined how cancer symptom awareness and barriers varied by ethnicity, controlling for socio-economic position, age and gender. Data were analysed using multivariable logistic regression.
Results:
Awareness of cancer symptoms was lower in minority ethnic groups than White participants, with the lowest awareness observed among Bangladeshis and Black Africans. Ethnic minorities were more likely than White British to report barriers to help-seeking. South Asians reported the highest emotional barriers, such as lack of confidence to talk to the doctor, and practical barriers, such as worry about many other things. The Irish were more likely than the White British to report practical barriers, such as being too busy to visit a doctor. White British participants were more likely than any other ethnic group to report that they would feel worried about wasting the doctor’s time. Overall, Black Africans had the lowest barriers. All differences were statistically significant (P<0.01 level), after controlling for confounders.
Conclusions:
Our findings suggest the need for culturally sensitive and targeted health campaigns, focused on improving recognition of cancer symptoms among ethnic minorities. Campaigns should tackle the specific barriers prevalent in each ethnic group.
Similar content being viewed by others
Main
Britain is a multi-ethnic society, which has been described as a ‘super-diversity’ to reflect recent changes in its socio-demographic structure (Vertovec, 2007). The population with an ethnic minority background has doubled in size between 2001 and 2011 Census data collection (Office for National Statistics, 2012b). Super-diversity refers to a shift in recent immigration patterns, including a wider range of ethnicities from all over the world, and a dynamic interplay between factors such as religious and cultural behaviour norms, legal status and links with homeland (Vertovec, 2007). England has a higher percentage of ethnic minorities (14%) in comparison with Scotland (4%) and Wales (4%) (Scotland’s Census, 2011; Welsh Government, 2012; Office for National Statistics, 2012a).
Ethnic minorities in England are more likely than the White majority to have advanced stage at diagnosis, the key predictor of poor cancer survival (Velikova et al, 2004; Jack et al, 2009). Advanced stage at diagnosis is common among people with longer time to presentation after the onset of symptoms (Burgess et al, 2006). Low cancer symptom awareness and increased barriers to seeking medical help have been suggested as risk factors for longer time to presentation (Macleod et al, 2009). Some studies suggested that ethnic minorities have lower recognition of cancer symptoms (Scanlon and Wood, 2005; Waller et al, 2009), and more barriers to early symptomatic presentation than the majority population (Forbes et al, 2011). However, findings about ethnic differences in cancer awareness and barriers to help-seeking have not been consistent across studies.
Robb et al (2009) reported that ethnic minorities had lower cancer symptom awareness than White British people, which was not confirmed by Linsell et al (2008). While Robb et al (2009) found no ethnic differences in perception of barriers to help-seeking, another survey revealed several differences (Waller et al, 2009). For example, South Asian women had higher emotional barriers than other ethnic minorities, such as feeling embarrassed or not confident to talk to their general practitioner (GP). Black Africans had lower barriers than any other minority group, but other patterns were not clear (Waller et al, 2009). Evidence suggests that some barriers may be frequent among White British. In East London, White women were found to be more worried about wasting the doctor’s time than Black or South Asian women (Forbes et al, 2011). However, another London-based study did not identify this barrier among White women (Marlow et al, 2014), perhaps because older women (65+) were not interviewed. Marlow et al (2014) suggested that some barriers to presentation of breast or cervical cancer symptoms were common regardless of ethnicity, such as fear of cancer. Other barriers were more culture-specific, such as reluctance of Indian women to discuss female body parts.
Drawing firm conclusions from previous studies is difficult for a number of reasons: for example, a sample limited to a particular geographical area and women only (Forbes et al, 2011; Marlow et al, 2014); lack of a White comparison group (Waller et al, 2009); and, not a large enough sample size to examine individual ethnic groups, so all minorities were categorised as ‘Other’ (Robb et al, 2009). Such broad categorisation does not acknowledge the heterogeneity that exists within the ‘Other’ group. Even within each of the broad ethnic subgroups, such as ‘White’, ‘Black’ and ‘Asian’, there are many diverse cultural practices, social values and health behavioural patterns (Nazroo, 2003). In addition, previous studies have not thoroughly assessed the role of socio-economic position (SEP), which is closely intertwined and interdependent with ethnicity (Williams et al, 2012).
Awareness raising campaigns were introduced in England to encourage early cancer presentation (Cancer Research UK, 2015), but they were not targeted to meet the needs of the ethnically diverse population. A clear understanding of gaps in cancer awareness and barriers prevalent in each ethnic group is necessary to improve the effectiveness of these campaigns; and, to understand the patterns of advanced-stage diagnosis by ethnicity. Therefore, this study aimed to quantify ethnic differences in cancer symptom awareness and barriers to symptomatic presentation in the English population, to help develop more effective health campaigns, tailored to the needs of different ethnic groups.
Materials and methods
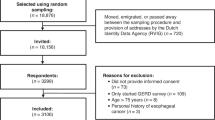
Cross-sectional surveys collected data across England, using the Cancer Research UK Cancer Awareness Measure (CAM) (Stubbings et al, 2009), during 2009/2011. Data from 18 surveys in total were collated into a uniquely large CAM data set (n=49 270). Just under half of all surveys (43%) were collected using random probability sampling frame, such as Royal Mail postcodes or UK Electoral Roll. The rest of the surveys (57%) were collected using non-random probability sampling techniques, such as approaching people on the street. We assigned each participant a measure of SEP, based on their postcode of residence and the income domain of indices of multiple deprivation, as previously described (Niksic et al, 2015). We classified participants into five groups of area income deprivation (ranging from 1—least deprived to 5—most deprived), based on quintiles in the English population (Department for Communities and Local Government, 2010). The same approach was used to calculate socio-economic deprivation groups, using the education and employment domain of the indices of multiple deprivation.
We excluded participants with missing information on gender (n=58), age (n=2431), area income deprivation (n=8151) and ethnicity (n=138). Ethnicity was self-reported, in response to a question: ‘Which of these best describes your ethnic group?’ We adopted the ethnic definitions of the 2011 Census for England to differentiate between the following nine ethnic groups: White British, White Irish, Indian, Pakistani, Bangladeshi, Chinese, Black African, Black Caribbean and Other (Office for National Statistics, 2012a). The ethnic group ‘Other’ included mixed race participants and those who described their ethnicity as ‘other’, including other White, other Asian and other Black backgrounds.
We used closed or prompted CAM questions, asking participants to recognise symptoms of cancer from the list of symptoms: ‘The following may or may not be warning signs for cancer. We are interested in your opinion’. The list of prompted questions included the following: ‘Do you think an unexplained lump or swelling could be a sign of cancer?’; ‘Do you think persistent unexplained pain could be a sign of cancer?’; ‘Do you think unexplained bleeding could be a sign of cancer?’; ‘Do you think a persistent cough or hoarseness could be a sign of cancer?’; ‘Do you think a persistent change in bowel or bladder habits could be a sign of cancer?’; ‘Do you think persistent difficulty swallowing could be a sign of cancer?’; ‘Do you think a change in the appearance of a mole could be a sign of cancer?’; ‘Do you think a sore that does not heal could be a sign of cancer?’; ‘Do you think unexplained weight loss could be a sign of cancer?’. Barriers to help-seeking were assessed using the questions: ‘Sometimes people put-off going to see the doctor, even when they have a symptom that they think might be serious. Could you say if any of these might put you off going to the doctor?’, and included the following: ‘I would be too embarrassed’; ‘I would be too scared’; ‘I would be worried about what the doctor might find’; ‘I would not feel confident talking about my symptom with the doctor’; ‘It would be difficult to make an appointment with my doctor’; ‘I would be too busy to make time to go to the doctor’; ‘I have too many other things to worry about’; ‘I would be worried about wasting the doctor’s time’; ‘It would be difficult for me to arrange transport to the doctor’s surgery’; ‘My doctor would be difficult to talk to’.
Analysis
We calculated cancer awareness and barriers scores by adding up ‘yes’ responses to the questions about cancer symptoms (range 0–9), and barriers to help-seeking (range 0–10), respectively. For example, a participant who recognised five potential cancer symptoms (five ‘yes’ responses) had cancer awareness score of five. Then we examined how cancer awareness and barriers scores varied between ethnic groups using Kruskal–Wallis tests. We examined the association between ethnic groups (independent variables) and both recognition of each cancer symptom and perception of each barrier to help-seeking (dependent variables), using logistic regression models. Because of multiple significance testing, the level of significance was set at P<0.01. The multivariable logistic regression models included a priori defined confounders: age, gender and SEP (presented in tables as area income deprivation).
We repeated the analyses using: (1) education and employment deprivation measures, instead of area income deprivation; (2) 12 ethnic groups, with Other White, Other Asian and Other Black backgrounds analysed separately; and, (3) data from the surveys that used random probability sampling only. All analyses were done using Stata 14.0 (STATA Corp, 2015).
Results
The distribution of gender, age and ethnic groups in our sample was similar to that of the general population of England (Table 1), with differences between our sample and the population often not larger than one percentage point (Office for National Statistics, 2012a). Overall more women responded to the survey; in most ethnic groups just over half of participants were females, with the exception of Pakistanis and Bangladeshis. People from South Asian and Black minority groups were more likely to live in the most socio-economically deprived areas, especially Pakistanis and Bangladeshis, in line with trends in the population as a whole. Ethnic minority groups were younger than White participants, which is what we would have expected from national data (Office for National Statistics, 2011).
Cancer awareness and barriers to help-seeking scores
We found statistically significant ethnic differences in cancer awareness and barriers scores (Table 2). White British and White Irish reported a higher average number of recognised symptoms in comparison with ethnic minority groups. We observed a trend of lower cancer awareness score with higher socio-economic deprivation among all ethnic groups. Overall, Black Africans had lower barriers score than all other ethnic groups. We found age and gender differences in awareness and barriers score for all ethnic groups, except Chinese and South Asians. Overall, women had the highest cancer awareness and barriers scores; 15–34-year olds had the lowest awareness scores, and 75+ year olds had the lowest barriers scores.
Participants who recognised all nine symptoms, considered to be highly aware of cancer symptoms, by ethnic group were: 44% White British, 39% White Irish, 29% Other, 24% Chinese, 23% both Black Caribbean and Indian, 22% Pakistani, 20% Black African and 16% Bangladeshi participants. Participants who identified three or more reasons that would deter them from seeking medical attention were considered to have above-average barriers to help-seeking. These were, by ethnic group: 39% Indian, 37% Bangladeshi, 36% Chinese, 34% Pakistani, 33% Other, 33% White Irish, 29% White British, and 28% for both Black Caribbean and Black African participants.
Recognition of individual cancer symptoms
Ethnic minority groups were less likely to recognise each cancer symptom than White participants, and adjustment for age, gender and area income deprivation, made little difference to the results (Table 3). Unadjusted results are available in Supplementary Material 1. Black African and Bangladeshi participants least frequently recognised each cancer symptom, except a ‘sore that does not heal’ (Table 3). Chinese participants had the lowest recognition of this symptom, with 49% lower odds of recognising it compared with White British (OR=0.51; 99% CI: 0.34–0.76). The most frequently recognised symptom was an ‘unexplained lump or swelling’ (94% of all participants), which Bangladeshi participants recognised less frequently than any other ethnic group (77%). Bangladeshis had almost seven times lower odds of recognising lump as a symptom of cancer than White British (OR=0.15; 99% CI: 0.11–0.21). The largest difference between ethnic minorities and White British was in recognition of ‘change in the appearance of a mole’, which was recognised by only 59% of Bangladeshis compared with 94% of White British participants. ‘Persistent cough or hoarseness’ was another symptom with low recognition; recognised by only 51% of Black Africans, in comparison with 70% of White British. Black Africans had significantly lower odds of recognising this symptom than White British (OR=0.55; 99% CI: 0.46–0.66).
Sensitivity analyses using area-level education or employment deprivation measures, instead of area income deprivation, hardly modified the results shown in Table 3 (results available on request). The results were also similar when 12 ethnic groups were analysed separately (Supplementary Material 2). Furthermore, restricting the analysis to the data collected via random probability sampling did not change Table 3 results (results available on request), suggesting they were not affected by the survey design.
Perception of individual barriers to help-seeking
Ethnic minority groups were generally more likely to identify barriers to presentation than White participants, and adjustment for age, gender and area income deprivation made little difference to the results (Table 4). Unadjusted results are available in Supplementary Material 3. In general, South Asians reported barriers to help-seeking more frequently than other ethnic groups (Table 4). Emotional barriers were the most common, reported by approximately a quarter of all South Asians, but slightly more frequently by Indian participants. Pakistanis had 51% higher odds of reporting embarrassment (OR=1.51; 99% CI: 1.17–1.93); while Indian participants had two-fold higher odds of reporting lack of ‘confidence to talk about their symptoms with the doctor’ (OR=2.03; 99% CI: 1.60–2.57), in comparison with White British. Practical barriers were also widespread, as over a quarter of South Asians reported being ‘worried about many other things’ (28%), and being ‘too busy’ to visit a doctor (24–31%).
Black participants had the lowest barriers, especially Black Africans. For example, they had 57% lower odds than White British of reporting that ‘worry about wasting the doctor’s time’ would be a barrier to help-seeking (OR=0.43; 99% CI: 0.33–0.55). Chinese participants most frequently reported that they would find it ‘difficult to talk’ to the GP about their symptoms (23%). White Irish had 68% higher odds than White British of reporting that being ‘too busy’ would put them off going to the doctor (OR=1.68; 99% CI: 1.26–2.23). White British participants were significantly more likely than any other ethnic group to report that they would be ‘worried about wasting the doctor’s time’. A quarter (25%) of White British reported this barrier in comparison with, for example, 18% of Black Caribbeans.
The most commonly reported barriers to seeking medical help were ‘worry about what the doctor might find’ (30%), and finding it ‘difficult to make an appointment’ (28%). We found no statistically significant differences between ethnic groups in relation to these barriers, or for being ‘too scared’ (borderline significance observed only for the ‘Other’). The only exception were Black Africans, who were significantly less likely than White British to report being too scared and having difficulties to make an appointment (Table 4). All minority ethnic groups, except Black Caribbeans, were more likely than White British to report that they would find it ‘difficult to arrange transport’ to the doctor’s surgery. We obtained similar results as those in Table 4 when using area level education or employment deprivation measures, instead of area income deprivation (results available on request), or when analysing 12, instead of 9, ethnic groups (Supplementary Material 4), or when we included data collected via random probability sampling only (results available on request).
Discussion
Main findings
Ethnic minorities had lower symptom awareness and more widespread barriers to seeking medical help than White participants. Bangladeshis and Black Africans were least likely to recognise cancer symptoms. South Asians reported increased emotional and practical barriers. White British were more likely than any other ethnic group to report that they would feel worried about wasting the doctor’s time. Black participants, especially Africans, were least likely to report barriers to seeking medical help. These results were stable after controlling for potential confounders, suggesting that ethnicity has an independent effect on cancer awareness and barriers to help-seeking.
Strengths and limitations
This is the largest study to assess ethnic differences in public cancer awareness and barriers to help-seeking in England; and, the first study to assess this question using a sample broadly representative of the general population, with fairly large groups within ethnic minorities. Our sample allowed us to examine differences within White, Black and South Asian minority groups as defined by the most recent Census classification (2011), using nine different ethnic groups. This meant that we could improve our understanding of cancer awareness and barriers to help-seeking within each ethnic group. Given our large sample, our results were more precise than those in previous studies. The stability and robustness of the results were confirmed by sensitivity analyses, and by controlling for key potential confounding factors—age, gender and socio-economic deprivation.
Possible limitations relate to the use of general CAM questionnaire, which did not allow a more in-depth investigation of awareness about, for example, breast or lung cancer symptoms only. Therefore, our cancer awareness score refers to the recognition of a range of possible cancer symptoms. However, it is necessary to quantify which symptoms of the most common types of cancer are adults from different ethnic groups in England able to recognise, prior to investigating site-specific cancer awareness. Some ethnic groups may have a greater propensity to give ‘socially desirable’ answers, as an attempt to present themselves in a better light (Bowling, 2002). For example, being ‘too busy’ may be seen as more aspirational and socially desirable among ethnic groups, such as the Chinese, who are stereotypically perceived as particularly hard-working. During interviews all participants were reassured of confidentiality and anonymity, which may have reduced social desirability bias. Approximately 50% of data on educational attainment were missing for participants from ethnic minority groups, and therefore, we did not include it in our analysis.
The CAM questionnaire did not include questions about country of birth or whether participants were first-, second- or third-generation immigrants. Therefore, we were not able to compare these subgroups. All participants in our sample were currently resident in England. We assumed that for most participants their self-defined ethnicity reflects their national identity, which may or may not relate to their country of birth. National identity is a multi-dimensional and subjective construct, which allows people to express which country they feel most affiliated to (Office for National Statistics, 2012b), and how they understand their rights, constraints and opportunities (Norton, 1997). It is possible that national identity is more important than country of birth in shaping health attitudes and behaviour of different ethnic groups, especially in second-generation immigrants. This question, however, is beyond the scope of our study and within the realm of medical anthropology. Finally, some people may prefer recourse to their culturally specific medical practices and traditional healing methods, and avoid the NHS altogether, in which case these barriers may not be applicable to them.
Comparison with existing literature
Only a few studies have addressed this research question using a validated questionnaire and including all major ethnic groups in the population. We confirmed the previous finding that ethnic minorities in the United Kingdom tend to have poor cancer awareness (Waller et al, 2009), and are less likely to recognise cancer symptoms than White British people (Robb et al, 2009; Forbes et al, 2011; Quaife et al, 2013). This pattern has also been observed in the United States, where African Americans and Hispanic people tend to lack knowledge about cancer symptoms and have numerous misconceptions about cancer (Suarez et al, 1997; Barroso et al, 2000; Shokar et al, 2005). Rauscher et al (2010) found more misconceptions about breast lumps among African American and Hispanic women than White American breast cancer patients. These misconceptions were, for example, that pressing or touching the breast lump will cause it to become breast cancer, that one needs to get a lump checked only if it is painful, or only if it is growing. Evidence suggests that people born outside of Australia, such as in Asia or Middle East, have poorer knowledge about symptoms of colorectal cancer than Australian-born people (Koo et al, 2010). These differences might emerge from the nature of health campaigns, which do not necessarily take account of specific needs and cultural norms of smaller ethnic groups, because they are usually generic and designed for the majority.
Our findings contrast with studies suggesting that White and ethnic minority groups in England equally endorse barriers to help-seeking (Robb et al, 2009). The only exception was that Robb et al (2009) found that 40% of White British and only 24% of ethnic minorities reported being worried about wasting the doctor’s time. We found similar trends, but with highly statistically significant differences. Waller et al (2009) found that worry about wasting the doctor’s time was the most common barrier (41%) among ethnic minorities in England as opposed to White British in our study; and that the Chinese had the highest barriers to help-seeking rather than the South Asians in our study. These inconsistencies may be due to the lack of adjustment for relevant confounding factors (Robb et al, 2009) or smaller sample sizes, and therefore lower power in previous studies.
Ethnic minorities in our study, with the exception of the Irish, described their ethnicity as, for example, Pakistani, Bangladeshi or Chinese. According to the UN (2014) classification, these ethnic groups originally come from a range of developing, low- or middle-income countries. A high-income country, such as England, invests disproportionally more resources on preventive and health services than, for example, Bangladesh. This may explain partly why ethnic minorities had lower cancer awareness than the White majority. More specifically, the lowest cancer awareness was observed for participants from arguably the poorest, low-income countries, such as the Sub-Saharan Africa and Indian subcontinent (World Bank, 2015).
Interestingly, some barriers were widespread among all ethnic groups in our sample, such as worry about what the doctor might find. We also did not observe ethnic differences in feeling ‘too scared’ to visit a doctor, with the exception of Black Africans. Fear of cancer diagnosis may be the underlying emotion behind these two barriers, because people may experience fear if they think that their medical examination could result in cancer diagnosis. However, evidence about the association between this fear and help-seeking behaviour is contradictory (Balasooriya-Smeekens et al, 2015). For example, some studies found that fear of cancer diagnosis was associated with longer time to presentation of symptomatic breast cancer (Nosarti et al, 2000; Burgess et al, 2006), others found that this fear was associated with shorter time to presentation (O’Mahony et al, 2013), and some studies found no evidence of this association (Friedman et al, 2006). It is possible that fear of cancer diagnosis may act as a motivator or barrier to seeking medical help, depending on its intensity, duration, context, coping skills and socio-demographic characteristics of an individual.
Indian participants had slightly higher emotional barriers than Bangladeshis and Pakistanis, but overall their results were similar. These three ethnic groups often share a range of similar traditional values, such as placing priority on family in dealing with matters of individual choice: the selection of clothes to wear, which university to attend, and whom to marry (Dale et al, 2002). Such decisions are likely to be the subject of negotiation within the family. Help-seeking behaviour may be closely related to ‘izzat’, which refers to maintaining family honour, and fear of bringing shame to the family (Gilbert et al, 2004). In one example, izzat was considered more imperative than doctor–patient confidentiality—some South Asian women expressed fears that the GP might speak to the family about their symptoms, particularly if the GP shared the same ethnic background or was a family friend (Gilbert et al, 2004). However, having a doctor from a different ethnic background could introduce different types of problems, including language barriers or difficulty in understanding specific socio-cultural values, which may be embedded in medical consultations.
Black participants, especially Africans, least frequently reported barriers to presentation, which may reflect more assertive attitudes towards health-care services. Chinese participants were most likely to perceive difficulties in talking about their symptoms with the doctor, and difficulties in arranging transport to the surgery. Liang et al (2004) found the same barriers among Chinese Americans. They also reported the ability to speak English as a key barrier, followed by the need for help with transportation. Learning the English language is likely to be a challenge for Chinese native speakers, considering fundamental differences between an alphabetic and a logographic system. Such difficulties are likely to affect the complex navigation in the primary and secondary health care, and the navigation of the UK public transport system, which is only signposted in English.
White British, as well as the Irish, were more likely than any other ethnic group to report that being worried about wasting the doctor’s time would deter them from seeking help, which confirmed and expanded previous findings (Forbes et al, 2011). The British stiff upper lip attitude and determination to remain stoical, despite a real threat that symptoms might be malignant, may influence help-seeking behaviour of the White majority. Scanlon et al (2006) revealed the same barrier during the interviews with both White British and Irish participants, who felt that they should not visit their doctor because their ‘needs are not important enough’ or they did not want to ‘make a fuss’. The Irish reported more barriers related to socio-economic factors, such as more stress due to working hard to establish themselves abroad, and working in difficult conditions, which led them to neglect their health. Similarly, we observed more practical barriers, such as being too busy, among Irish than White British. Some people feel reluctant to appear to be overusing valuable NHS resources, in the light of recent concerns that NHS cannot effectively provide medical services to an increasingly elderly population.
An additional consideration is necessary before implementing these findings. Ethnic differences in cancer survival are not fully understood, and they might be attributable to the differences in socio-economic deprivation. While studies done in the United States (Ward et al, 2004; Newman et al, 2006) support the proposition that ethnic minorities have worse cancer survival than the majority population after controlling for deprivation, recent studies done in the United Kingdom (Maringe et al, 2015; Morris et al, 2015) and New Zealand (McKenzie et al, 2011) do not support this. The inconsistency might be due to methodological differences between the studies, or the fact that the NHS in the United Kingdom is free for everyone at the point of access. The NHS has no record about the exact number of minorities, such as elderly South Asian cancer patients who return to their home country to die, which may bias the survival estimates. However, even with limited effects on cancer survival, efforts to improve cancer awareness and encourage help-seeking in different ethnic groups may be beneficial for early diagnosis.
Implications and conclusion
Future studies should explore reasons why different ethnic groups report specific barriers to help-seeking, the meaning attached to each barrier, the effects of educational attainment and literacy skills, and the role of language and religion in cancer symptom awareness and barriers to help-seeking. Differences in cancer awareness and barriers between recent immigrants, and the first or subsequent generation immigrants should also be explored. The role of fear of cancer diagnosis in help-seeking behaviour of people with different socio-demographic and ethnic background requires further attention. Understanding ethnic differences in awareness about specific cancer sites, using Lung or Colorectal Cancer Awareness Measure, would also be useful. Prior to developing campaigns tailored to meet the needs of ethnically diverse population, it is essential to pilot these campaigns and evaluate their impact on early diagnosis and cancer survival.
Our findings are directly applicable to England, but it is likely that they may be extrapolated to the other developed, ethnically diverse countries with similar health-care system, which is free for everyone at the point of access. The findings may contribute to the NHS goals to reduce ethnic inequalities in cancer health (Department of Health, 2011). The term ‘socially sensitive’ has often been used to denote campaigns adjusted to suit the culturally specific needs of minority ethnic groups only. We suggest the expansion of this term to include the culturally specific needs of both the ethnic minority and the majority population.
Most campaigns aimed at encouraging early cancer presentation are not targeted to meet different needs of ethnically diverse population in England. We recommend the development of targeted campaigns to address these needs, while acknowledging the nuance within and between each ethnic group. Cultural competence, defined as an ‘awareness of the cultural factors that influence another’s views and attitudes’ (Napier et al, 2014), needs to be introduced into health-care practice and campaigns. Ethnic minorities could benefit from educational campaigns aimed at improving their recognition of cancer symptoms (Scanlon et al, 2006; Forbes et al, 2011). South Asians may benefit most from campaigns aimed at alleviating their emotional barriers, by providing support and encouragement to discuss their symptoms, using culturally sensitive language and local community organisations (Netto et al, 2010). Practical barriers should be addressed among South Asians, the Irish and the Chinese, by clear educational messages that health should not be neglected (Scanlon and Wood, 2005; Scanlon et al, 2006), and by informing people of health services available nearby their place of work. Black people may benefit most from campaigns aimed at raising their cancer symptom awareness. These campaigns should address their misconceptions about cancer, with the assistance of religious and spiritual leaders (Koffman et al, 2008; Banning, 2011). Empathy and reassurance may be useful to address inhibitions of the majority population, such as the idea that going to the doctor will waste the doctor’s time (Forbes et al, 2011). Without tackling this barrier it may not be possible to improve cancer survival rates in England. The development of targeted and culturally sensitive cancer awareness campaigns is likely to improve early presentation among all ethnic groups in England.
References
Balasooriya-Smeekens C, Walter FM, Scott S (2015) The role of emotions in time to presentation for symptoms suggestive of cancer: a systematic literature review of quantitative studies. Psychooncology 24 (12): 1594–1604.
Banning M (2011) Black women and breast health: a review of the literature. Eur J Oncol Nurs 15 (1): 16–22.
Barroso J, McMillan S, Casey L, Gibson W, Kaminski G, Meyer J (2000) Comparison between African-American and white women in their beliefs about breast cancer and their health locus of control. Cancer Nurs 23 (4): 268–276.
Bowling A (2002) Research Methods in Health: Investigating Health and Health Service 2nd edn Open University Press: Buckingham and Philadelphia.
Burgess CC, Potts HWW, Hamed H, Bish AM, Hunter MS, Richards MA, Ramirez AJ (2006) Why do older women delay presentation with breast cancer symptoms? Psychooncology 15 (11): 962–968.
Cancer Research UK (2015) Be Clear on Cancer. Available at http://www.cancerresearchuk.org/health-professional/early-diagnosisactivities/be-clear-on-cancer (accessed on 12 April 2015).
Dale A, Shaheen N, Kalra V, Fieldhouse E (2002) Routes into education and employment for young Pakistani and Bangladeshi women in the UK. Ethn Racial Stud 25 (6): 942–968.
Department for Communities and Local Government (2010) The English Indices of Deprivation 2010.
Department of Health (2011) Assessment of the Impact on Equalities (AIE). Published Alongside Improving Outcomes: A Strategy for Cancer. Department of Health: London.
Forbes LJL, Atkins L, Thurnham A, Layburn J, Haste F, Ramirez AJ (2011) Breast cancer awareness and barriers to symptomatic presentation among women from different ethnic groups in East London. Br J Cancer 105 (10): 1474–1479.
Friedman LC, Kalidas M, Elledge R, Dulay MF, Romero C, Chang J, Liscum KR (2006) Medical and psychosocial predictors of delay in seeking medical consultation for breast symptoms in women in a public sector setting. J Behav Med 29 (4): 327–334.
Gilbert P, Gilbert J, Sanghera J (2004) A focus group exploration of the impact of izzat, shame, subordination and entrapment on mental health and service use in South Asian women living in Derby. Mental Health Relig Cult 7 (2): 109–130.
Jack RH, Davies EA, Moller H (2009) Breast cancer incidence, stage, treatment and survival in ethnic groups in South East England. Br J Cancer 100 (3): 545–550.
Koffman J, Morgan M, Edmonds P, Speck P, Higginson IJ (2008) ‘I know he controls cancer’: the meanings of religion among Black Caribbean and White British patients with advanced cancer. Soc Sci Med 67 (5): 780–789.
Koo JH, Arasaratnam MM, Liu K, Redmond DM, Connor SJ, Sung JJ, Leong RW (2010) Knowledge, perception and practices of colorectal cancer screening in an ethnically diverse population. Cancer Epidemiol 34 (5): 604–610.
Liang W, Yuan E, Mandelblatt JS, Pasick RJ (2004) How do older Chinese women view health and cancer screening? Results from focus groups and implications for interventions. Ethn Health 9 (3): 283–304.
Linsell L, Burgess CC, Ramirez AJ (2008) Breast cancer awareness among older women. Br J Cancer 99: 1221–1225.
Macleod U, Mitchell ED, Burgess C, MacDonald S, Ramirez AJ (2009) Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. Br J Cancer 101: s92–s101.
Maringe C, Li R, Mangtani P, Coleman M, Rachet B (2015) Cancer survival differences between South Asians and non-South Asians of England in 1986–2004, accounting for age at diagnosis and deprivation. Br J Cancer 113 (1): 173–181.
Marlow LA, McGregor LM, Nazroo JY, Wardle J (2014) Facilitators and barriers to help-seeking for breast and cervical cancer symptoms: a qualitative study with an ethnically diverse sample in London. Psychooncology 23 (7): 749–757.
McKenzie F, Ellison-Loschmann L, Jeffreys M (2011) Investigating reasons for ethnic inequalities in breast cancer survival in New Zealand. Ethn Health 16 (6): 535–549.
Morris M, Woods L, Rogers N, O’Sullivan E, Kearins O, Rachet B (2015) Ethnicity, deprivation and screening: survival from breast cancer among screening-eligible women in the West Midlands diagnosed from 1989 to 2011. Br J Cancer 113 (3): 548–555.
Napier A, Ancarno C, Butler B, Calabrese J, Chater A, Chatterjee H, Guesnet F, Horne R, Jacyna S, Jadhav S (2014) Culture and health. The Lancet and University College London commission on culture and health. Lancet 384 (9954): 1607–1639.
Nazroo JY (2003) The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health 93 (2): 277–284.
Netto G, Bhopal R, Lederle N, Khatoon J, Jackson A (2010) How can health promotion interventions be adapted for minority ethnic communities? Five principles for guiding the development of behavioural interventions. Health Promot Int 25 (2): 248–257.
Newman LA, Griffith KA, Jatoi I, Simon MS, Crowe JP, Colditz GA (2006) Meta-analysis of survival in African American and White American patients with breast cancer: ethnicity compared with socioeconomic status. J Clin Oncol 24 (9): 1342–1349.
Niksic M, Rachet B, Warburton F, Wardle J, Ramirez A, Forbes L (2015) Cancer symptom awareness and barriers to symptomatic presentation in England–are we clear on cancer? Br J Cancer 113 (3): 533–542.
Norton B (1997) Language, identity, and the ownership of English. TESOL Quart 31 (3): 409–429.
Nosarti C, Crayford T, Roberts J, Elias E, McKenzie K, David A (2000) Delay in presentation of symptomatic referrals to a breast clinic: patient and system factors. Br J Cancer 82 (3): 742–748.
O’Mahony M, McCarthy G, Corcoran P, Hegarty J (2013) Shedding light on women’s help seeking behaviour for self discovered breast symptoms. Eur J Oncol Nurs 17 (5): 632–639.
Office for National Statistics (2011) 2011 Census Data for England DC2101EW–Ethnic Group by Sex by Age. Available at https://www.nomisweb.co.uk/census/2011/DC2101EW/view/2092957699?rows=c_age&cols=c_ethpuk11 (accessed on 11 February 2015).
Office for National Statistics (2012a) 2011 Census: Population Estimates for England–Ethnic Group (All Usual Residents). Available at http://www.nomisweb.co.uk/census/2011/KS201EW/view/2092957699?cols=measures (accessed on 11 October 2013).
Office for National Statistics (2012b) Ethnicity and National Identity in England and Wales 2011. Available at http://www.ons.gov.uk/ons/dcp171776_290558.pdf (accessed on 11 October 2014).
Quaife SL, Forbes LJL, Ramirez AJ, Brain KE, Donnelly C, Simon AE, Wardle J (2013) Recognition of cancer warning signs and anticipated time to help-seeking in a population sample of adults in the UK. Br J Cancer 110: 12–18.
Rauscher GH, Ferrans CE, Kaiser K, Campbell RT, Calhoun EE, Warnecke RB (2010) Misconceptions about breast lumps and delayed medical presentation in urban breast cancer patients. Cancer Epidemiol Biomark Prev 19 (3): 640–647.
Robb KA, Stubbings S, Ramirez A, Macleod U, Austoker J, Waller J, Hiom S, Wardle J (2009) Public awareness of cancer in Britain: a population based survey in adults. Br J Cancer 101: s18–s23.
Scanlon K, Harding S, Hunt K, Petticrew M, Rosato M, Williams R (2006) Potential barriers to prevention of cancers and to early cancer detection among Irish people living in Britain: a qualitative study. Ethn Health 11 (3): 325–341.
Scanlon K, Wood A (2005) Breast cancer awareness in Britain: are there difference based on ethnicity? Divers Health Social Care 2: 211–221.
Scotland’s Census (2011) Ethnicity, Identity, Language and Religion. Available at http://www.scotlandscensus.gov.uk/ethnicity-identity-language-and-religion (accessed on 15 February 2016).
Shokar NK, Vernon SW, Weller SC (2005) Cancer and colorectal cancer: knowledge, beliefs, and screening preferences of a diverse patient population. Fam Med 37 (5): 341–347.
STATA Corp (2015) Stata 14.0 Statistical Software. College Station: Texas.
Stubbings S, Robb KA, Waller J, Ramirez A, Austoker J, Macleod U, Hiom S, Wardle J (2009) Development of a measurement tool to assess public awareness of cancer. Br J Cancer 101: s13–s17.
Suarez L, Roche RA, Nichols D, Simpson DM (1997) Knowledge, behavior, and fears concerning breast and cervical cancer among older low-income Mexican-American women. Am J Prev Med 13 (2): 137.
UN (2014) Country Classification (Statistical Annex). World Economic Situation and Prospects (WESP). Available at http://www.un.org/en/development/desa/policy/wesp/wesp_current/2014wesp_country_classification.pdf (accessed on 10 February 2015).
Velikova G, Booth L, Johnston C, Forman D, Selby P (2004) Breast cancer outcomes in South Asian population of West Yorkshire. Br J Cancer 90 (10): 1926–1932.
Vertovec S (2007) Super-diversity and its implications. Ethn Racial Stud 30 (6): 1024–1054.
Waller J, Robb KA, Stubbings S, Ramirez A, Macleod U, Austoker J, Hiom S, Wardle J (2009) Awareness of cancer symptoms and anticipated help-seeking among ethnic minority groups in England. Br J Cancer 101: s24–s30.
Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, Thun M (2004) Cancer Disparities by Race/Ethnicity and Socioeconomic Status. CA Cancer J Clin 54 (2): 78–93.
Welsh Government (2012) 2011 Census: First Results for Ethnicity, National Identity, and Religion for Wales. Available at http://gov.wales/docs/statistics/2012/121217sb1262012en.pdf (accessed on 22 February 2016).
Williams DR, Kontos EZ, Viswanath K, Haas JS, Lathan CS, MacConaill LE, Chen J, Ayanian JZ (2012) Integrating multiple social statuses in health disparities research: the case of lung cancer. Health Serv Res 47 (3pt2): 1255–1277.
World Bank (2015) Low Income Countries. Available at http://data.worldbank.org/income-level/LIC (accessed on 14 January 2015).
Acknowledgements
This study is part of a PhD programme funded by the Policy Research Unit in Cancer Awareness, Screening, and Early Diagnosis, which in turn receives funding from the Department of Health Policy Research Programme. It is collaboration between researchers from seven institutions: Queen Mary University of London, UCL, King's College London, London School of Hygiene and Tropical Medicine, Hull York Medical School, Durham University, and Peninsula Medical School. We would also like to acknowledge our great debt to Professor Jane Wardle (University College London), whose helpful feedback to the conference abstracts and interesting discussions have contributed to shaping this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
This work is licensed under the Creative Commons Attribution-Non-Commercial-Share Alike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Niksic, M., Rachet, B., Warburton, F. et al. Ethnic differences in cancer symptom awareness and barriers to seeking medical help in England. Br J Cancer 115, 136–144 (2016). https://doi.org/10.1038/bjc.2016.158
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.158
Keywords
This article is cited by
-
What do cancer survivors believe caused their cancer? A secondary analysis of cross-sectional survey data
Cancer Causes & Control (2024)
-
The UK public and healthcare professionals' awareness of mouth cancer
British Dental Journal (2023)
-
Differences in cancer incidence by broad ethnic group in England, 2013–2017
British Journal of Cancer (2022)
-
Clinical profile, risk factors and functional outcomes in women and men presenting with hip fractures in KwaZulu-Natal, South Africa
Archives of Osteoporosis (2022)
-
Perceived barriers to seeking cancer care in the Gaza Strip: a cross-sectional study
BMC Health Services Research (2021)