Abstract
Background:
The relationship between statin use and non-melanoma skin cancer (NMSC) is unclear with conflicting findings in literature. Data from the Women’s Health Initiative (WHI) Observational Study and WHI Clinical Trial were used to investigate the prospective relationship between statin use and NMSC in non-Hispanic white (NHW) postmenopausal women.
Methods:
The WHI study enrolled women aged 50–79 years at 40 US centres. Among 133 541 NHW participants, 118 357 with no cancer history at baseline and complete medication/covariate data comprised the analytic cohort. The association of statin use (baseline, overall as a time-varying variable, duration, type, potency, lipophilicity) and NMSC incidence was determined using random-effects logistic regression models.
Results:
Over a mean of 10.5 years of follow-up, we identified 11 555 NMSC cases. Compared with participants with no statin use, use of any statin at baseline was associated with significantly increased NMSC incidence (adjusted odds ratio (ORadj) 1.21; 95% confidence interval (CI): 1.07–1.35)). In particular, lovastatin (OR 1.52; 95% CI: 1.08–2.16), simvastatin (OR 1.38; 95% CI: 1.12–1.69), and lipophilic statins (OR 1.39; 95% CI: 1.18–1.64) were associated with higher NMSC risk. Low and high, but not medium, potency statins were associated with higher NMSC risk. No significant effect modification of the statin–NMSC relationship was found for age, BMI, smoking, solar irradiation, vitamin D use, and skin cancer history.
Conclusions:
Use of statins, particularly lipophilic statins, was associated with increased NMSC risk in postmenopausal white women in the WHI cohort. The lack of duration–effect relationship points to possible residual confounding. Additional prospective research should further investigate this relationship.
Similar content being viewed by others
Main
Non-melanoma skin cancer (NMSC), which includes basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), is the most common cancer in the United States and is responsible for significant economic costs (Rogers et al, 2010; National Cancer Institute, 2012). Although NMSC is more common among men than women, the incidence has rapidly increased for both genders (Christenson et al, 2005; Rogers et al, 2010). Well-established NMSC risk factors include ultraviolet radiation from sun or tanning bed exposure (Gallagher et al, 1995; van Dam et al, 1999), increasing age (Gray et al, 1997; Karagas et al, 1999), immunosuppression (particularly for SCCs) (Lichter et al, 2000), and light skin (Hussain et al, 2009).
In laboratory studies, statins (3-hydroxy-3 methylglutaryl coenzyme A, HMG-CoA reductase inhibitors) have appeared to protect against NMSC by causing apoptosis of keratinocytes by lowering cellular cholesterol levels (Gniadecki, 2004) and activating the RAFMEK (mitogen-activated protein kinase 1) pathway (Wu et al, 2004). Furthermore, cholesterol depletion because of statin use has been shown to inhibit the Hedgehog signaling pathway (Cooper et al, 2003; Corcoran and Scott, 2006), which is critical in the carcinogenesis of basal cell carcinoma (Tang et al, 2007; Von Hoff et al, 2009). Statins have also been shown to inhibit cancer cells in animal models and in vitro (Chan et al, 2003). However, statins also have immunomodulatory properties including increasing regulatory T cells, which may lead to an increased risk for NMSC (Curiel, 2007; Jang, 2008; Mausner-Fainberg et al, 2008; Goldstein et al, 2009a, 2009b). Additionally, statins have been associated with increased photosensitivity, which may be due to their effect on signal-transduction pathways leading to proinflammatory cytokines (Zhang and Elmets, 2010).
Clinical studies have also reported inconsistent relationships between NMSC and statin use. Several large retrospective studies and a meta-analysis of randomised controlled trials (RCTs) found no significant relationship between statins and NMSC incidence (Bjerre and LeLorier, 2001; Asgari et al, 2009; Haukka et al, 2010; Li et al, 2014). An analysis of three statin RCTs designed to examine cardiovascular outcomes also found no increased risk of skin cancer incidence (Peto et al, 2008), whereas other studies (both observation and case–control) have found lower incidence of NMSC and/or overall skin cancer in statin users (Blais et al, 2000; Graaf et al, 2004). On the other hand, several reviews and RCTs have found an increased incidence of NMSC and/or melanoma with statin use (Scandinavian Simvastatin Survival Study Group, 1994; Collins et al, 2002; Kuoppala et al, 2008).
To contribute further to this literature, we investigated the prospective relationship between NMSC and statin use among postmenopausal white women in the Women’s Health Initiative (WHI) Clinical Trial (CT) and WHI Observational Study (OS). Given the high NMSC incidence, especially in older populations, and 2013 cholesterol management guidelines, which are expected to broaden statin use to ∼56 million people in the United States, including patients without known cardiovascular disease (Stone et al, 2014), it is important to further understand this relationship.
Materials and methods
Design, setting, and participants
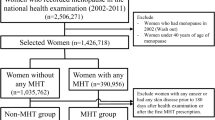
The WHI was designed to study morbidity and mortality in postmenopausal women through a large OS and a set of CTs, including diet modification (DM), hormone therapy (HT), and calcium and vitamin D (CaD), as described previously (WHI Investigators, 1998). In brief, women were recruited between 1993 and 1998 at 40 US clinical centres with the following eligibility criteria: age 50–79 years, postmenopausal, estimated survival of at least 3 years, and no plans to move away from the recruitment area within 3 years. The combined OS+CT multiethnic cohort included 161 808 women. For our analyses, we included only white women owing to the low number of skin cancer cases in other ethnicities, which reduced the analytic cohort size to 133 541. We then excluded participants who lacked follow-up time and medication information at baseline, had personal cancer history at baseline (including NMSC and melanoma), and were missing confounders in the scientific model; this resulted in a final cohort size of 118 357 women (Figure 1).
Measurement of exposures and confounders
For measurement of statin use, participants were instructed to bring prescription medication containers to the baseline screening interview. Medication names were entered into the database by interviewers. Statin use was also updated at years 1, 3, 6, and 9 for CT participants, and year 3 for OS participants using the same methodology. OS women were followed until year 6 and CT women were followed until year 9 because of low number of medication inventories due to study closeout.
Statins were defined as any HMG-CoA reductase inhibitors, and classified based on potency and lipophilicity/hydrophilicity according to a prior WHI study on statin use and melanoma (Jagtap et al, 2012). Lipophilic statins included lovastatin, simvastatin, fluvastatin, and cerivastatin. Hydrophilic statins included atorvastatin, pravastatin, and rosuvastatin. Potency was defined as follows: low – lovastatin, fluvastatin; medium – pravastatin; high – simvastatin, atorvastatin, cerivastatin, rosuvastatin. A small percentage (<1%) of participants used more than one statin drug; among these participants, the analysis duration of statin use was equal to the duration for the drug used for the longest duration time.
Potential confounders were included as covariates in the scientific model and defined a priori based on hypothesised and established factors for NMSC development. Information on confounders was collected through baseline questionnaires, and included the following: age group at screening (50–59, 60–69, and 70–79), education (⩽high school diploma/GED, school after high school, college degree or higher), body mass index (BMI) (<25, ⩾25–30, and >30 kg m−2), smoking status (never, past, and current), vitamin D intake (<200, 200–<400, 400–<600, and ⩾600 IU), solar irradiance of region in Langleys (300–325, 350, 375–380, 400–430, and 475–500), geographic region by latitude (Southern: <35°N; Middle: 35–40°N, and Northern: >40°N), total physical activity (METs per week, quartiles), current health-care provider (yes/no, as proxy for access to medical care), adjustment for assignment to CT (active vs placebo arms of DM, HT conjugated equine Oestrogens and oestrogen+progestin (E+P), and calcium+vitamin D (CaD) trials) or OS, use of oral contraceptives, and use of menopausal HT.
Classification of cases (follow-up and ascertainment)
Non-melanoma skin cancer cases were self-reported through questionnaires (every 6 months for CT and every year for OS) and not centrally adjudicated. Basal cell carcinoma and SCC were not reported separately. Over 10.5 average years of follow-up through August 2009, 11 555 NMSC cases were identified: 1529 among statin users and 10 026 among non-statin users.
Statistical analysis
The primary outcome of interest was development of first-ever NMSC. We used random-effects logistic regression models to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for NMSC incidence in relation to statin use, as time to diagnosis data was not available for self-reported data. A random-effects model allows us to appropriately model the correlation between women’s repeated NMSC reports. We fit two models, age- and study-arm-adjusted and multivariable-adjusted, which adjusted for the confounders listed above. We fit several models estimating ORs for NMSC as a function of these parameters of statin use separately: (1) any statin use, (2) type of statin (as defined earlier in the Materials and Methods section), (3) statin potency, (4) statin category, and (5) duration of statin use in years (none, <1, 1 to <3, ⩾3, <5, and ⩾5). The primary exposure of interest was any statin use, and all others were considered of secondary interest. As such, all secondary P-values were adjusted using the Bonferroni correction to control the family-wise error rate. Each P-value was multiplied by a factor of 4 to account for the four secondary exposures. All tests were two-sided and tested at the 0.05 level of significance.
In the primary model with any statin use as the exposure, we formally tested for effect modification in separate models for each potential effect modifier by using a Wald test to obtain an omnibus P-value for the statistical interaction term. We tested six prespecified variables: age (50–59, 60–69, 70–79 years), BMI (<25, ⩾25–30, and ⩾30 kg m−2), smoking (never, former, and current), solar irradiance Langleys (⩽375 and >375), and vitamin D intake (<400 and ⩾400 IU).
As a post hoc sensitivity analysis, we analysed the relationship between NMSC and statin use at baseline using propensity score matching (PSM). Variables included for matching in the propensity score were defined a priori based on factors that may affect a participant’s propensity for using statins, but were not likely to be affected by statin use itself: health status, age, access to regular medical, current health-care provider, recent pap smear, recent mammogram, income, occupation, education, marital status, physical activity, smoking, vitamin D use, use of oral contraceptives, use of postmenopausal hormonal therapy, solar irradiance in Langleys, latitude, US region, family history (skin cancer, other cancer, MI, diabetes, stroke), osteoporosis history, arthritis history, multivitamin use, history of fracture before the age of 55 years, and CT arms. Propensity was determined by modelling the likelihood of statin use at baseline as a function of the above variables using a logistic regression models. The predicted log ORs resulting from this model were used at propensities. We used these propensities in the Matching package (Sekhon, 2011) in R to implement a 1 to 1 matching scheme where all baseline statin users were matched with a single baseline non-user with the nearest propensity for statin use. The PSM data set was then fit to a conditional logistic regression model grouping on matched pairs. All statistical analyses were completed using SAS 9.3 (SAS Institute, Cary, NC USA) or R 3.1.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
The baseline characteristics of the study cohort are presented in Table 1A, stratified by use of statins at baseline. In general, statin users were older, had higher BMI distributions, and were more likely to have a current health-care provider. Other baseline characteristics were similarly distributed between the two groups. At baseline, 7.5% of the cohort used statins (8.1% in OS and 6.7% in CT); this increased to 13.5% in the OS at year 3 and 18.6% in the CT at year 6 (Table 1B). At baseline, the most commonly used statins in the WHI OS+CT were simvastatin (30.7%), followed by lovastatin (27.5%), pravastatin (22.3%), fluvastatin (12.0%), and atorvastatin (8.2%) (Table 2). Cerivastatin and rosuvastatin were not used at baseline (not on the market at that time) but were reported in follow-up questionnaires in subsequent years. Low potency statins were used by 39.0% of the cohort, compared with 22.2% for medium potency statins, and 38.8% of the cohort for high potency statins. Lipophilic statins were used by 69.8% of the cohort. The distribution of statin use characteristics was similar among OS and CT participants.
In our study cohort, any use of statins (primary hypothesis, as a time-varying variable) in the random-effects logistic regression model was associated with significantly increased NMSC incidence (OR 1.21; 95% CI: 1.07–1.35; Table 3). Secondary analyses were adjusted for multiple testing using the Bonferroni correction method as described in the Materials and Methods section. For the secondary hypothesis of statin type, increased risk was found only for lovastatin (OR 1.52; 95% CI: 1.08–2.16) and simvastatin (OR 1.38; 95% CI: 1.12–1.69). Low (OR 1.33, 95% CI: 1.02–1.74) and high potency statins (OR 1.20; 95% CI: 1.06–1.37) had an increased risk compared with non-statin users. Additionally, lipophilic statin users had a significant increase compared with non-statin users (OR 1.39; 95% CI: 1.18–1.64). There was no clear trend in duration of use; participants using statins for <3 years had a significant increase in odds of NMSC compared with never users; however, those using statins for >3 years were not significantly different compared with never users. In the secondary analyses, there was no statistically significant effect modification found for the relationship between any statin use and NMSC incidence for the prespecified subgroup (age, BMI, smoking, Langleys, vitamin D; Table 4).
As a post hoc sensitivity analysis, we conducted a PSM analysis to reanalyse the relationship between statin use and NMSC incidence, as detailed in the Materials and Methods section. This analysis matched women who used statins with women who did not use statins (but had a similar propensity to use statins), and compared the outcomes between the matched pairs. The PSM analysis was based on ‘any statin use’ and cohort characteristics at study baseline, and did not find a significant relationship between NMSC incidence and statin use.
Discussion
In our large cohort of postmenopausal white women, use of statins was associated with an increased incidence of all NMSC. In particular, after adjusting P-values to account for testing of multiple secondary hypotheses on statin type and potency, increased risk was found for lovastatin and simvastatin statin types only, which was consistent with our finding of an increased risk for lipophilic statins, low potency, and high potency statins. There was no clear association for duration of use. There was also no significant effect modification for the relationship between NMSC and statin use by age, BMI, smoking, Langleys, vitamin D use, or history of NMSC/melanoma. To our knowledge, this is the first study to examine the relationship between statin use and all NMSC in a prospective cohort setting.
Comparison with other studies
The first two simvastatin trials suggested an association with NMSC seen more often in treatment groups (Mascitelli et al, 2010). Other prior clinical studies on the relationship between NMSC and statins have been somewhat limited and conflicting, ranging from no significant relationship (for either all NMSCs or BCC/SCC) (Bjerre and LeLorier, 2001; Asgari et al, 2009; Haukka et al, 2010; Li et al, 2014), increased risk with statin use (Scandinavian Simvastatin Survival Study Group., 1994; Collins et al, 2002; Kuoppala et al, 2008; Arnspang et al, 2014), to decreased risk with statin use (Blais et al, 2000; Graaf et al, 2004; Peto et al, 2008). Few prospective studies have been conducted to investigate the relationship between statin use and either BCC or SCC, particularly with as many participants and cases as our study. However, several large studies have suggested an increased risk of NMSC associated with statin use. One study that showed an increased risk with statin use and NMSC incidence was a meta-analysis of all cancers and statins (median RR 1.6, range 1.2–2, evidence strength moderate) (Kuoppala et al, 2008); this analysis included RCTs, cohort studies, and case–control studies. It was also reported that NMSC was observed more often in the treatment groups of two simvastatin trials, the Scandinavian Simvastatin Survival Study (4S) and the Heart Protection Study (HPS), with the relationship statistically significant if both studies were combined (Scandinavian Simvastatin Survival Study Group, 1994; Collins et al, 2002) This agrees with our finding of a substantial increase in NMSC risk being seen for simvastatin specifically. One record-linkage study of over 400 000 Finnish participants did not find an overall association with statin use and NMSC, but found an increased risk associated with pravastatin specifically (Haukka et al, 2010). A nationwide case–control study in Denmark also found significantly increased risk of BCC only with ever statin use among 38 484 cases (OR 1.09; 1.06–1.33), which the authors attributed to possible residual confounding (Arnspang et al, 2014). A prior WHI analysis found no significant evidence for statin use as a risk factor for melanoma (Jagtap et al, 2012). In addition to these reports, the relationship of NMSC with statin use has been assessed in retrospective and case–control studies with mixed results (Blais et al, 2000; Graaf et al, 2004; Asgari et al, 2009; Haukka et al, 2010; Arnspang et al, 2014).
One plausible biological mechanism for increased NMSC risk with statin use is immunomodulation leading to increased regulatory T cells (Curiel, 2007; Jang, 2008; Mausner-Fainberg et al, 2008; Goldstein et al, 2009a, 2009b). However, multiple molecular pathways have also been proposed for how statins could decrease NMSC risk (Cooper et al, 2003; Gniadecki, 2004; Wu et al, 2004; Corcoran and Scott, 2006; Tang et al, 2007; Von Hoff et al, 2009), and alternative biological mechanisms warrant further study. The literature has also reported photosensitivity and cutaneous side effects associated with statins, which may be related to increased NMSC risk, although the mechanisms are also not well understood (Rodriguez-Pazos et al, 2010; Nardi et al, 2011; Toth et al, 2012).
Sensitivity analysis
In a post hoc PSM analysis conducted as a sensitivity analysis, the use of statins was no longer found to be significantly associated with NMSC incidence. However, the PSM analysis examined outcomes of matched pairs based on a propensity to use statins rather than statin use itself. In contrast, the main analysis, which investigated actual statin use and adjusted for measures of health access, found a significant relationship between NMSC incidence and statin use. Additionally, the PSM analysis was based on characteristics at study baseline; however, statin use increased considerably during the course of the trial, which was accounted for in the main analysis only. The conflicting findings of the main analysis with the PSM analysis suggest other possible contributors to our findings of increased NMSC incidence with statin use, which may be related to characteristics of women with a propensity to use statins (including better medical surveillance and access to care). However, our main analysis and our sensitivity analysis using PSM accounted for measures of socioeconomic status including current health-care provider and education. A randomised trial of statin use would control for such characteristics of users and non-users.
Strengths and limitations
The strengths of this study include the large size and geographic distribution of cohort, prospective nature of the study (given the rarity of prospective studies on this relationship), large size of the cohort and number of NMSC cases, and detailed information on confounders and exposures including statin use (including duration and type). Although factors such as age, BMI, smoking, solar irradiance, and vitamin D intake did not significantly modify the relationship of NMSC with statin use, the fact that our study took these into account is another strength. Limitations of the study include the fact that the study was observational in nature, NMSC was self-reported (not centrally adjudicated) and not further broken down into BCC and SCC, time to event data was not collected, and statin use was self-reported and relatively low at baseline. In addition, we limited the analyses to white women because of the small sample size (and thus potential number of NMSC cases) in other ethnicities, limiting generalisability of the findings to ethnicities where NMSC is not as prevalent. We were also not able to fully adjust for sun exposure because of limitations in the data collection, but we adjusted for proxies of exposure including Langleys and geographic area. Additionally, the lack of duration–effect relationship found for statin use and NMSC incidence (particularly effect found for those treated <1 year) points to the possibility of residual confounding.
Conclusions
In conclusion, the use of statins was associated with increased NMSC risk in our cohort of postmenopausal white women. As statin use is likely to increase significantly in the future under the new statin use guidelines and NMSC is already the most common cancer in the United States, these results may be important and warrant further investigation. As these observations do not provide evidence of causality or that a side effect of statin use is increased NMSC, we are not suggesting changes in current statin recommendations. Regardless, preventive sun exposure measures (which have been shown to be protective against NMSC) should be recommended for statin users as well as non-users (including sunscreen, wearing protective clothing, and avoiding the sun during peak exposure times). Patients at high risk for NMSC because of personal/family history, medical comorbidities, or skin type may want to consider using a statin type that is less strongly associated with NMSC incidence. Further areas for investigation include studying this relationship in the setting of a randomised controlled trial (including the effects of specific statin types on BCC and SCC separately), the effect of protective sun exposure behaviors on this relationship, and the underlying biological mechanisms that may mediate increased NMSC risk from statin use.
Change history
02 February 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arnspang S, Pottegard A, Friis S, Clemmensen O, Andersen KE, Hallas J, Gaist D (2014) Statin use and risk of nonmelanoma skin cancer: a nationwide study in Denmark. Br J Cancer 112 (1): 153–156.
Asgari MA, Tang J, Epstein EH, Chren MM, Warton EM, Quesenberry CP, Go AS, Friedman GD (2009) Statin use and risk of basal cell carcinoma. J Am Acad Dermatol 61 (1): 66–72.
Bjerre LM, LeLorier J (2001) Do statins cause cancer? A meta-analysis of large randomized clinical trials. Am J Med 110 (9): 716–723.
Blais L, Desgagne A, LeLorier J (2000) 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors and the risk of cancer – a nested case–control study. Arch Intern Med 160 (15): 2363–2368.
Chan KKW, Oza AM, Siu LL (2003) The statins as anticancer agents. Clin Cancer Res 9 (1): 10–19.
Christenson LJ, Borrowman TA, Vachon CM, Tollefson MM, Otley CC, Weaver AL, Roenigk RK (2005) Incidence of basal cell and squamous cell carcinomas in a population younger than 40 years. JAMA 294 (6): 681–690.
Collins R, Armitage J, Parish S, Sleight P, Peto R, Collaborati HPS (2002) MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360 (9326): 7–22.
Cooper MK, Wassif CA, Krakowiak PA, Taipale J, Gong R, Kelley RI, Porter FD, Beachy PA (2003) A defective response to Hedgehog signaling in disorders of cholesterol biosynthesis. Nat Genet 33 (4): 508–513.
Corcoran RB, Scott MP (2006) Oxysterols stimulate Sonic hedgehog signal transduction and proliferation of medulloblastoma cells. Proc Natl Acad Sci USA 103 (22): 8408–8413.
Curiel TJ (2007) Tregs and rethinking cancer immunotherapy. J Clin Invest 117 (5): 1167–1174.
Gallagher RP, Hill GB, Bajdik CD, Fincham S, Coldman AJ, McLean DI, Threlfall WJ (1995) Sunlight exposure, pigmentary factors, and risk of nonmelanocytic skin cancer. I. Basal cell carcinoma. Arch Dermatol 131 (2): 157–163.
Gniadecki R (2004) Depletion of membrane cholesterol causes ligand-independent activation of Fas and apoptosis. Biochem Biophys Res Commun 320 (1): 165–169.
Goldstein MR, Mascitelli L, Pezzetta F (2009a) The double-edged sword of statin immunomodulation. Int J Cardiol 135 (1): 128–130.
Goldstein MR, Mascitelli L, Pezzetta F (2009b) Statins, regulatory T cells, and pediatric graft coronary artery disease. Pediatr Transplant 13 (1): 139–140.
Graaf MR, Beiderbeck AB, Egberts ACG, Richel DJ, Guchelaar HJ (2004) The risk of cancer in users of statins. J Clin Oncol 22 (12): 2388–2394.
Gray DT, Suman VJ, Su WP, Clay RP, Harmsen WS, Roenigk RK (1997) Trends in the population-based incidence of squamous cell carcinoma of the skin first diagnosed between 1984 and 1992. Arch Dermatol 133 (6): 735–740.
Haukka J, Sankila R, Klaukka T, Lonnqvist J, Niskanen L, Tanskanen A, Wahlbeck K, Tiihonen J (2010) Incidence of cancer and statin usage—record linkage study. Int J Cancer 126 (1): 279–284.
Hussain SK, Sundquist J, Hemminki K (2009) The effect of having an affected parent or sibling on invasive and in situ skin cancer risk in Sweden. J Invest Dermatol 129 (9): 2142–2147.
Jagtap D, Rosenberg CA, Martin LW, Pettinger M, Khandekar J, Lane D, Ockene I, Simon MS (2012) Prospective analysis of association between use of statins and melanoma risk in the Women's Health Initiative. Cancer 118 (20): 5124–5131.
Jang TJ (2008) Prevalence of Foxp3 positive T regulatory cells is increased during progression of cutaneous squamous tumors. Yonsei Med J 49 (6): 942–948.
Karagas MR, Greenberg ER, Spencer SK, Stukel TA, Mott LA (1999) Increase in incidence rates of basal cell and squamous cell skin cancer in New Hampshire, USA. New Hampshire Skin Cancer Study Group. Int J Cancer 81 (4): 555–559.
Kuoppala J, Lamminpaa A, Pukkala E (2008) Statins and cancer: a systematic review and meta-analysis. Eur J Cancer 44 (15): 2122–2132.
Li X, Wu XB, Chen Q (2014) Statin use is not associated with reduced risk of skin cancer: a meta-analysis. Br J Cancer 110 (3): 802–807.
Lichter MD, Karagas MR, Mott LA, Spencer SK, Stukel TA, Greenberg ER (2000) Therapeutic ionizing radiation and the incidence of basal cell carcinoma and squamous cell carcinoma. The New Hampshire Skin Cancer Study Group. Arch Dermatol 136 (8): 1007–1011.
Mascitelli L, Pezzetta F, Goldstein MR (2010) The epidemic of nonmelanoma skin cancer and the widespread use of statins: Is there a connection? Dermato-Endocrinology 2 (1): 37–38.
Mausner-Fainberg K, Luboshits G, Mor A, Maysel-Auslender S, Rubinstein A, Keren G, George J (2008) The effect of HMG-CoA reductase inhibitors on naturally occurring CD4+CD25+ T cells. Atherosclerosis 197 (2): 829–839.
National Cancer Institute (2012) Cancer Trends Progress Report – 2011/2012 Update. National Cancer Institute, Bethesda, MD, USA.
Nardi G, Lhiaubet-Vallet V, Leandro-Garcia P, Miranda MA (2011) Potential phototoxicity of rosuvastatin mediated by its dihydrophenanthrene-like photoproduct. Chem Res Toxicol 24 (10): 1779–1785.
Peto R, Emberson J, Landray M, Baigent C, Collins R, Clare R, Califf R (2008) Analyses of cancer data from three ezetimibe trials. N Engl J Med 359 (13): 1357–1366.
Rodriguez-Pazos L, Sanchez-Aguilar D, Rodriguez-Granados MT, Pereiro-Ferreiros MM, Toribio J (2010) Erythema multiforme photoinduced by statins. Photodermatol Photoimmunol Photomed 26 (4): 216–218.
Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, Coldiron BM (2010) Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol 146 (3): 283–287.
Scandinavian Simvastatin Survival Study Group (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344 (8934): 1383–1389.
Sekhon JS (2011) ‘Multivariate and Propensity Score Matching Software with automated balance optimization: the matching package for R.’. J Stat Softw 42 (7): 1–52.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr., Watson K, Wilson PW, Eddleman KM, Jarrett NM, LaBresh K, Nevo L, Wnek J, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Curtis LH, DeMets D, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK, Smith SC Jr., Tomaselli GF American College of Cardiology/American Heart Association Task Force on Practice G (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129 (25, Suppl 2): S1–45.
Tang JY, So PL, Epstein EH Jr (2007) Novel Hedgehog pathway targets against basal cell carcinoma. Toxicol Appl Pharmacol 224 (3): 257–264.
Toth PP, Morrone D, Weintraub WS, Hanson ME, Lowe RS, Lin J, Shah AK, Tershakovec AM (2012) Safety profile of statins alone or combined with ezetimibe: a pooled analysis of 27 studies including over 22,000 patients treated for 6-24 weeks. Int J Clin Pract 66 (8): 800–812.
van Dam RM, Huang Z, Rimm EB, Weinstock MA, Spiegelman D, Colditz GA, Willett WC, Giovannucci E (1999) Risk factors for basal cell carcinoma of the skin in men: results from the health professionals follow-up study. Am J Epidemiol 150 (5): 459–468.
Von Hoff DD, LoRusso PM, Rudin CM, Reddy JC, Yauch RL, Tibes R, Weiss GJ, Borad MJ, Hann CL, Brahmer JR, Mackey HM, Lum BL, Darbonne WC, Marsters JC Jr, de Sauvage FJ, Low JA (2009) Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med 361 (12): 1164–1172.
WHI Investigators (1998) Design of the Women's Health Initiative clinical trial and observational study. The Women's Health Initiative Study Group. Control Clin Trials 19 (1): 61–109.
Wu J, Wong WW, Khosravi F, Minden MD, Penn LZ (2004) Blocking the Raf/MEK/ERK pathway sensitizes acute myelogenous leukemia cells to lovastatin-induced apoptosis. Cancer Res 64 (18): 6461–6468.
Zhang A, Elmets CA (2010) Drug-induced photosensitivity. eMedicine. Available at: http://emedicine.medscape.com/article/1049648-overview-a5 (accessed 15 September 2015).
Acknowledgements
We acknowledge the dedicated efforts of investigators and staff at the WHI clinical centres, the WHI Clinical Coordinating Center, and the National Heart, Lung, and Blood program office (listing available at http://www.whi.org). We also recognise the WHI participants for their extraordinary commitment to the WHI program. The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, US Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C. The funders had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The WHI is registered under ClinicalTrials.gov. Trial registration ID: NCT00000611. This study was approved by the ethics committees at the WHI Coordinating Center, Fred Hutchinson Cancer Research Center, and all 40 clinical centres.
Author contributions
AW, MS, MD, and JT participated in study conception and design. KK, HH, and MD performed the data analysis. AW, MS, MD, and JT participated in initial data interpretation. AW wrote the initial draft of the manuscript. All authors contributed to additional data interpretation and revisions and approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
These data were presented in part as a Late-Breaking Abstract at the 2014 Society of Investigative Dermatology meeting (LB806).
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Wang, A., Stefanick, M., Kapphahn, K. et al. Relation of statin use with non-melanoma skin cancer: prospective results from the Women’s Health Initiative. Br J Cancer 114, 314–320 (2016). https://doi.org/10.1038/bjc.2015.376
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.376
Keywords
This article is cited by
-
Investigating the burden of cardiovascular comorbidities in inpatient non-melanoma skin cancer outcomes
Archives of Dermatological Research (2023)
-
Comment on ‘Statin use and all-cancer survival: prospective results from the Women’s Health Initiative’
British Journal of Cancer (2017)
-
Protective Effects of Statins in Cancer: Should They Be Prescribed for High-Risk Patients?
Current Atherosclerosis Reports (2016)