Abstract
Background:
Retinoblastoma is a rare childhood eye cancer caused by germline or somatic mutations in the RB1 gene. Previous studies observed elevated breast cancer risk among retinoblastoma survivors. However, there has been no research on breast cancer risk in relation to radiation (primarily scatter radiation from the primary treatment) and genetic susceptibility of retinoblastoma survivors.
Methods:
Two groups of retinoblastoma survivors from the US and UK were selected, and breast cancer risk analysed using a case–control methodology, nesting within the respective cohorts, matching on heritability (that is to say, having bilateral retinoblastoma or being unilateral cases with at least one relative with retinoblastoma), and using exact statistical methods. There were a total of 31 cases and 77 controls.
Results:
Overall there was no significant variation of breast cancer risk with dose (P>0.5). However, there was a pronounced and significant (P=0.047) increase in the risk of breast cancer with increasing radiation dose for non-heritable retinoblastoma patients and a slight and borderline significant (P=0.072) decrease in risk of breast cancer with increasing radiation dose for heritable retinoblastoma patients, implying significant (P=0.024) heterogeneity in radiation risk between the heritable and non-heritable retinoblastoma groups; this was unaffected by the blindness status. There was no significant effect of any type of alkylating-agent chemotherapy on breast cancer risk (P>0.5).
Conclusions:
There is significant radiation-related risk of breast cancer for non-heritable retinoblastoma survivors but no excess risk for heritable retinoblastoma survivors, and no significant risk overall. However, these results are based on very small numbers of cases; therefore, they must be interpreted with caution.
Similar content being viewed by others
Main
Retinoblastoma (RB) is a rare childhood eye cancer caused by germline or somatic mutations in the RB1 tumour suppressor gene. A total of 25–35% of children with RB develop tumours in both eyes (bilateral) as a result of a germline mutation in the RB1 gene, and the other 65–75% of children with RB develop tumours in only one eye (unilateral) usually caused by somatic mutations in the RB1 gene (Knudson, 1971). Although all bilateral survivors are presumed to have a germline mutation, only approximately one-third have inherited a mutation from a parent, whereas the other two-thirds have a de novo germline mutation that occurs during formation of the sperm or egg from an unaffected parent (Dryja et al, 1989; Little et al, 2012). Unilateral cases with a family history of RB (at least one relative with RB) are also considered to be heritable cases, whereas the remaining majority of unilateral cases are considered to be non-heritable. Despite excellent long-term survival, previous studies have found that long-term heritable RB survivors have an elevated risk of developing second cancers (SCs) associated with RB radiation treatment (Marees et al, 2008; Kleinerman et al, 2012). Although non-heritable RB patients were not at greater risk of a SC overall compared with the general population, and much less likely to receive radiotherapy (RT) than heritable RB patients, breast cancer risk was significantly elevated in both heritable and non-heritable RB patients (Kleinerman et al, 2005; Reulen et al, 2008).
The male and female breast is known to be radiosensitive, especially following exposures at young ages (Preston et al, 2002; Ron et al, 2005). A recent study has highlighted very high radiation breast cancer risks associated with diagnostic exposures among a genetically susceptible subgroup of BRCA1/2 survivors (Pijpe et al, 2012), although two other US studies of BRCA1/2 mutation carriers did not find increased risks associated with therapeutic radiation exposure (Bernstein et al, 2013) or diagnostic radiation for those exposed under the age of 50 (John et al, 2013). In addition, there are structural abnormalities and loss of expression of the RB1 gene in 20–35% of all breast tumours (Varley et al, 1989; Bosco and Knudsen, 2007). However, as yet, there has been little epidemiologic research on the risk of breast cancer in relation to radiation and genetic susceptibility of long-term RB survivors.
We therefore performed radiation dose–response analyses in a case–control study of breast cancer following RB nested within a previously evaluated US cohort of long-term survivors of RB (Kleinerman et al, 2005, 2012) to determine this risk. We pooled data from this case–control study with another case–control data-set nested within a UK cohort of breast cancers after childhood cancer (Reulen et al, 2008). Owing to the known effects of certain forms of chemotherapy, in particular alkylating agents, on risk of subsequent breast cancer (Travis et al, 2003), we assessed risks in relation both to chemotherapy and to radiation exposure. Owing to the reported association between blindness and breast cancer incidence (Feychting et al, 1998; Pukkala et al, 1999; Verkasalo et al, 1999; Flynn-Evans et al, 2009) we also examined the effect of adjusting for this.
Materials and methods
The US cohort consisted of 1601 1-year survivors of RB diagnosed between 1914 and 1984 at two US hospitals, as previously studied by Kleinerman et al (2005). Seven hundred and fifty-five of these (47.2%) were female. There were 17 people with missing RT treatment information who were excluded, leaving an analysis cohort of 1584. Abstractors recorded baseline information from hospital records on diagnosis, laterality, treatment, and family history of RB as well as any mention of a SC. Any SC diagnosed up to 31 December 2001 was obtained by trained interviewers through three separate telephone interviews with survivors or parents, as described elsewhere (Kleinerman et al, 2005). In addition, periodic searches of the National Death Index were conducted to ascertain information on vital status and causes of deaths (Yu et al, 2009). Invasive SCs were confirmed by autopsy and pathology reports whenever possible (14 cases), hospital or physician records (four cases), death certificates (six cases), or initial questionnaire (one case). We excluded all in situ cancers from this analysis. A nosologist coded all confirmed breast cancers according to the International Classification of Diseases for Oncology (Fritz et al, 2000). Person–years of follow-up began 1 year after RB diagnosis and continued until the earliest occurring of: (a) the patient developing invasive breast cancer; (b) last contact; (c) death; or (d) 31 December 2008. The Special Studies Institutional Review Board of the National Cancer Institute approved the study.
The UK cohort consisted of 581 female patients diagnosed with RB between 1940 and 1991 under the age of 15 and who had survived at least 5 years after RB, as previously studied (Hawkins et al, 2008; Reulen et al, 2008). The cohort was ascertained through the National Registry of Childhood Tumours (NRCT), which is a population-based registry maintained by the Childhood Cancer Research Group at the University of Oxford. The methods of ascertainment were as described previously (Hawkins et al, 1992). The population-based cohort was electronically linked, using full personal identifiers, to the population-based national cancer registries for England, Wales and Scotland through ‘flagging’ at the National Health Service Central Registers, which provided incident SC from 1971 (Hawkins et al, 1992). We also wrote to the general practitioner of every survivor who had not died to specifically ask about the occurrence of any SC. In addition, a questionnaire was sent to survivors who were aged at least 16 years which included questions specifically relating to SC (Hawkins et al, 2008). The NRCT provided ascertainment of all cancers diagnosed below age 15 years. Finally, through ‘flagging’ we obtained underlying causes of death relating to all deaths occurring beyond 5 years from diagnosis of childhood cancer, and deaths coded to neoplastic causes were carefully investigated. Time at risk for a subsequent primary breast cancer began at 5 years subsequent to RB diagnosis and ended at the earliest of: (a) the patient developing invasive breast cancer; (b) the first occurrence of loss to follow-up; (c) death; or (d) reaching the study exit date, December 31, 2005. Because national breast cancer incidence rates only became available with the start of the UK National Health Service Central Register Cancer Registry in 1971, breast cancer rates were estimated for the period 1962–1970 by use of the mean rates for the period 1971–1974.
Case–control studies
Twenty female and one male breast cancer cases were identified from the US cohort using medical records, telephone interviews, or self-reports, and as described above were confirmed with pathology reports or death certificates. (The two multiple primary cases in the cohort were each counted as a single case, and another case had an intervening cancer.) Each case had to be the first primary cancer (apart from non-melanoma skin cancer) after the RB. Each case was matched to a maximum of three controls on sex, RB heritable status, and date of birth within 5 years, to control for heritability, sex, and birth cohort variations. Each control had to be alive and free of any subsequent cancer (apart from non-melanoma skin) for a period at least as long as the corresponding interval from RB diagnosis to breast cancer diagnosis in the index case. If more than three controls were available meeting these criteria, three controls were selected at random. Fifty-six controls were selected. For the UK (GENE-RAD-RISK) data set there were 10 female breast cancer cases, and for each up to five controls were selected using the above matching criteria and for the same reasons. If more than five controls were available meeting these criteria, five controls were selected at random. A total of 21 controls were selected. For a single case the matching criteria on the year of birth had to be relaxed to be within 10 years. In addition, a suitable control could not be found for a single case each in the UK and US cohorts; both cases were excluded, although they were included in the SIR analysis of Table 2. A single (heritable) case in the US cohort developed an intervening cancer, and therefore was not included in the case–control study, although it was included in the SIR analysis of Table 2. Information on bilateral blindness was only available for the US cohort.
Radiation dosimetry
Detailed information on radiation treatment of RB was abstracted from RT records for US and UK cases and controls, and absorbed dose to the breast bud, which was primarily scatter radiation from the primary treatment field (the eye), was estimated by measurements and computer simulations, based on clinical treatment notes (Ligot et al, 1998; Shamsaldin et al, 2000; Stovall et al, 2006). Scatter dose is likely to be less of an issue currently than formerly because, as noted by Kleinerman et al (2005), the rates of SCs were higher among those treated with the lower energy (kilovoltage) radiation, which had much more scatter, in the earlier part of the cohort, than with the much higher energy (megavoltage) therapy used later. The first US case or control with radiation treatment was in 1928 and the first UK case or control in 1948; reconstruction of doses from such relatively old records is not in principle difficult, nor any less reliable than for more modern treatment data, if the records can be found. Actual conditions of exposure were simulated based on external beam machine characteristics, field configurations, treatment conditions, and patient characteristics (for example, age; Ligot et al, 1998; Shamsaldin et al, 2000; Stovall et al, 2006). The breast radiation dose was estimated for each individual patient from the dose received to the eye for RB treatment, in particular accounting for age at treatment and other parameters (Ligot et al, 1998; Shamsaldin et al, 2000; Stovall et al, 2006). Breast dose for the UK cases and controls was estimated using the ICTA software package developed at the Gustave Roussy Institute, again based on clinical treatment notes (Ligot et al, 1998; Shamsaldin et al, 2000). Doses for the cases were for the breast bud of the affected breast; doses for the matched controls were for the same (left/right) breast bud as for the index case. All information on the data, reliability, and validity of the method used in this software to estimate absorbed doses of RT can be found in previous publications (Ligot et al, 1998; Shamsaldin et al, 2000).
Statistical methods
For the US cohort, the expected number of breast cancers in the general population was estimated from age-, sex-, and calendar-year-specific cancer incidence rates from Connecticut for 1935–1972 (and for years from 1973 onwards via SEER) Tumor Registries. For expected cancer rates before 1935, when the Connecticut Tumor Registry began, we used rates for 1935–1939. For the UK data, analogous computations were performed using the corresponding neoplasm rates of the England and Wales general population. The standardised incidence ratio (SIR) was estimated with exact (Poisson-based) 95% confidence intervals (Breslow and Day, 1987). As described below, log-linear conditional logistic regression models were used to examine the dose–response relationship between the odds ratio (OR) for breast cancer and radiation dose in the case–control data, in which the assumed probability of breast cancer (Y=1) following a breast dose of D Gy, chemotherapy type C (=none, triethylenemelamine, cyclophosphamide), and bilateral blindness indicator B is assumed to be given by:

Information on chemotherapy was derived from clinical treatment notes in each component data set; for the US cohort, information on bilateral blindness was derived in the same way.
The model was fitted via conditional maximum likelihood using LogXact 10 (Cytel, Inc., Cambridge, MA, USA, 2013) and excluded patients with unknown radiation dose. Mid-p exact confidence intervals were derived, and all hypothesis tests (for example, of heterogeneity of OR by heritability subgroup and age) were based on fitting appropriate generalisations of the above logistic model, with interaction terms to test for the desired effect (for example, departure from homogeneity) (Cox and Hinkley, 1974), and reported in Table 5. Additional analyses of unconditional OR are reported (in Table 4), with P-values computed via Fisher’s exact test and associated exact confidence intervals on the OR estimated using the epitools library of R (R version 3.0.1, http://www.r-project.org/, 2013). Sensitivity analyses were also conducted (the results of which are not reported in the Tables) in which we excluded the single male case and associated controls, also examining the effects of adjusting for chemotherapy in the RB heritable and non-heritable groups separately.
Ethical approvals
The Special Studies Institutional Review Board of the National Cancer Institute approved the US study protocol. The UK study obtained consent of the multicentre research ethics committee and every local research ethics committee in Britain.
Results
As indicated in Table 1, overall there were 1584 survivors of both sexes in the US cohort, with 25 breast cancer cases and 45 590 person–years of follow-up among 1-year survivors. In the UK cohort, there were 581 female survivors with 11 breast cancer cases and 15 838 person–years of follow-up among 5-year survivors (Table 1). The mean age at RB diagnosis was 1.3 years in the US cohort and 1.8 years in the UK cohort (Table 1).
Table 2 demonstrates that among irradiated patients in the two RB cohorts, the SIR for the irradiated patients is 3.89 (95% CI 2.34, 6.07) while for the non-irradiated patients the SIR is 3.04 (95% CI 1.77, 4.87); there are similar patterns of risk in the two component (US, UK) cohorts (Table 2). The SIR for breast cancer is 3.43 (95% CI 1.88, 5.76) for irradiated heritable RB patients and 6.19 (95% CI 2.01, 14.45) for the irradiated non-heritable group. There were indications of excess risk of breast cancer also among the unirradiated heritable and non-heritable RB patients, which for both groups were statistically significant, with SIRs of 8.72 (95% CI 3.51, 17.97) and 2.09 (95% CI 1.00, 3.84), respectively. The ratio of SIRs for irradiated : unirradiated suggests an excess radiation-associated risk both overall (heritable+non-heritable; relative risk (RR)=3.89/3.04=1.28) and for the non-heritable RB group (RR=6.19/2.09=2.97) but not for the heritable RB group (RR=3.43/8.72=0.39). The same pattern was also observed in the US cohort (RR=1.19 overall, RR=3.16 for non-heritable RB, RR=0.35 for heritable RB) and in the UK cohort (RR=1.50 overall, RR=2.29 for non-heritable RB, RR=0.49 for heritable RB).
Table 3 lists descriptive characteristics of the 31 cases and 77 controls in the combined US and UK case–control studies. Seventeen breast cancer cases (54.8%) and 42 controls (54.5%) had heritable RB. Age at RB diagnosis was comparable for cases and controls (mean, 18.6 months; mean, 17.2 months). The mean age at breast cancer diagnosis was 43.6 years (range, 25–61.9). The mean total breast bud radiation dose was 0.16 Gy (range, 0–0.65 Gy) for cases and was 0.17 Gy (range, 0–1.3 Gy) for controls (Table 3).
The unconditional exact analysis of Table 4 shows that there were no radiation-exposed controls in the non-heritable RB group, so that ORs for all non-zero dose groups were infinite. The indications of excess risk (or lack of it) by RB-heritability status were similar for both the US and UK groups, and generally similarly statistically significant (or not) for the US data set as in total (for example, the OR for non-heritable cases 0.01+ Gy vs 0 Gy was ∞ (95% CI 1.86, ∞), P=0.014, data not shown); none of the findings for the UK data set were statistically significant.
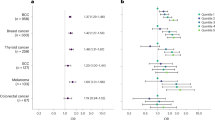
The conditional exact regression analysis of Table 5 demonstrates that overall there was no significant variation in breast cancer risk with dose (P>0.5). However, there was a pronounced and statistically significant (P=0.047) increase in the excess OR per Gy for non-heritable RB patients, and a modest and borderline significant (P=0.072) decrease for heritable RB patients. Consequently, there was significant (P=0.024) heterogeneity in radiation risk between the heritable and non-heritable RB groups, and this was true, at borderline levels of significance, for the US series (P=0.064, results not shown). These results were essentially unchanged if additional adjustment was made for bilateral blindness (Table 5). (The contrast of the conditional exact regression analysis of this Table with the unconditional exact analysis of Table 4 should be noted; the latter also does not take individual dose estimates into account but is simply assessing the OR for exposed vs unexposed.)
Results were essentially unchanged if only female subjects were considered. The exact regressions of Table 5 were the same, and as the male case was non-heritable and radiation unexposed, the effect of excluding him was to make the SIR in Table 2 for the relevant cell marginally statistically significant (nine cases observed, 4.78 expected, SIR=1.88, 95% CI 0.86, 3.57; results not shown).
Table 6 demonstrates that there were elevated but nonsignificant effects of alkylating agent chemotherapy on breast cancer risk (OR=1.76, 95% CI=0.40, 9.25, two-sided P=0.578), either overall or within the RB heritable or non-heritable subgroups (P>0.5, results not shown). However, although these data were available in both cohorts, they were less complete in the US study.
Discussion
The analyses of this paper suggest that, although there is no overall significant trend in breast cancer risk with radiation dose, among non-heritable RB cases there is a high and statistically significant radiogenic risk of breast cancer, in contrast to the lack of evidence for radiogenic risk among heritable RB cases. To the best of our knowledge, this is the first study of breast cancer in relation to radiation dose and genetic susceptibility of long-term RB survivors.
Table 7 shows that the overall risks in this study are somewhat lower, indeed nonsignificantly negative, compared with those estimated in other groups, in particular the US scoliosis cohort (Doody et al, 2000), for whom the ERR/Gy was 5.4 (95% CI 1.2, 14.1). Risks in most other radiation-exposed groups are lower than this (Table 7) and are probably not inconsistent with those in the present study; however, the wide range of ages at exposure should be noted. (It should be noted that strictly the presentation of an overall OR estimate for our study in Table 7 may be invalid, given the presence of heterogeneity in risk by RB heritable status. Nevertheless, for the purposes of comparison with the other studies, which lack information on heritability, we judge that presenting the overall estimate in Table 7 is the correct thing to do here.)
Reulen et al (2008) examined breast cancer incidence in relation to population expected numbers and radiation and RB heritability status, and observed a significant excess risk among the heritable RB survivors, both among those receiving radiation therapy and those not so doing, somewhat similar to our findings (Table 2). There was also an elevated risk (albeit nonsignificant) among the non-heritable RB survivors (Reulen et al, 2008), again paralleling our findings (Table 2).
There are experimental data suggesting that inactivation of RB can interfere with induction of senescence in two human breast cancer cell lines (Bazarov et al, 2012). Retinoblastoma inactivation has also been implicated in triple-negative breast cancers (lacking receptors for oestrogen receptor (ER), progesterone receptor (PR), or human epidermal growth factor receptor 2 (HER2); Trere et al, 2009) that account for 10–17% of all breast carcinomas (Reis-Filho and Tutt, 2008). We were unable to investigate how breast cancer risk varied by receptor status in this study due to the lack of available data.
There are known to be other associations of breast cancer with the RB1 gene: structural RB1 abnormalities were detected in DNA from 15 out of 77 (19%) of sporadic, primary breast carcinomas examined clinically (Varley et al, 1989). However, a much lower prevalence (3 out of 73) was observed in another clinical series (Berge et al, 2010). It is reasonably clear that RB1 mutation is associated with breast cancer, albeit in a relatively small proportion (<5%) of cases in the general population (Cancer Genome Atlas Network, 2012), although its involvement in the various other epithelial tumours in which mutations in RB1 have been detected (Harbour et al, 1988; Kubota et al, 1995; Miyamoto et al, 1995) is less clear. RB1 is known to be involved in cell cycle regulation (Weinberg, 1995).
It is well known that RB survivors experience an elevated incidence of many cancer types in adulthood (Fletcher et al, 2004; Marees et al, 2008; Kleinerman et al, 2012). The excess risk is not exclusively associated with possible radio- or chemotherapy received – among those with heritable RB – because there is still a significant excess of these tumours among those with heritable RB who were treated surgically only (Fletcher et al, 2004; Marees et al, 2008). This may go some way to explain our findings. The particularly elevated risk (SIR=8.72, Table 2) of breast cancer seen in heritable RB patients who were not treated with radiation indicates the importance of RB heritability for breast cancer. However, the somewhat less elevated risk (SIR=2.09, Table 2) of breast cancer seen in the unirradiated non-heritable RB patients suggests that there must also be non-genetic factors raising risk. There is more general evidence to suggest that individuals with higher baseline risk of developing cancer (in the absence of radiation exposure) may have a reduced radiation-associated RR (Little et al, 1999); in particular, the study of Little et al (1998) showed that brain tumour excess RRs per Gy (ERR) were markedly lower among the patients with cancer-prone disorders compared with those in the non-susceptible population at borderline levels of statistical significance (two-sided P=0.06). Likewise, in the study by Tucker et al (1987) there were nonsignificant indications (two-sided P=0.67) of a lower bone tumour radiogenic ERR among patients with RB than among those patients without RB. In the study by Tucker et al (1987) the RB group includes both those patients treated for bilateral RB, which are presumed to be heritable, and those treated for unilateral RB, most of which are presumed to be non-heritable. The vast majority (21 out of 22 (95.5%) of the cases, 57 out of 65 (87.7%) of the controls) of the patients with RB in the study by Tucker et al (1987) had bilateral RB. Combining our results with those of other heritable radiation-exposed groups (Tucker et al, 1987; Little et al, 1998; Bernstein et al, 2013; John et al, 2013), but in contrast to the results of another recent study (Pijpe et al, 2012), it would appear that in the high-risk heritable group (in our case the RB1 gene mutation carriers) the much higher baseline breast cancer risk induced by the genetic component may leave minimal opportunity for expression of a radiation effect. The very high risk in the non-heritable RB group is probably to some extent due to chance, a consequence in part of the small numbers in this data set. Nevertheless, our finding is supported by much other data (Tucker et al, 1987; Little et al, 1998; Bernstein et al, 2013; John et al, 2013), albeit in relation to other end points and familial genetic syndromes, suggesting that it is in the non-heritable RB group where one would expect to see the largest excess radiation risk. While this would explain why risks were lower in the heritable group, it would not explain why the SIR in the radiation-treated heritable RB group should be lower than that for the unirradiated heritable group (RR=3.43/8.72=0.39, Table 2), resulting in a RR that is less than 1. The fact that this is observed in both data sets suggests that it may not be a chance finding (although chance cannot be entirely discounted), the explanation for which is not clear to us. One possible explanation is that there is something about the subjects in the heritable RB group who were not given RT that places them at higher risk than the subjects in the heritable RB group given RT, possibly a result of other therapy that they received, or possibly selection. As shown by Table 6, some types of alkylating-agent chemotherapies double the breast cancer risk; therefore, this may contribute to a part of the effect observed here. One might also hypothesise that cells with one RB1 mutation might be more sensitive to the effects of radiation so that more of the nascent breast bud cells could be killed, rather than damaged.
The present study has limitations. In particular, the small number of cases means that chance cannot completely be discounted as a source of the findings. Assessment of heterogeneity in such a small data set is potentially difficult and may be stretching the analysis further than is warranted. The small size of the study and the relatively modest radiation doses mean that the study should have low power to detect moderate risks (Little et al, 2010), although not risks of the magnitude observed in the non-heritable RB group; it is well known that any significant findings in underpowered studies are likely to be overestimates of the true effects (Land, 1980). Although parity and family history are important risk factors for breast cancer (Costantino et al, 1999), there is no information on these covariates in the US cohort. There are such data in the UK series; however, the small size of the data set and the substantial fraction of missing information made further analysis impossible. Likewise, blindness is thought to be protective with respect to breast cancer risk (Feychting et al, 1998; Pukkala et al, 1999; Verkasalo et al, 1999; Flynn-Evans et al, 2009). Information is only available in the US cohort on this; however, there is little evidence of a confounding effect of blindness on our results (Table 5). There are other differences in the underlying populations in the two countries (US, UK) – for example, in the weight by age. However, this is unlikely to affect results as controls were sampled for each case within the associated national cohort data set.
As discussed above, while we would expect a lower risk in the heritable RB group than in the non-heritable RB group, the finding of a borderline significant negative trend for the former (and the very high risk for the latter) is implausible. The most likely explanation is chance, resulting from the very small numbers in the study – it should be emphasised that the negative trend for the heritable RB group and the positive trend for the non-heritable RB group are both of borderline statistical significance (P=0.072, P=0.047, respectively, Table 5). Another possibility is that by chance the controls were not correctly chosen. However, as we note below, the pattern of risk was the same in both component substudies (US, UK), and it appears moderately implausible (but not impossible) that the same pattern of bias should operate in the two cohorts. The OR estimates for the non-heritable RB group were infinite; for this reason, all inferences in this paper were based on exact statistics (using LogXact, Cytel, Inc.). However, because of the small numbers, non-statistical sources of error are possibly of more significance. It is possible that somehow the cases we reported as non-heritable RB were really heritable RB. De novo germline mutations that manifest as unilateral RB will only become unmasked with affected offspring, which may or may not have occurred. There are other possibilities also – for example, incomplete family histories, or unexpressed or less penetrant mutations in the parents. Another possibility (again perhaps rather unlikely) is that somehow treatment dose was missed. It is reassuring that both the UK and US data sets are consistently pointing in the same direction, in relation to risks in heritable and non-heritable RB groups, although unsurprisingly (given the small numbers in each), there are at best borderline indications of significance (for example, P=0.064 for heterogeneity of radiation risk between the heritable and non-heritable US cases) in either of the component data sets considered separately. Another reassuring feature is the measure of consistency between the results of the cohort and case–control studies, so that from Table 2 one can estimate a RR (RT exposed vs RT unexposed) in the heritable RB group of 3.43/8.72=0.39, while for the non-heritable RB group the analogous RR is 6.19/2.09=2.96. These are within the 95% CI given in the last line of Table 4, namely (0.22, ∞) and (2.62, ∞), respectively.
Nevertheless, the results are intriguing because both the US and UK case–control series indicate that the risk for radiation-related breast cancer is greater in the non-heritable than in the heritable RB survivors, and the risk in the latter group is not raised. In the past, radiation was much more likely to be used to treat the heritable RB patients (about 85% of the US patients received RT), whereas non-heritable RB patients typically were treated surgically (only about 15% of the US patients were treated with RT and mostly had more extensive or recurrent disease). Radiation would be used for extensive disease not treatable with globe excision or recurrent disease after surgery. Both would possibly occur in slightly older individuals. Only one orbit would likely have been treated in contrast to bilateral RB where both orbits could be treated. In particular, the vast majority (>99%) of unilateral cases without microscopic or macroscopic extraocular disease would normally be treated by enucleation (Abramson and Schefler, 2004). This could account for the lack of controls who received RT in the non-heritable RB group. As discussed above, the lower radiation-related risk in the heritable group may be attributed to the higher baseline risk for breast cancer due to a germline RB1 mutation. Retinoblastoma patients are less frequently treated with RT today (Gobin et al, 2011). The present study highlights the elevated breast cancer risk in RB survivors, irrespective of radiation treatment or heritability group (Table 2), and indicates the need for further follow-up of these cohorts.
Change history
13 May 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abramson DH, Schefler AC (2004) Update on retinoblastoma. Retina 24 (6): 828–848.
Adams MJ, Dozier A, Shore RE, Lipshultz SE, Schwartz RG, Constine LS, Pearson TA, Stovall M, Winters P, Fisher SG (2010) Breast cancer risk 55+ years after irradiation for an enlarged thymus and its implications for early childhood medical irradiation today. Cancer Epidemiol Biomarkers Prev 19 (1): 48–58.
Bazarov AV, Lee WJ, Bazarov I, Bosire M, Hines WC, Stankovich B, Chicas A, Lowe SW, Yaswen P (2012) The specific role of pRb in p16INK4A_ mediated arrest of normal and malignant human breast cells. Cell Cycle 11 (5): 1008–1013.
Berge EO, Knappskog S, Geisler S, Staalesen V, Pacal M, Børreson-Dale A-L, Puntervoll P, Lillehaug JR, Lønning PE (2010) Identification and characterization of retinoblastoma gene mutations disturbing apoptosis in human breast cancers. Mol Cancer 9: 173.
Bernstein JL, Thomas DC, Shore RE, Robson M, Boice JD Jr, Stovall M, Andersson M, Bernstein L, Malone KE, Reiner AS, Lynch CF, Capanu M, Smith SA, Tellhed L, Teraoka SN, Begg CB, Olsen JH, Mellemkjaer L, Liang X, Diep AT, Borg A, Concannon P, Haile RW (2013) Contralateral breast cancer after radiotherapy among BRCA1 and BRCA2 mutation carriers: A WECARE Study Report. Eur J Cancer 49 (14): 2979–2985.
Bosco EE, Knudsen ES (2007) RB in breast cancer: at the crossroads of tumorigenesis and treatment. Cell Cycle 6 (6): 667–671.
Breslow NE, Day NE (1987) Statistical methods in cancer research. Volume II—The design and analysis of cohort studies. IARC Sci Publ 82: 1–406.
Cancer Genome Atlas Network (2012) Comprehensive molecular portraits of human breast tumours. Nature 490 (7418): 61–70.
Costantino JP, Gail MH, Pee D, Anderson S, Redmond CK, Benichou J, Wieand HS (1999) Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst 91 (18): 1541–1548.
Cox DR, Hinkley DV (1974) Theoretical Statistics pp 1–511. Chapman and Hall: London.
Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE (2000) Breast cancer mortality after diagnostic radiography: findings from the U.S. Scoliosis Cohort Study. Spine (Phila Pa 1976) 25 (16): 2052–2063.
Dryja TP, Mukai S, Petersen R, Rapaport JM, Walton D, Yandell DW (1989) Parental origin of mutations of the retinoblastoma gene. Nature 339 (6225): 556–558.
Feychting M, Österlund B, Ahlbom A (1998) Reduced cancer incidence among the blind. Epidemiology 9 (5): 490–494.
Fletcher O, Easton D, Anderson K, Gilham C, Jay M, Peto J (2004) Lifetime risks of common cancers among retinoblastoma survivors. J Natl Cancer Inst 96 (5): 357–363.
Flynn-Evans EE, Stevens RG, Tabandeh H, Schernhammer ES, Lockley SW (2009) Total visual blindness is protective against breast cancer. Cancer Causes Control 20 (9): 1753–1756.
Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S (2000) International Classification of Diseases for Oncology 3rd edn. World Health Organization: Geneva, Switzerland.
Gobin YP, Dunkel IJ, Marr BP, Brodie SE, Abramson DH (2011) Intra-arterial chemotherapy for the management of retinoblastoma: four-year experience. Arch Ophthalmol 129 (6): 732–737.
Guibout C, Adjadj E, Rubino C, Shamsaldin A, Grimaud E, Hawkins M, Mathieu M-C, Oberlin O, Zucker J-M, Panis X, Lagrange J-L, Daly-Schveitzer N, Chavaudra J, de Vathaire F (2005) Malignant breast tumors after radiotherapy for a first cancer during childhood. J Clin Oncol 23 (1): 197–204.
Harbour JW, Lai S-L, Whang-Peng J, Gazdar AF, Minna JD, Kaye FJ (1988) Abnormalities in structure and expression of the human retinoblastoma gene in SCLC. Science 241 (4863): 353–357.
Hawkins MM, Kinnier Wilson LM, Stovall MA, Marsden HB, Potok MHN, Kingston JE, Chessells JM (1992) Epipodophyllotoxins, alkylating agents, and radiation and risk of secondary leukaemia after childhood cancer. BMJ 304 (6832): 951–958.
Hawkins MM, Lancashire ER, Winter DL, Frobisher C, Reulen RC, Taylor AJ, Stevens MCG, Jenney M (2008) The British Childhood Cancer Survivor Study: objectives, methods, population structure, response rates and initial descriptive information. Pediatr Blood Cancer 50 (5): 1018–1025.
Inskip PD, Robison LL, Stovall M, Smith SA, Hammond S, Mertens AC, Whitton JA, Diller L, Kenney L, Donaldson SS, Meadows AT, Neglia JP (2009) Radiation dose and breast cancer risk in the Childhood Cancer Survivor Study. J Clin Oncol 27 (24): 3901–3907.
John EM, McGuire V, Thomas D, Haile R, Ozcelik H, Milne RL, Felberg A, West DW, Miron A, Knight JA, Terry MB, Daly M, Buys SS, Andrulis IL, Hopper JL, Southey MC, Giles GG, Apicella C, Thorne H, Whittemore AS (2013) Diagnostic chest X-rays and breast cancer risk before age 50 years for BRCA1 and BRCA2 mutation carriers. Cancer Epidemiol Biomarkers Prev 22 (9): 1547–1556.
Kleinerman RA, Tucker MA, Tarone RE, Abramson DH, Seddon JM, Stovall M, Li FP, Fraumeni JF Jr (2005) Risk of new cancers after radiotherapy in long-term survivors of retinoblastoma: an extended follow-up. J Clin Oncol 23 (10): 2272–2279.
Kleinerman RA, Yu C-L, Little MP, Li Y, Abramson D, Seddon J, Tucker MA (2012) Variation of second cancer risk by family history of retinoblastoma among long-term survivors. J Clin Oncol 30 (9): 950–957.
Knudson AG Jr (1971) Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci USA 68 (4): 820–823.
Kubota Y, Fujinami K, Uemura H, Dobashi Y, Miyamoto H, Iwasaki Y, Kitamura H, Shuin T (1995) Retinoblastoma gene mutations in primary human prostate cancer. Prostate 27 (6): 314–320.
Land CE (1980) Estimating cancer risks from low doses of ionizing radiation. Science 209 (4462): 1197–1203.
Ligot L, Diallo I, Shamsaldin A, Chavaudra J, Bonaîti-Pellié C, de Vathaire F (1998) Individualized phantom based on CT slices and auxological data (ICTA) for dose estimations following radiotherapy for skin haemangioma in childhood. Radiother Oncol 49 (3): 279–285.
Little MP, de Vathaire F, Shamsaldin A, Oberlin O, Campbell S, Grimaud E, Chavaudra J, Haylock RGE, Muirhead CR (1998) Risks of brain tumour following treatment for cancer in childhood: Modification by genetic factors, radiotherapy and chemotherapy. Int J Cancer 78 (3): 269–275.
Little MP, Kleinerman RA, Stiller CA, Li G, Kroll ME, Murphy MFG (2012) Analysis of retinoblastoma age incidence data using a fully stochastic cancer model. Int J Cancer 130 (3): 631–640.
Little MP, Muirhead CR, Haylock RGE, Thomas JM (1999) Relative risks of radiation-associated cancer: comparison of second cancer in therapeutically irradiated populations with the Japanese atomic bomb survivors. Radiat Environ Biophys 38 (4): 267–283.
Little MP, Wakeford R, Lubin JH, Kendall GM (2010) The statistical power of epidemiological studies analyzing the relationship between exposure to ionizing radiation and cancer, with special reference to childhood leukemia and natural background radiation. Radiat Res 174 (3): 387–402.
Lundell M, Mattsson A, Karlsson P, Holmberg E, Gustafsson A, Holm L-E (1999) Breast cancer risk after radiotherapy in infancy: a pooled analysis of two Swedish cohorts of 17,202 infants. Radiat Res 151 (5): 626–632.
Marees T, Moll AC, Imhof SM, de Boer MR, Ringens PJ, van Leeuwen FE (2008) Risk of second malignancies in survivors of retinoblastoma: more than 40 years of follow-up. J Natl Cancer Inst 100 (24): 1771–1779.
Mehta CR, Patel NR (1986) Algorithm 643. FEXACT: A FORTRAN subroutine for Fisher’s exact test on unordered r*c contingency tables. ACM Trans Math Software 12 (2): 154–161.
Miyamoto H, Shuin T, Torigoe S, Iwasaki Y, Kubota Y (1995) Retinoblastoma gene mutations in primary human bladder cancer. Br J Cancer 71 (4): 831–835.
Pijpe A, Andrieu N, Easton DF, Kesminiene A, Cardis E, Noguès C, Gauthier-Villars M, Lasset C, Fricker J-P, Peock S, Frost D, Evans DG, Eeles RA, Paterson J, Manders P, van Asperen CJ, Ausems MGEM, Meijers-Heijboer H, Thierry-Chef I, Hauptmann M, Goldgar D, Rookus MA, van Leeuwen FE (2012) Exposure to diagnostic radiation and risk of breast cancer among carriers of BRCA1/2 mutations: retrospective cohort study (GENE-RAD-RISK). BMJ 345: e5660.
Preston DL, Mattsson A, Holmberg E, Shore R, Hildreth NG, Boice JD Jr (2002) Radiation effects on breast cancer risk: a pooled analysis of eight cohorts. Radiat Res 158 (2): 220–235.
Preston DL, Ron E, Tokuoka S, Funamoto S, Nishi N, Soda M, Mabuchi K, Kodama K (2007) Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiat Res 168 (1): 1–64.
Pukkala E, Verkasalo PK, Ojamo M, Rudanko S-L (1999) Visual impairment and cancer: a population-based cohort study in Finland. Cancer Causes Control 10 (1): 13–20.
Reis-Filho JS, Tutt ANJ (2008) Triple negative tumours: a critical review. Histopathology 52 (1): 108–118.
Reulen RC, Taylor AJ, Winter DL, Stiller CA, Frobisher C, Lancashire ER, McClanahan FM, Sugden EM, Hawkins MM (2008) Long-term population-based risks of breast cancer after childhood cancer. Int J Cancer 123 (9): 2156–2163.
Ron E, Ikeda T, Preston DL, Tokuoka S (2005) Male breast cancer incidence among atomic bomb survivors. J Natl Cancer Inst 97 (8): 603–605.
Shamsaldin A, Lundell M, Diallo I, Ligot L, Chavaudra J, de Vathaire F (2000) Estimation of the radiation dose from radiotherapy for skin haemangiomas in childhood: the ICTA software for epidemiology. Phys Med Biol 45 (12): 3589–3599.
Stovall M, Weathers R, Kasper C, Smith SA, Travis L, Ron E, Kleinerman R (2006) Dose reconstruction for therapeutic and diagnostic radiation exposures: use in epidemiological studies. Radiat Res 166 (1 Pt 2): 141–157.
Travis LB, Hill DA, Dores GM, Gospodarowicz M, van Leeuwen FE, Holowaty E, Glimelius B, Andersson M, Wiklund T, Lynch CF, Van’t Veer MB, Glimelius I, Storm H, Pukkala E, Stovall M, Curtis R, Boice JD Jr., Gilbert E (2003) Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA 290 (4): 465–475.
Treré D, Brighenti E, Donati G, Ceccarelli C, Santini D, Taffurelli M, Montanaro L, Derenzini M (2009) High prevalence of retinoblastoma protein loss in triple-negative breast cancers and its association with a good prognosis in patients treated with adjuvant chemotherapy. Ann Oncol 20 (11): 1818–1823.
Tucker MA, D’Angio GJ, Boice JD Jr, Strong LC, Li FP, Stovall M, Stone BJ, Green DM, Lombardi F, Newton W, Hoover RN, Fraumeni JF Jr (1987) Bone sarcomas linked to radiotherapy and chemotherapy in children. N Engl J Med 317 (10): 588–593.
Varley JM, Armour J, Swallow JE, Jeffreys AJ, Ponder BAJ, T'Ang A, Fung Y-KT, Brammar WJ, Walker RA (1989) The retinoblastoma gene is frequently altered leading to loss of expression in primary breast tumours. Oncogene 4 (6): 725–729.
Verkasalo PK, Pukkala E, Stevens RG, Ojamo M, Rudanko S-L (1999) Inverse association between breast cancer incidence and degree of visual impairment in Finland. Br J Cancer 80 (9): 1459–1460.
Weinberg RA (1995) The retinoblastoma protein and cell cycle control. Cell 81 (3): 323–330.
Yu C-L, Tucker MA, Abramson DH, Furukawa K, Seddon JM, Stovall M, Fraumeni JF Jr, Kleinerman RA (2009) Cause-specific mortality in long-term survivors of retinoblastoma. J Natl Cancer Inst 101 (8): 581–591.
Acknowledgements
We are grateful for the technical assistance of Jeremy Miller and the detailed and helpful comments of Dr Peter Inskip, Dr Ethel Gilbert, and the two referees. This work was supported by the Intramural Research Program of the National Institutes of Health, the National Cancer Institute (NCI), Division of Cancer Epidemiology and Genetics.
Disclaimer
The study sponsor (NCI) played no role in study design and the collection, analysis, interpretation of data, the writing of the article and the decision to submit it for publication. MPL, MAT and RAK are employees of NCI. All researchers had access to all the data. All anonymised data used in the paper can be provided upon request upon application to the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Little, M., Schaeffer, M., Reulen, R. et al. Breast cancer risk after radiotherapy for heritable and non-heritable retinoblastoma: a US–UK study. Br J Cancer 110, 2623–2632 (2014). https://doi.org/10.1038/bjc.2014.193
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2014.193
Keywords
This article is cited by
-
Long-term risk of subsequent cancer incidence among hereditary and nonhereditary retinoblastoma survivors
British Journal of Cancer (2021)
-
High-energy particle beam and gamma radiation exposure, familial relatedness and cancer in mice
British Journal of Cancer (2017)