Abstract
Background:
As sodium, potassium and fluid intake are related to hypertension, an established risk factor for renal cell cancer (RCC), they may be independent risk factors for RCC.
Methods:
The Netherlands Cohort Study (NLCS) with case-cohort design included 120 852 participants aged 55–69 years. At baseline, diet and lifestyle were assessed with questionnaires. After 17.3 years of follow-up, 485 RCC cases and 4438 subcohort members were available for analyses.
Results:
Sodium intake increased RCC risk (P-trend=0.03), whereas fluid and potassium intake did not. For high sodium and low fluid intake, the RCC risk additionally increased (P-interaction=0.02).
Conclusion:
Sodium intake is a potential risk factor for RCC, particularly if fluid consumption is low.
Similar content being viewed by others
Main
The suggested risk factor pattern for renal cell cancer (RCC), including an increased risk with hypertension, smoking and obesity and a decreased risk with moderate alcohol consumption (Chow et al, 2010) also determines cardiovascular disease risk. In addition, evidence clearly suggests that high sodium intake may cause a rise in blood pressure, the development of hypertension (De Wardener and Macgregor, 2002) and affects renal function (Macgregor, 1997; De Wardener et al, 2004; Susic and Frohlich, 2012). Furthermore, prolonged sodium excess may contribute directly to kidney damage (Kotchen et al, 2013). Therefore, high sodium intake may be a risk factor for RCC, potentially through hypertension.
The effect of sodium on blood pressure may, however, be modified by potassium intake or fluid intake, given their influence on blood pressure regulation and sodium homeostasis, which are both key functions of the kidney (Whelton et al, 1997; Rose and Post, 2001). That considered, potassium intake and fluid intake may individually influence RCC risk, or modify potential effects of sodium intake on RCC risk. Until now, only few studies investigated the potential association between RCC risk and sodium intake, potassium intake (Mellemgaard et al, 1996) or fluid intake (Lee et al, 2006; Hu et al, 2009; Allen et al, 2011). In these studies, no attention has been given to their joint effects on renal function or on the potential influence of hypertension. In this study, we investigate whether sodium, potassium and fluid intake and their potential interactions are associated with RCC risk in a prospective study.
Materials and methods
The present study is conducted within the Netherlands Cohort Study (NLCS), a prospective cohort study including 120 852 participants aged 55–69 years at baseline (Van Den Brandt et al, 1990). The case-cohort design was used for efficiency in questionnaire processing and follow-up (Prentice, 1986). All cohort members were followed up for cancer occurrence, whereas the subcohort was followed up for vital status to estimate person years at risk for the entire cohort. All participants completed a baseline questionnaire on dietary habits and lifestyle. Details on the dietary assessment in the NLCS are available online (Supplementary Information). In brief, a 150-item, food frequency questionnaire (FFQ) represented the dietary part of the questionnaire (Goldbohm et al, 1994, 1995). Intakes of sodium, potassium and fluid were calculated using the computerised Dutch food composition table (Nevo tabel, 1986). Sodium and potassium intake were adjusted for total energy intake using the residual method (Willett and Stampfer, 1986). Sodium intake did not include sodium from added salt, yet the baseline questionnaire included specific questions on salt added during home-preparation or before consumption (Van Den Brandt et al, 2003), from which discretionary salt intake was calculated (Supplementary Information). In addition, information on salt preference was available (Supplementary Information).
After 17.3 years of follow-up, 485 histological confirmed, epithelial RCC cases and 4438 subcohort members with complete dietary information were included in Cox proportional hazards analyses adjusted for the case-cohort design (Barlow, 1994). Associations between sodium, potassium and fluid intake and RCC risk were analysed in the total population, by hypertension status and when participants with a low-salt diet were excluded, as these subpopulations may differ in dietary behaviours, so influencing the associations under study. Confounders were selected a priori and included age, energy intake and RCC risk factors (i.e. sex, BMI, hypertension, smoking, alcohol consumption). Robustness of data was investigated by excluding the first two years of follow-up and by reanalysing data separately for the first and second half of follow-up. Interactions with sodium and discretionary salt intake were investigated for potassium and fluid intake and for RCC risk factors. A P-value<0.05 was considered significant. Data were analysed with STATA (version 12).
Results
Energy-adjusted sodium intake was lower in subcohort members than in RCC cases (Table 1). Discretionary salt intake, perceived saltiness, potassium intake and fluid intake were similar among RCC cases, subcohort members and quintiles of sodium intake.
Sodium intake was associated with an increased RCC risk (Table 2). In multivariable-adjusted analyses, we observed a significantly increasing trend across quintiles (P-trend=0.03) to a maximum in the highest quintile (HR(95% CI): 1.40(0.99–1.97)) and a significant increase in RCC risk per increment of 1 g per day (HR(95% CI): 1.07(1.00–1.15)). For discretionary salt intake, the RCC risk was u-shaped, with a significantly increased HR for non-users and a non-significantly increased HR for users in quartile 4 (vs 1) (HR(95% CI): 2.36(1.56–3.56) and 1.16(0.85–1.58), respectively). Only after excluding non-users, there was a significant increase in RCC risk per increment of 1 g per day (HR(95% CI): 1.04(1.00–1.08)). Furthermore, participants who indicated soups and restaurant food as being ‘much too salty’ (vs ‘good’) had the highest RCC risk (HR(95% CI): 1.70(1.24–2.33)). Fluid and potassium intake were not associated with RCC risk.
We observed no difference between multivariable-adjusted models with and without hypertension as confounder, indicating that mediation was not present (data not shown). In addition, no significant interactions between hypertension and any of the exposures under study regarding RCC risk were observed (Supplementary Table). In participants without hypertension, the RCC risk for discretionary salt intake (‘no’ vs quartile 1) was no longer significant (HR(95% CI): 1.74(0.84–3.63)). Excluding the first two years of follow-up or excluding participants with a low-salt diet did not change results (data not shown). However, the association between sodium intake and RCC risk clearly attenuated over time. We observed a higher HR for quintile 5 (vs 1) of sodium intake during the first nine years of follow-up and a lower HR during the second nine years of follow-up (HR(95% CI): 1.71(1.08–2.71) and 1.12(0.69–1.82), respectively).
There was a significant interaction between sodium and fluid intake, but not between sodium and potassium intake regarding RCC risk (P-interaction=0.02 and 0.73, respectively; Table 3). Participants with high sodium and low fluid intake compared to those with low sodium and low fluid intake had a higher RCC risk (HR(95% CI): 1.91(1.10–3.32)). Other interactions between sodium or discretionary salt intake and RCC risk factors were not significant (data not shown).
Discussion
To our knowledge, this is the first prospective study to investigate sodium, potassium and fluid intake and their interactions as potential risk factors for RCC. For sodium intake, the association with RCC risk has been reported in a case-control study, showing a decreased risk for higher sodium intake in men, but not in women (Mellemgaard et al, 1996). In the present study, we observed an increased RCC risk for higher sodium intake and no interaction between sex and sodium intake for RCC risk. In addition, we found no indications for mediation or effect-modification by hypertension, suggesting that sodium intake may be associated with RCC risk independently of hypertension. Fluid intake was not associated with RCC risk, which is in line with previous prospective cohort studies (Lee et al, 2006; Allen et al, 2011), but not with a case-control study showing an increased RCC risk for higher fluid intake (Hu et al, 2009). All studies, however, ignored potential confounding by or effect-modification through sodium intake. Yet, we observed an interaction between sodium and fluid intake for RCC risk, which supports our hypothesis that the balance between sodium and fluid intake is important in RCC aetiology. Potassium intake was not associated with RCC risk, which is similar to previous research (Mellemgaard et al, 1996).
We recognise that salt (sodium chloride) intake is a difficult concept to measure accurately, particularly with questionnaires. However, our baseline questionnaire was specifically designed to study salt intake as it additionally included specific questions on discretionary salt intake. Although the FFQ was able to rank individuals adequately according to sodium intake when compared to nine-day dietary records (Goldbohm et al, 1994; Van Den Brandt et al, 2003), information on the validity of discretionary salt intake was not available. Nevertheless, the mean salt intake (sodium from ready-to-eat foods plus discretionary salt) in our population (8.7 g per day) is comparable to that of the Dutch population in 1986 (Nederlandse Voedingsraad, 1986).
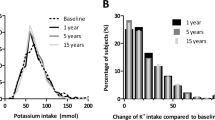
Exposures were only assessed at baseline. Although nutrient intakes were rather stable during the first five years follow-up (Goldbohm et al, 1995), they may have changed during later follow-up, possibly explaining the attenuation in risk estimate over time.
Compared to sodium intake, which is calculated using standardised measurement units of the FFQ, the inter-individual range of discretionary salt intake is very large (up to factor 10). To capture all variability, it might be desirable to combine both indicators of sodium intake into one overall intake variable. However, discretionary salt intake is highly influenced by habits, attitudes and beliefs (Shepherd and Farleigh, 1986). In fact, those who wish to reduce salt intake may particularly reduce discretionary salt intake. The observed u-shape in RCC risk for discretionary salt intake may perhaps reflect one’s ability to reduce discretionary salt intake to prevent or control hypertension. Indeed, participants with hypertension were overrepresented in the lowest category of discretionary salt intake (data not shown). Therefore, an overall intake variable was less informative than both individual indicators of sodium intake separately, as HRs for this overall variable fully reflected the arbitrary combination of a linear and u-shaped trend (data not shown).
We used high-perceived saltiness as an indicator of low-salt preference. Salt preference may indicate actual sodium intake, although no consensus has been reached (Mattes, 1997). Indeed, we observed an inverse relation with perceived saltiness for discretionary salt intake (P<0.001), but not for sodium intake (P=0.86). The association between high-perceived saltiness and RCC risk was, however, in opposite direction as expected, as previously observed for stomach cancer (Van Den Brandt et al, 2003). Perhaps, this association may be explained by the hedonic shift, in which the taste of reduced-sodium products becomes more acceptable over time (Mattes, 1997).
The mechanism through which sodium intake may influence RCC risk is unknown. Perhaps, high renal sodium load constitutes to RCC carcinogenesis through inflammation, as sodium is suggested to have inflammatory properties, which can have tumour-promoting consequences (Fiore et al, 2011; Hanahan and Weinberg, 2011).
In conclusion, sodium intake is a potential risk factor for RCC, particularly if fluid consumption is low, but potassium and fluid intake are not associated with RCC risk. However, these findings await confirmation in other prospective studies and for specific RCC subtypes. Special attention should be given to the role of hypertension and other related diseases, such as end-stage renal disease, in the association between sodium intake and RCC risk.
Change history
04 February 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Allen NE, Balkwill A, Beral V, Green J, Reeves G (2011) Fluid intake and incidence of renal cell carcinoma in UK women. Br J Cancer 104: 1487–1492.
Barlow WE (1994) Robust variance estimation for the case-cohort design. Biometrics 50: 1064–1072.
Chow WH, Dong LM, Devesa SS (2010) Epidemiology and risk factors for kidney cancer. Nat Rev Urol 7: 245–257.
De Wardener HE, He FJ, Macgregor GA (2004) Plasma sodium and hypertension. Kidney Int 66: 2454–2466.
De Wardener HE, Macgregor GA (2002) Sodium and blood pressure. Curr Opin Cardiol 17: 360–367.
Fiore MC, Jimenez PM, Cremonezzi D, Juncos LI, Garcia NH (2011) Statins reverse renal inflammation and endothelial dysfunction induced by chronic high salt intake. Am J Physiol Renal Physiol 301: F263–F270.
Goldbohm RA, Van ’T Veer P, Van Den Brandt PA, Van ’T Hof MA, Brants HA, Sturmans F, Hermus RJ (1995) Reproducibility of a food frequency questionnaire and stability of dietary habits determined from five annually repeated measurements. Eur J Clin Nutr 49: 420–429.
Goldbohm RA, Van Den Brandt PA, Brants HA, Van’t Veer P, Al M, Sturmans F, Hermus RJ (1994) Validation of a dietary questionnaire used in a large-scale prospective cohort study on diet and cancer. Eur J Clin Nutr 48: 253–265.
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144: 646–674.
Hu J, Mao Y, Desmeules M, Csizmadi I, Friedenreich C, Mery L (2009) Total fluid and specific beverage intake and risk of renal cell carcinoma in Canada. Cancer Epidemiol 33: 355–362.
Kotchen TA, Cowley Jr AW, Frohlich ED (2013) Salt in health and disease—a delicate balance. N Engl J Med 368: 1229–1237.
Lee JE, Giovannucci E, Smith-Warner SA, Spiegelman D, Willett WC, Curhan GC (2006) Total fluid intake and use of individual beverages and risk of renal cell cancer in two large cohorts. Cancer Epidemiol Biomarkers Prev 15: 1204–1211.
Macgregor GA (1997) Salt—more adverse effects. Am J Hypertens 10: 37S–41S.
Mattes RD (1997) The taste for salt in humans. Am J Clin Nutr 65: 692S–697S.
Mellemgaard A, Mclaughlin JK, Overvad K, Olsen JH (1996) Dietary risk factors for renal cell carcinoma in Denmark. Eur J Cancer 32a: 673–682.
Nederlandse Voedingsraad (1986) Vermindering gebruik keukenzout: eindadvies. Den Haag: Nederlandse Voedingsraad.
Nevo tabel (1986) Dutch food composition table 1986-1987; Nederlands voedingsstoffenbestand 1986-1987. Voorlichtingsbureau voor de Voeding: The Hague, The Netherlands.
Prentice RL (1986) On the design of synthetic case-control studies. Biometrics 42: 301–310.
Rose BD, Post TW (2001) Clinical Physiology of Acid-Base and Electrolyte Disorders. McGraw-Hill, Medical Publishing Division: New York, NY, USA.
Shepherd R, Farleigh CA (1986) Attitudes and personality related to salt intake. Appetite 7: 343–354.
Susic D, Frohlich ED (2012) Salt consumption and cardiovascular, renal, and hypertensive diseases: clinical and mechanistic aspects. Curr Opin Lipidol 23: 11–16.
Van Den Brandt PA, Botterweck AA, Goldbohm RA (2003) Salt intake, cured meat consumption, refrigerator use and stomach cancer incidence: a prospective cohort study (Netherlands). Cancer Causes Control 14: 427–438.
Van Den Brandt PA, Goldbohm RA, Van ‘T Veer P, Volovics A, Hermus RJ, Sturmans F (1990) A large-scale prospective cohort study on diet and cancer in The Netherlands. J Clin Epidemiol 43: 285–295.
Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, Klag MJ (1997) Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA 277: 1624–1632.
Willett W, Stampfer MJ (1986) Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124: 17–27.
Acknowledgements
This study was supported by the Netherlands Cancer Society. We are indebted to the participants of this study, and further wish to thank The Netherlands Cancer Registry and the Dutch Pathology Registry. We are grateful to Dr Maarten Christiaans, nephrologist at the Maastricht University Medical Centre for sharing his expert knowledge on renal physiology and to Henny Brants, research dietitian at TNO for her extensive efforts on the current data. Finally we thank Sacha van de Crommert, Jolanda Nelissen, Jacqueline Spronck, Conny de Zwart, Marijke Moll and Annemie Pisters, for their assistance with data entry or data management; and Harry van Montfort, Ton van Moergastel, Ellen Dutman, Ralph Meijer and Ruud Schmeitz for programming assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Deckers, I., van den Brandt, P., van Engeland, M. et al. Long-term dietary sodium, potassium and fluid intake; exploring potential novel risk factors for renal cell cancer in the Netherlands Cohort Study on diet and cancer. Br J Cancer 110, 797–801 (2014). https://doi.org/10.1038/bjc.2013.771
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.771
Keywords
This article is cited by
-
The association of healthy lifestyle index score and the risk of renal cell cancer in the Netherlands cohort study
BMC Cancer (2023)
-
Inactivation of epithelial sodium ion channel molecules serves as effective diagnostic biomarkers in clear cell renal cell carcinoma
Genes & Genomics (2023)
-
Kidney Cancer Integrative Oncology: Possible Options for Care
Current Oncology Reports (2023)
-
The Vitamin D status is associated with serum C-reactive protein and adhesion molecules in patients with renal cell carcinoma
Scientific Reports (2019)
-
Knowledge, Attitudes and Behaviours Related to Dietary Salt Intake in High-Income Countries: a Systematic Review
Current Nutrition Reports (2018)