Abstract
Background:
TMPRSS4 is a membrane-anchored protease involved in cell migration and invasion in different cancer types including lung cancer. TMPRSS4 expression is increased in NSCLC and its inhibition through shRNA reduces lung metastasis. However, molecular mechanisms leading to the protumorigenic regulation of TMPRSS4 in lung cancer are unknown.
Methods:
miR-205 was identified as an overexpressed gene upon TMPRSS4 downregulation through microarray analysis. Cell migration and invasion assays and in vivo lung primary tumour and metastasis models were used for functional analysis of miR-205 overexpression in H2170 and H441 cell lines. Luciferase assays were used to identify a new miR-205 direct target in NSCLC.
Results:
miR-205 overexpression promoted an epithelial phenotype with increased E-cadherin and reduced fibronectin. Furthermore, miR-205 expression caused a G0/G1 cell cycle arrest and inhibition of cell growth, migration, attachment to fibronectin, primary tumour growth and metastasis formation in vivo. Integrin α5 (a proinvasive protein) was identified as a new miR-205 direct target in NSCLC. Integrin α5 downregulation in lung cancer cells resulted in complete abrogation of cell migration, a decreased capacity to adhere to fibronectin and reduced in vivo tumour growth, compared with control cells. TMPRSS4 silencing resulted in a concomitant reduction of integrin α5 levels.
Conclusion:
We have demonstrated for the first time a new molecular pathway that connects TMPRSS4 and integrin α5 through miR-205 to regulate cancer cell invasion and metastasis. Our results will help designing new therapeutic strategies to inhibit this novel pathway in NSCLC.
Similar content being viewed by others
Main
Lung cancer is a critical problem in public health. It represents the most frequent tumour type in men and the second in women, and the 5-year survival rate remains inferior to 20% (Jemal et al, 2010). More than 60% of NSCLC patients present locally advanced, unresectable or metastatic (stage III/IV) tumours at the time of diagnosis, which fatally concludes in death within few months after diagnosis. In spite of the advent of targeted therapies, which has been a breakthrough for NSCLC management, only a small percentage of patients will benefit from them. Therefore, there is a need for identifying new potential therapeutic targets against which more effective treatments may be developed.
Altered expression of proteases is currently considered as a hallmark of cancer, as malignant cells need proteolytic activities to promote growth, motility and invasion (Roy et al, 2009). Type II transmembrane serine proteases (TTSPs) are characterised by the presence of an N-terminal transmembrane domain that anchors these proteases to the plasma membrane. TTSPs include 18 members that can be divided into four groups. Examples of TTSPs related to cancer are hepsin, matriptase, HAT/DESC and TMPRSS4 (Szabo and Bugge, 2008).
TMPRSS4 comprises a short N-terminal cytoplasmic domain, a transmembrane domain and a large extracellular domain that contains the catalytic activity. TMPRSS4 is synthesised as an inactive zymogen that needs to be activated (Netzel-Arnett et al, 2003). However, both the substrates and activators of this serine protease are largely unknown. TMPRSS4 participates in the regulation of cellular signalling events at the plasma membrane and in the extracellular matrix (Hooper et al, 2001). TMPRSS4 is upregulated in pancreatic, colon, lung, ovary and thyroid cancers, where it has been suggested as a diagnostic marker (Kebebew et al, 2005). In a previous work, we demonstrated that TMPRSS4 is highly expressed in lung tumours compared with normal lung, particularly in squamous cell carcinomas (SCC) as compared with adenocarcinomas (AC). We also demonstrated that high TMPRSS4 mRNA levels in SCC are associated with poor prognosis (Larzabal et al, 2011). Moreover, a knockdown strategy to reduce TMPRSS4 levels in lung tumour cells resulted in a significant impairment of metastasis in animal models (Larzabal et al, 2011).
Studies of biological activity in colon cancer have reported that elevated TMPRSS4 expression induces epithelial-to-mesenchymal transition (EMT) of cancer cells and promotes metastasis (Jung et al, 2008; Kim et al, 2010). Further analysis of TMPRSS4-mediated signalling in colon cancer cells suggested that multiple downstream signalling pathways are activated. These included Src, ERK1/2, AKT, FAK and Rac1, resulting in E-cadherin downregulation and induced expression of integrin α5β1, a critical adhesion molecule involved in the acquisition of an EMT phenotype and cell motility (Maschler et al, 2005). Inhibition of PI3K or Src with specific compounds decreases cell invasiveness and actin rearrangement mediated by TMPRSS4. Moreover, functional blockade of integrin α5β1 demonstrated that this integrin has an important role in TMPRSS4-mediated effects (Kim et al, 2010). In spite of these data, the molecular regulation of TMPRSS4 in cancer cells is poorly understood.
The aim of this study was to identify molecular mechanisms involved in the protumorigenic regulation of TMPRSS4 in NSCLC. Through a microarray analysis, we discovered that the miR-205 gene (MIR205HG) was consistently overexpressed upon TMPRSS4 downregulation. We demonstrate here that overexpression of miR-205 promotes an epithelial phenotype and inhibits tumour cell migration and metastasis formation in lung cancer models. Moreover, we have identified integrin α5β1 (a proinvasive protein) as a new miR-205 direct target in NSCLC; we also show a novel molecular mechanism that connects TMPRSS4 with integrin α5β1 through miR-205.
Materials and methods
Cell culture
All human lung cancer cell lines were obtained from the American Type Culture Collection (Manassas, VA, USA) and were maintained in RPMI (Sigma, Madrid, Spain) with 10% fetal bovine serum (Thermo Scientific, Waltham, MA, USA) and 1% penicillin-streptomycin (Lonza, Basel, Switzerland), at 37 °C and 5% CO2 atmosphere.
H358 and H441 cell clones with a reduction of TMPRSS4 (shTMP4) and their corresponding controls (carrying the empty vector; shCtrl) were previously described by our group (Larzabal et al, 2011).
Immortalised normal human bronchial epithelial cells (HBECs) have been previously characterised (Ramirez et al, 2004). These cell lines were kindly provided by Dr J.D. Minna (University of Texas Southwestern Medical Center, Dallas, TX, USA). Cells were maintained in keratinocyte serum-free medium supplemented with human recombinant epidermal growth factor (EGF) and bovine pituitary extract (Life Technologies, Carlsbad, CA, USA).
miRNA transfection
H2170, H441 and A549 cell lines were transfected with miRNASelect pEP-miR Null control vector or miRNASelect pEP-hsa-miR-205 vector (Cell Biolabs, San Diego, CA, USA) using GeneJuice reagent (Merck Millipore, Darmstadt, Germany). Transfected cell clones were selected with puromycin (2 μg ml−1).
Integrin α5 inhibition
We used integrin α5 shRNA lentiviral particles (Santa Cruz Biotechnology, Dallas, TX, USA) to inhibit integrin α5 expression in the H2170 cell line. Infection with shRNA was performed with polybrene according to the manufacturer’s protocol. Stable clones were selected with 1 μg ml−1 puromycin. The integrin α5 expression was analysed by western blot and qPCR.
RNA extraction and quantitative real-time PCR
RNA isolation and qPCR was carried out as previously described (Larzabal et al, 2011). Assays were performed to quantify mRNA levels of human E-cadherin, fibronectin, ZEB1/ZEB2 and integrin α5. The primer sequences are shown in Supplementary Table 1.
To detect mature miR-205 expression, TRIzol reagent (Invitrogen, Carlsbad, CA, USA) was used to isolate total RNA. For the quantification of this miRNA, stem-loop RT of 20 ng total RNA was run using the TaqMan MicroRNA Reverse Transcription kit (Applied Biosystems, Foster City, CA, USA) with specific primers for miR-205 and RNU48 as endogenous control (Applied Biosystems). Subsequently, the qPCR amplifications were performed with TaqMan 2 × Universal PCR Master Mix, No AmpErase UNG (Applied Biosystems) and specific primers for miR-205 and RNU48 (Applied Biosystems). Relative miR-205 levels were normalised to RNU48 expression. Data are given as 2−ΔΔCt or 2−ΔCt.
Proliferation and clonogenic assays
To determine proliferation of H2170 and H441 cells and their miR-205 expressing clones, 1200 cells per well were seeded in 96-well plates. Ninety-six hours after plating, MTT assays were performed following the manufacturer’s protocol (Sigma).
To evaluate the clonogenic potential of miR-205 expressing clones, 500 cells per well were plated into six-well plates in adherent conditions. After 10 days in culture, colonies were fixed with 4% buffered formalin (Panreac, New Jersey, NY, USA) and stained with 2% crystal violet. The number of colonies per well was determined.
Anchorage-independent growth assay
Soft-agar assay was used to determine the ability of miR-205-expressing clones to grow under anchorage-independent conditions. Each well of a six-well plate was coated with culture medium containing 0.6% agarose. Upon solidification, a layer of 0.3% agar in culture medium carrying 2000 cells per well was placed on top of the agarose. Colonies were stained with MTT and counted after 2 weeks of incubation.
Cell cycle analysis
For cell cycle distribution analysis, adherent and floating cells were fixed in 70% ethanol for 1 h (or until analysis) at 4 °C. Cells were then rehydrated in PBS, treated with RNase A (0.2 mg ml−1, Sigma) for 1 h at 37 °C and stained with 7AAD (0.02 mg ml−1, Sigma). Cells were analysed in a flow cytometer (FACSCalibur, BD). Percentages of cells in the Sub-G0, G0/G1, S and G2/M phases were determined.
Migration assays
Migration assays were conducted in a Boyden chamber for the H2170 and A549 cell lines. A total of 15 000 cells per well in serum-free medium were seeded in the upper transwell of 24-well plates (Costar, Tewksbury, MA, USA). Medium with 10% of serum was used as a chemoattractant and was placed in the lower compartment. After 48 h, cells in the top chamber were wiped with a cotton swab, and cells in the lower compartment were fixed with 4% formalin and stained with crystal violet. The number of migratory cells was evaluated with a Leica DMIL LED microscope using the LAS EZ software (Leica Microsystems, Wetzlar, Germany).
H441 cells did not migrate through the transwell in Boyden chambers (unpublished observations). For this reason, we examined migration of this cell line with an in vitro model of wound healing. Cells were grown until confluence, and a 20-p micropipette tip was used to create a linear scratch in the monolayer. Pictures of the wounds were taken right after the scratching and 24 h later with a Nikon Eclipse photomicroscope (Nikon, Kingston, UK) using the ACT-2U1.6 software (Nikon). The empty surface between the wound edges was measured with the TScratch analysis software (Zurich, Switzerland).
Adhesion assay
Single-cell suspensions were rinsed with serum-free medium supplemented with 0.5% BSA, and 30 000 cells per well were seeded in 96-well plates precoated with 3% BSA (control), fibronectin (20 μg ml−1 per well) or collagen type I (50 μg ml−1 per well). After 30 min incubation to let cells adhere to the substrates at 37 °C, wells were washed with PBS to remove the floating cells. Attached cells were fixed in 4% paraformaldehyde and stained with 0.5% toluidine blue. To obtain the adherent cell number, stained cells were treated with 1% SDS, and the absorbance at 595 nm was measured using a Sunrise spectrophotometer (Tecan, San Jose, CA, USA).
E-cadherin and fibronectin immunofluorescence
Control cells and miR-205-expressing cell clones were grown in slide chambers until confluence. Cells were fixed by immersion in acetone:methanol (1 : 1) solution for 10 min at −20 °C. Then, non-specific binding sites were blocked with 2% BSA, and slides were incubated with primary anti-E-cadherin (BD Bioscience, San Jose, CA, USA) or anti-fibronectin (Abcam, Cambridge, UK) antibodies at 1 : 100 dilution for 2 h at room temperature. Slides were then incubated in darkness with the secondary antibody (488 Alexa Fluor dye, Invitrogen) for 1 h at room temperature. For nuclei staining, samples were incubated with 0.1 mg ml−1 DAPI. A hydrophilic mounting medium (SlowFade antifade) was used, and coverslips were sealed with nail polish. For visualisation and acquisition of images, an Axio Imager Z1 (ZEISS) epifluorescence microscope equipped with a CoolSnap CCD camera was used.
Microarray hybridisation and bioinformatic analysis
Transcriptional profiling was done with the Affymetrix Human Gene 1.0 ST microarray according to the manufacturer’s protocol. Both background correction and normalisation were done with RMA (Robust Multichip Average) algorithm (Irizarry et al, 2003). Then, a filtering process was performed to eliminate low expression probe set intensities for each probe, recorded in CEL files and data were analysed. The analysis of significant gene expression changes in shTMP4 samples compared with expression in control cells was performed by Z-score transformation of fold-change distributions (Cheadle et al, 2003). A threshold of |z|>2.3 (P-value<0.01) was set to select genes for further analysis. The selection of genes differentially expressed in miR-205-overexpressing cells with respect to control cells was performed using the criteria based on the fold-change value. Probe sets were selected as significant using a cutoff value of 2. The set of differentially expressed genes was compared with the miRNA-predicted targets stored in public databases (Betel et al, 2008; Griffiths-Jones et al, 2008; Friedman et al, 2009). As a result, putative microRNA target genes with altered expression were identified.
Western blotting
Protein extraction and western blot were carried out as previously described (Ponz-Sarvise et al, 2011). The primary antibodies (diluted at 1 : 1000) were as follows: anti-human ITGα5 (Sigma), anti phospho-Src (Cell Signaling, Danvers, MA, USA) and anti-Src (Cell Signaling). An anti-human β-actin antibody (Sigma) at 1 : 10 000 dilution was used as a loading control. Horseradish peroxidase-labelled secondary antibodies (GE Healthcare, Waukesha, WI, USA) against the corresponding primary antibodies were used. Immunoreactive bands were visualised by a chemiluminescent method using the Lumi-lightPLUS kit (Roche, Palo Alto, CA, USA).
Generation of H2170 TGL-expressing cells for in vivo imaging
Amphopack-293 packaging cells (Clontech, Madison, WI, USA) cultured with DMEM and 10% fetal bovine serum were transfected with the pSFGNESTGL purified plasmid as previously described (Larzabal et al, 2011). After 48 h in culture, virus containing supernatant was added to parental H2170 cells and H2170-miR-205-expressing cell clones. To increase the efficiency of infection, 7.5 μg ml−1 polybrene (Sigma) was added to the virus containing supernatants. Vector containing GFP+ cells were sorted by FACS (FACSAria Ilu). More than 90% of the cells were confirmed to express the reporter construct (Supplementary Figure 1A).
In vivo experiments
Animal studies were carried out according to the ethical guidelines established by our Institution (University of Navarra), under an approved animal protocol (069/11). For the lung metastasis model, 1.5 × 106 H2170 cells containing the control vector (miR-Scr) or the miR-205 overexpressing clones (miR-205#2 or miR-205#3) infected with the TGL reporter vector were injected in the tail vein in NOD SCID ILRβ2 null (NSG) mice. Four mice per group were used. Lung tumour development was monitored by detection of luciferase photon emission, using a Xenogen (Xenogen Inc., Alameda, CA, USA) (IVIS 100 series) living image system. Anaesthetised mice were injected intraperitoneally with 3 mg of D-Luciferin (Promega, Fitchburg, WI, USA) diluted in PBS, 5 min before light caption. The image acquisition time was in the range of 5 min. Data analyses were performed with the Living Image Igor Pro (Xenogen) software coupled to the IVIS system. Photon counts were calculated for each mouse using a circular region of interest.
To study the effect of miR-205 on primary tumour growth, 10 × 106 H2170 cells and their corresponding miR-205-overexpressing clones (miR-205#2 or miR-205#3) were injected subcutaneously into the flanks of the mice in a 1 : 1 PBS/Matrigel solution (BD). A similar experiment was conducted to assess whether knockdown of ITGα5 (shITGα5 H2170 cells) would decrease primary tumour growth with respect to controls. Tumour volumes were calculated with the formula: V=length × (width)2/2.
Immunohistochemistry
Tumours were excised, fixed, paraffin-embedded and cut in 5 μm thick sections, which were placed on slides. Slides were deparaffinised, rehydrated and treated for 12 min with 3% H2O2 (Panreac) in water to quench the endogenous peroxidase activity. For caspase-3, antigen retrieval was performed by heating the sections in a microwave oven in 1 mM EDTA (pH 8). Tissues were then blocked with normal goat serum in TBS (30 min, RT). Incubation with the following primary antibodies was done overnight at 4 °C: anti-cleaved caspase-3 Asp175 (Cell Signaling) at 1 : 200 dilution, anti-PCNA (Clone PC10; Dako, Glostrup, Denmark) at 1 : 400 dilution and anti-integrin α5 (Sigma) at 1 : 50 dilution. After incubation with Envision anti-rabbit or anti-mouse system (Dako), peroxidase activity was developed with DAB (3,3′-diaminobenzidine; Dako). Finally, slides were counterstained with haematoxylin, dehydrated and mounted with DPX (VWR).
Renilla luciferase assay
The renilla luciferase constructs with the 3′-untranslated region (UTR) of ITGα5 were made with the following oligonucleotides:
ITGα5 3′UTR-F: 5′-CTAGAGAGGAGCTGGGGATCCCTCCGCCCTGTGAAGGAACCATGCACTGTGAAGGACCCTTGTGC-3′
ITGα5 3′UTR-R: 5′-GGCCGCACAAGGGTCCTTCACAGTGCATGGGGCGGAGGGATCCCCAGCTCCTCT-3′
ITGα5-3′UTR-Mut-F: 5′-CTAGAGAGGAGCTGGGGATCCTCAACCCCCAGACACTTGAGGTAGCCCTTGTGC-3′
ITGα5-3′UTR-Mut-R: 5′-GGCCGCACAAGGGCTACCTCAAGTGTCTGGGGGTTGAGGATCCCCAGCTCCTCT-3′
These oligonucleotides contain the target site sequence or the mutated version (indicated in bold letters), which is complementary to the seed sequence of miR-205. Hybridised oligonucleotides were ligated into the XbaI—NotI site of the renilla reporter vector (pRL-SV40; Promega). GeneJuice reagent was used to co-transfect the renilla- ITGα5-3′UTR vector or the Renilla- ITGα5-3′UTR-mut, and a control vector containing firefly luciferase (pGL3-basic; Promega), together with either pre-miR-205 or scramble precursor-miR vectors. Renilla luciferase activity was measured 48 h after transfection with the Dual-Luciferase System (Promega) in a Berthold Luminometer (Lumat LB 9507).
Statistical analysis
Statistical differences between groups were examined with the Student’s t-test or ANOVA for unpaired parametric variables and the Mann–Whitney U-test or Kruskal-Wallis for unpaired non-parametric variables. Normality was analysed with the Shapiro-Wilks test. Data were processed with the SPSS statistical software (SPSS-IBM Inc., Chicago, IL, USA) (version 17.0 for Windows SPSS) and GraphPad Prism 5 software (GraphPad Software Inc., San Diego, CA, USA). P-values lower than 0.05 were considered as statistically significant.
Results
TMPRSS4 knockdown upregulates miR-205 expression
Previous studies have shown that TMPRSS4 has a role in cell migration and invasion (Kim et al, 2010). We have demonstrated that TMPRSS4 expression is increased in NSCLC and that its inhibition through shRNA reduces lung metastasis (Larzabal et al, 2011). Because molecular mechanisms activated by TMPRSS4 are unknown, we used an shRNA strategy to knockdown this protease in H358 and H441 cells, in search of genes with an altered expression. Clones H358 shTMP4-2 and shTMP4-3 and H441 shTMP4 (with a reduced TMPRSS4 expression) were selected for the microarray analysis. We have previously shown that these clones have reduced proliferative and migratory ability compared with their respective controls (H358 shCtrl and H441 shCtrl) (Larzabal et al, 2011).
A list of 287 probes was found to be deregulated by >two-fold in the three cell clones analysed. From those, 176 probes corresponded to non-annotated sequences. We then focused our analysis in those genes whose expression trend was the same (either upregulation or downregulation) in the three clones (Figure 1A). Twenty-nine genes followed this pattern (12 of them overexpressed and 17 of them underexpressed). As expected, TMPRSS4 was one of the downregulated genes of this set. Other downregulated genes that have a role in cancer cell adhesion included DDR1 and CLEC18A. DDR1 has been shown to promote lung cancer metastasis to the bone, and its expression correlates with poor prognosis in NSCLC patients (Valencia et al, 2012).
(A) Hierarchical cluster diagram of differentially expressed genes in H358 and H441 shTMP4 cell clones compared with their respective controls (shCtrl). (B) Expression of miR-205 by qPCR in immortalised human lung cells (HBEC) and in lung cancer-derived cell lines. The RNA was isolated when cells reached 70% confluency in all cases. (C) An MTT assay performed 72 h after plating. An inhibition in the proliferation of H2170 and H441 cells transfected with miR-205 was observed. (D) Clonogenic assays showed a lower number of clones in H2170 and H441 cells with high miR-205 expression compared with controls. Representative images are shown. Data and error bars: mean±s.d. *P<0.05; **P<0.01; ***P<0.001. All these experiments were repeated at least three independent times.
One of the upregulated genes found in the list was MIR205HG. This microRNA has been described as a tumour suppressor gene in different tumour types (Song and Bu, 2009; Wu et al, 2009; Majid et al, 2011), a reason whereby we decided to further study its role in lung cancer. miR-205 expression in H358 and H441 shCtrl and shTMP4 cell clones was validated by qPCR (Supplementary Figure 1B).
miR-205 is downregulated in lung cancer cell lines
We first determined mRNA levels of miR-205 in a panel of immortalised non-malignant human lung cells and human lung cancer cell lines. Cancer cell lines did not express miR-205 (or had very low expression, as in the case for H358 cells) in comparison with immortalised HBEC cells (Figure 1B and Supplementary Table 2), suggesting a tumour suppressor role for miR-205 in lung cancer.
miR-205 regulates cell proliferation, cell cycle progression and anchorage-independent growth in lung cancer cell lines
The effects of miR-205 on lung cancer were studied by overexpressing miR-205 precursor molecules (pre-miR-205) in H2170 and H441 cell lines. Overexpression was confirmed by real-time PCR, and two clones for H2170 (miR-205#2 and #3) and for H441 (miR-205#3 and #4) were selected for functional assays (Supplementary Figures 1C and D).
Initially, we assessed whether ectopic expression of miR-205 had a biological effect on proliferation and clonogenicity. MTT proliferation assays indicated that cell clones overexpressing miR-205 had a reduction in cell proliferation rates compared with cells transfected with scramble vector (miR-Scr) in both cell lines tested (Figure 1C). Furthermore, the overexpression of miR-205 decreased clonogenic capacity of H2170 and H441 cell lines (Figure 1D). These data indicate that miR-205 inhibits cell growth in lung cancer cell lines. As anchorage-independent growth is strongly correlated with tumorigenicity, we then determined whether miR-205 would alter cell growth in soft agar. H2170 cell clones were plated in soft agar and incubated for 2 weeks before counting the number of colonies. As shown in Figure 2A, the ability to form colonies was almost abolished in miR-205-overexpressing clones compared with scramble control. The same results were observed in the H441 cell line (Supplementary Figure 1E).
(A) Soft agar assays demonstrated less capacity of H2170 miR-205-overexpressing clones to grow in non-adherent conditions than control cells. (B) Representative cell cycle distribution profiles of H2170 control cells (miR-Scr) and a miR-205-overexpressing clone (miR-205#2). Cell cycle distribution showed an arrest in the G0/G1 phase after miR-205 overexpression in the H2170 cell line, as revealed by an increase in the proportion of cells in this phase and a decrease in the S phase. (C) Migration of H2170 cells in Boyden chambers was strongly reduced by overexpression of miR-205. (D) Migration of H441 cells in wound healing assays was impaired as well in clones with high miR-205 levels. (E) Adhesion assay of H2170 miR-Scr, miR-205#2 and miR-205#3 clones to fibronectin (FNC). BSA was used as a negative control. Data and error bars show mean±s.d. *P<0.05. **P<0.01. All these assays were repeated at least three independent times.
A cell cycle analysis by flow cytometry was performed to determine whether the decrease in cell proliferation due to miR-205 upregulation was associated with a cycle arrest. Overexpression of miR-205 produced a significant increase in the percentage of cells in the G0/G1 phase (from 56.44±1.72% to 66.03±1.77%; P<0.05), along with a decrease in the S phase (Figure 2B), indicating that miR-205 induced a cell cycle arrest in the H2170 cell line. Similar results were observed in the H441 cell line (Supplementary Figure 1F).
miR-205 inhibits cell migration and adhesion to fibronectin and promotes an epithelial phenotype in lung cancer cells
We next investigated whether miR-205 would modify cell migration in lung cancer cells. For this purpose, H2170 control cells or clones with elevated miR-205 levels were subjected to a migration assay. As shown in Figure 2C, 48 h after plating, upregulation of miR-205 completely blocked the ability of cells to migrate. Migration assays in Boyden chamber could not be performed with the H441 cell line because, in our hands, these cells did not migrate through the transwells. To further confirm the effect of miR-205 on migration through transwells, A549 cells with miR-205 overexpression or control cells (carrying the empty vector) were also used. As shown in Supplementary Figure 1G, similar results to those found for H2170 cells were obtained. In addition, as an alternative to this assay using H441 cells, an in vitro wound healing assay was performed to analyse migration in these cells. Figure 2D and Supplementary Figure 2A show that overexpression of miR-205 caused a reduction in the ability of H441 cells to migrate.
To study the effects of miR-205 on cell–matrix adhesion, we cultured H2170 cells on different substrates. miR-205 overexpression decreased cell adhesion to fibronectin (Figure 2E) but not to collagen type I (Supplementary Figure 2B). A similar tendency was found for H441 cells, although results did not reach statistical significance (data not show).
Different studies have demonstrated that miR-205 regulates EMT by targeting ZEB2 (Gandellini et al, 2009; Matsushima et al, 2011). As shown in Figure 3A, ZEB1 and ZEB2 mRNA levels were strongly reduced in miR-205-overexpressing cells. The analysis of EMT markers by qPCR and immunofluorescence revealed a marked increase in E-cadherin along with a pronounced decrease in fibronectin in H2170 cells with miR-205 overexpression (Figures 3B–D). The effect of miR-205 on E-cadherin and fibronectin expression was similar (although less remarkable) in H441 cells compared with H2170 cells (Supplementary Figures 2C and D). These results show that miR-205 inhibits EMT and cell motility and promotes an epithelial phenotype.
(A) ZEB1 and ZEB2 mRNA levels were decreased in H2170 cells with an upregulation of miR-205. GAPDH was used as internal control. (B, C) Expression of E-cadherin (B) and fibronectin (C) in H2170 control cell (miR-Scr) and miR-205-overexpressing cell clones measured by qPCR. GAPDH was also used as internal control. (D) Representative immunofluorescence images ( × 400) of E-cadherin and fibronectin in H2170 miR-Scr, miR-205#2, and miR-205#3 clones. All the experiments were repeated at least three independent times.
miR-205 reduces primary tumour growth and lung metastasis
An in vivo assay was performed to investigate the role of miR-205 on primary tumour growth. Overexpression of miR-205 resulted in a significant reduction in tumour volumes (P<0.05) in animals xenotransplanted with both miR-205#2 and miR-205#3 H2170 clones, compared with mice injected with the miR-Scr control (Supplementary Figure 2E).
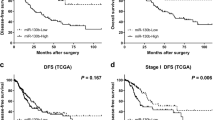
Furthermore, we used a xenograft model to analyse the effect of miR-205 on lung metastasis. In this case, animals were injected with the H2170 clones in the tail vein and monitored by bioluminescence until day 21. At day14th and 21st, a significant increase in light emission in the H2170 miR-Scr group was observed in comparison with the group injected with miR-205-overexpressing cells (Figures 4A and B). At the end of the study (day 21), animals were killed and lungs were examined for metastatic lesions. Histological analysis confirmed a less tumour burden in mice injected with cells that overexpressed miR-205 (Figure 4C). Immunohistochemical analysis of active caspase-3 revealed a higher proportion of apoptotic cells in tumours with increased levels of miR-205 (Figure 4D).
(A) Representative luminometric images of mice injected in the tail vein with 5 × 105 H2170 control or miR-205-expressing clones. (B) Photon emission quantification revealed a significant reduction in tumour burden in the groups injected with miR-205#2 and miR-205#3 cell clones. (C) Representative histological images of lungs from mice injected with H2170 miR-Scr or miR-205 overexpressing cells ( × 40). Numerous tumours are seen in control mice but not in the animals injected with cells that express miR-205. (D) Quantification of active caspase-3 in lung tumours. Measurements are given as relative area occupied by positive signals with respect to reference area. Significant increase in caspase-3 was found in mice injected with miR-205-overexpressing cells. Representative IHC images of caspase-3 immunostaining ( × 200) in tumour samples are shown. Data and error bars: mean±s.d. *P<0.05.
Identification of miR-205 targets
We wanted to address the molecular mechanism that causes miR-205 effects in lung cancer. We hypothesised that miR-205 could reduce the expression of target genes that induce EMT and inhibit cell invasion. To identify miR-205 target genes, we compared mRNA expression profiles in H2170 cells overexpressing miR-205 with those of controls (miR-Scr). By microarray analysis, 796 probes displayed a >two-fold reduction in expression as a result of miR-205 upregulation compared with controls. We searched within our gene list for putative-predicted miR-205 targets using publicly available and commonly used programs, such as TargetScan4, miRBase, PicTar and miRanda. Among the candidates, many were related with cell–cell and cell–matrix adhesion, cell invasion and metastasis (a selected list can be found in Supplementary Table 3). Importantly, one of the genes was integrin α5 (ITGα5), whose 3′-UTR sequence had a perfect complementarity with the seed sequence of miR-205 (Figure 5A).
(A) Sequence alignment of human miR-205 and the 3′-UTR of ITG α 5. The seed sequence (in bold letters) of miR-205 (top), 3′-UTR of ITGα5 (middle) and mutant 3′-UTR of ITGα5 (bottom) to generate the renilla reporter constructs is shown. (B) miR-205 overexpression reduced ITGα5 mRNA levels in the H2170 cell line. (C) miR-205 overexpression abrogated ITGα5 protein levels in H2170 cells. Protein expression was normalised to β-actin. (D) Phospho-Src in the H2170 cell clones. (E) Luciferase assay shows that miR-205 inhibited wild type but not mutated ITGα5-3′-UTR reporter activity. All these experiments were repeated at least three independent times.
Because ITGα5 is overexpressed in lung cancer (Dingemans et al, 2010), it promotes invasion of cancer cells (Hood and Cheresh, 2002) and its expression has been linked to TMPRSS4 in colon cancer (Kim et al, 2010), we focused our attention on this gene. We analysed whether endogenous ITGα5 mRNA and protein levels decreased when miR-205 was overexpressed. We found that miR-205 upregulation in H2170 or H441 lung cancer cells caused a significant reduction in endogenous ITGα5 mRNA levels (Figure 5B for H2170 cells and Supplementary Figure 2F for H441 cells) and protein levels (Figure 5C for H2170 cells and Supplementary Figure 2G for H441 cells). Moreover, Src signalling pathway activated by integrins was downregulated in H2170 cells with an overexpression of miR-205 (Figure 5D). To determine whether ITGα5 was a direct target of miR-205, we constructed renilla-based reporters that contained the wild-type or the mutated miR-205 target sequences of the ITGα5 3′-UTR. Ectopic expression of miR-205 inhibited the expression of the reporter vector containing the wild-type sequence of ITGα5 3′-UTR but not the reporter vector containing the mutation of the seed-miR-205 binding site in the two cell lines tested (Figure 5E for H2170 cells and Supplementary Figure 2H for H441 cells). These data show that ITGα5 is a direct target of miR-205 and that miR-205 can reduce ITGα5 mRNA and protein levels.
Knockdown of ITGα5 in lung cancer cells reduces cell migration and cell–matrix adhesion
To examine whether ITGα5 expression could mediate miR-205 regulation of cell proliferation and migration, shRNAs against ITGα5 were transfected in H2170 cells. ITGα5 shRNA efficiently decreased ITGα5 expression, as detected by western blot analysis (Figure 6A). ITGα5 depletion resulted in a complete abrogation of cell migration (Figure 6B) but no changes in cell proliferation or cell cycle distribution were observed (data not shown).
(A) Analysis of ITG α 5 by western blot in H2170 cells after infection with the shRNA targeting ITG α 5. (B) Migration of H2170 cells was completely blocked after inhibition of ITGα5. (C) The inhibition of ITGα5 resulted in a decrease in adhesion to fibronectin (FNC). BSA was used as a negative control. (D) Tumour volumes in mice injected with H2170 cells with reduced or wild-type levels of ITGα5. A delay in tumour growth was found in cells depleted in ITGα5. (E) Expression of ITGα5 in H358, H441 and H2170 cell lines after transfection with control shRNA or TMPRSS4-specific shRNA. Protein expression was normalised to β-actin. (F) Analysis of ITGα5 expression in a panel of 30 lung cancer cell lines measured by qPCR. Twenty-two cell lines were positive for this gene, 10 of which showed high expression. GAPDH was use as internal control. All the in vitro experiments were repeated at least three independent times.
As integrins are major adhesion molecules involved in cell-ECM interactions, we studied the effects of ITGα5 on cell–matrix adhesion. After culture of these cells on different substrates, we observed that ITGα5 levels modified the adhesiveness to fibronectin (Figure 6C) but not to collagen type I (data not shown). All these results provide evidence that inhibition of ITGα5 by miR-205 is responsible, at least in part, for the antitumorigenic effect observed in NSCLC cells with miR-205 upregulation.
Knockdown of ITGα5 inhibits tumour growth in vivo
To further explore whether ITGα5 knockdown would be responsible for the inhibition of tumour growth observed following miR-205 reconstitution, an in vivo experiment was performed. As shown in Figure 6D, subcutaneous xenotransplantation of H2170 cells with ITGα5 depletion caused a significant tumour shrinkage (P<0.05) in comparison with control cells.
Relationship between TMPRSS4 and ITGα5 expression
Having demonstrated that reduction of TMPRSS4 increases miR-205, which targets ITGα5, we studied levels of ITGα5 in shTMP4 cell clones. Figure 6E shows that, in agreement with previous results, ITGα5 levels were lower in shTMP4 clones than in controls, in the three cell lines tested. We also wondered whether there would be a correlation between ITGα5 and TMPRSS4 expression in cell lines. qPCR analysis for ITGα5 was conducted in 30 lung cancer cell lines and its expression was compared with that of TMPRSS4 in our previous publication (Larzabal et al, 2011). As shown in Figure 6F, 22 out of 30 cell lines expressed ITGα5. Eleven of the TMPRSS4 (+) cells expressed ITGα5 as well, but some TMPRSS4 (−) cells were positive for ITGα5 (Supplementary Table 4). This shows that ITGα5 may be regulated by other proteins in addition to TMPRSS4. On the basis of our findings, we propose a molecular mechanism through which TMPRSS4, regulating miR-205 expression, can modulate ZEB1, ZEB2 and ITGα5 levels to inhibit EMT and metastasis in lung cancer (Figure 7).
Discussion
TMPRSS4 has been shown to increase cell motility and invasion, to induce EMT and to promote metastasis in different cancer models, through multiple downstream signalling pathways involving ERK, AKT, Src and Rac1 (Kim et al, 2010). TMPRSS4 is upregulated in some cancer types, such as colon, pancreas, thyroid and lung (Wallrapp et al, 2000; Kebebew et al, 2005; Kim et al, 2010; Larzabal et al, 2011). Thus, this serine protease has emerged as a promising diagnostic and therapeutic target in cancer. Nonetheless, the molecular regulation of TMPRSS4 leading to these effects is still unknown. In the present study, we have identified a new molecular mechanism whereby TMPRSS4 regulates integrin α5 levels through the expression of miR-205. Because ITGα5 is strongly involved in the protumorigenic effects elicited by TMPRSS4, the data reported here about this novel molecular axis will help designing therapeutic strategies to inhibit this pathway. Moreover, in the present study we confirm the tumour suppressor role of miR-205 in lung cancer.
In order to elucidate the mechanism of action elicited by TMPRSS4 during EMT and metastasis formation, we conducted a microarray analysis where we compared gene expression profiles after TMPRSS4 inhibition in H358 and H441 lung cancer cell lines, with those of mock-transfected cells. As expected, the majority of genes with a differential expression were related with cell invasion and motility, in keeping with the functional role described for this serine protease in some tumour types (Jung et al, 2008; Kim et al, 2010). One of the upregulated genes was miR-205, a microRNA that has been described as a tumour suppressor (Song and Bu, 2009; Wu et al, 2009; Majid et al, 2011).
MicroRNAs (miRs) are small, non-coding RNAs that negatively regulate gene expression via translational repression or messenger RNA degradation (Bartel, 2004). MicroRNAs are involved in biologic and pathologic processes, including cell differentiation, proliferation and apoptosis (Kloosterman and Plasterk, 2006). Accumulating evidence indicates that deregulation of miRs is associated with the development of human cancers and suggests a causal role of miRs in tumour initiation and progression, as they can function as oncogenes or tumour suppressors (Caldas and Brenton, 2005; Chen, 2005). Recently, studies have shown that miR-205 regulates EMT through the modification of E-cadherin and other adhesion proteins (Bracken et al, 2009; Gibbons et al, 2009). Expression of the miR-200 family and miR-205 has been shown to be reduced in cells undergoing EMT. These miRs act by directly targeting the 3′-UTR sequence of ZEB1 and SIP1 (Gregory et al, 2008; Park et al, 2008). miR-205 has also been shown to suppress metastatic spread of human breast cancer xenografts in nude mice (Iorio et al, 2009) and to exert a tumour suppressor role by targeting HER3 receptor and VEGF-A in breast cancer (Iorio et al, 2009; Wu and Mo, 2009) and Src in renal cancer (Majid et al, 2011). In lung cancer, overexpression of miR-205 in cell lines hinders cell migration and invasion (Song and Bu, 2009) and its inhibition results in the acquisition of cancer stem cell and EMT properties, which favors tumour progression (Tellez et al, 2011). Consistent with these reports, we demonstrate that miR-205 was markedly downregulated in lung cancer cell lines compared with non-malignant HBEC lung epithelial cells. Its overexpression strongly reduced cell proliferation and clonogenic survival and caused G0/G1 cell cycle arrest. In addition, we show that forced expression of miR-205 in lung cancer cells impaired migratory and invasive capabilities. Furthermore, we demonstrate that miR-205 expression reduced lung metastasis formation and promoted an epithelial phenotype by inducing E-cadherin and decreasing fibronectin levels. However, the role of miR-205 in lung cancer remains controversial, since some studies indicate a high expression of this miRNA in lung cancer compared with normal lung tissue (Yanaihara et al, 2006; Markou et al, 2008; Lebanony et al, 2009). Interestingly, expression of miR-205 has been described as a biomarker to distinguish between AC and SCC (Hamamoto et al, 2013; Jiang et al, 2013). It is worth noticing though, that exposure of HBEC cells to tobacco carcinogens silences miR-205 expression through epigenetic mechanisms, leading to a dedifferentiation programme (Tellez et al, 2011). Moreover, epigenetic silencing of miRNAs with tumour suppressor features, including miR-205, is emerging as a common hallmark of human tumours (Lujambio et al, 2008).
Each miRNA has the potential to target hundreds of genes, which harbour sequences in their 3′-UTRs that are complementary to the seed region of the miRNA (Lim et al, 2005). Different targets of miR-205 have been described including, as previously mentioned, ZEB1 and SIP1 (Gregory et al, 2008), ERBB3 and VEGF-A (Wu et al, 2009), LDL receptor protein 1 (Song and Bu, 2009) and PKCɛ (Gandellini et al, 2009). In the present study, we have identified and validated for the first time ITGα5 as a new target of miR-205 in cancer.
Integrins are a family of cell adhesion proteins that activate diverse intracellular signalling molecules and reorganise the actin cytoskeleton to regulate attachment, survival and motility (Giancotti and Ruoslahti, 1999; Hood and Cheresh, 2002). In NSCLC, expression of particular integrins has been shown to predict the clinical course and prognosis of patients (Adachi et al, 2000; Gogali et al, 2004). ITGα5 binds to integrin β1 to give rise to the α5β1 heterodimer. Fibronectin stimulates the proliferation of lung cancer cells through α5β1 integrin receptor-mediated signalling; thus knockdown of this integrin reduces tumour burden (Roman et al, 2010). High expression of ITGα5 is associated with lower overall survival in patients with early stages of NSCLC (Dingemans et al, 2010). Moreover, high ITGα5 levels have been associated with poor prognosis in NSCLC patients with negative lymph nodes (Adachi et al, 2000). We show here that 22 out of 30 lung cancer cell lines analysed expressed ITGα5. Furthermore, inhibition of this integrin diminishes cancer cell migration, adhesion and tumour growth. These data suggest that ITGα5 may constitute a target worth studying in patients with NSCLC.
A close relationship between acquisition of EMT features and ITGα5 expression has been observed. Inhibition of E-cadherin in ovarian cancer cells causes upregulation of ITGα5 (Sawada et al, 2008). ZEB2, a transcription factor that represses E-cadherin, upregulates ITGα5 levels through cooperation with Sp1 to induce EMT and invasion in cancer cells (Nam et al, 2012). In this line, Kim et al (2010) pointed to TMPRSS4 as a new regulator of EMT in colon cancer and suggested that Src, FAK and ERK, which are major downstream effectors of integrins, appeared to be key signalling molecules involved in cell invasion and in the cadherin switch, presumably via regulation of ITGα5 expression. In agreement with these results, we show a downregulation of ITGα5 in H358, H441 and H2170 lung cancer cell lines with an inhibition of TMPRSS4, which confirms the regulation of ITGα5 by TMPRSS4. Therefore, it appears that targeting the novel TMPRSS4/miR-205/ITGα5 axis may be a promising strategy to inhibit EMT and metastasis in NSCLC. In this regard, an antibody targeting integrin α5β1 (volociximab, PDL Biopharma) has been developed and is being currently tested in phase II clinical trials for solid tumours (particularly for renal carcinoma).
In summary, our results provide evidence for the existence of a new molecular connection between two membrane-anchored proteins (ITGα5 and TMPRSS4) that cooperate to foster tumour growth, metastasis and migration, through miR-205. This new intracellular signalling pathway appears to have an important role in the development of lung cancer. TMPRSS4 blockade in tumour cells causes an overexpression of miR-205, resulting in an inhibition of the transcription factors ZEB1 and ZEB2, and ITGα5, which leads to a loss of EMT features. This, in turn, decreases cell–matrix interaction and cell invasiveness, hindering cell migration and metastasis formation. Biological or pharmacological approaches to block TMPRSS4 and ITGα5 may constitute an interesting novel approach to inhibit lung cancer.
Change history
04 February 2014
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adachi M, Taki T, Higashiyama M, Kohno N, Inufusa H, Miyake M (2000) Significance of integrin alpha5 gene expression as a prognostic factor in node-negative non-small cell lung cancer. Clin Cancer Res 6 (1): 96–101.
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116 (2): 281–297.
Betel D, Wilson M, Gabow A, Marks DS, Sander C (2008) The microRNA.org resource: targets and expression. Nucleic Acids Res 36 (Database issue): D149–D153.
Bracken CP, Gregory PA, Khew-Goodall Y, Goodall GJ (2009) The role of microRNAs in metastasis and epithelial-mesenchymal transition. Cell Mol Life Sci 66 (10): 1682–1699.
Caldas C, Brenton JD (2005) Sizing up miRNAs as cancer genes. Nat Med 11 (7): 712–714.
Cheadle C, Vawter MP, Freed WJ, Becker KG (2003) Analysis of microarray data using Z score transformation. J Mol Diagn 5 (2): 73–81.
Chen CZ (2005) MicroRNAs as oncogenes and tumor suppressors. N Engl J Med 353 (17): 1768–1771.
Dingemans AM, van den Boogaart V, Vosse BA, van Suylen RJ, Griffioen AW, Thijssen VL (2010) Integrin expression profiling identifies integrin alpha5 and beta1 as prognostic factors in early stage non-small cell lung cancer. Mol Cancer 9: 152.
Friedman RC, Farh KK, Burge CB, Bartel DP (2009) Most mammalian mRNAs are conserved targets of microRNAs. Genome Res 19 (1): 92–105.
Gandellini P, Folini M, Longoni N, Pennati M, Binda M, Colecchia M, Salvioni R, Supino R, Moretti R, Limonta P, Valdagni R, Daidone MG, Zaffaroni N (2009) miR-205 Exerts tumor-suppressive functions in human prostate through down-regulation of protein kinase Cepsilon. Cancer Res 69 (6): 2287–2295.
Giancotti FG, Ruoslahti E (1999) Integrin signaling. Science 285 (5430): 1028–1032.
Gibbons DL, Lin W, Creighton CJ, Zheng S, Berel D, Yang Y, Raso MG, Liu DD, Wistuba II, Lozano G, Kurie JM (2009) Expression signatures of metastatic capacity in a genetic mouse model of lung adenocarcinoma. PLoS One 4 (4): e5401.
Gogali A, Charalabopoulos K, Constantopoulos S (2004) Integrin receptors in primary lung cancer. Exp Oncol 26 (2): 106–110.
Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G, Vadas MA, Khew-Goodall Y, Goodall GJ (2008) The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol 10 (5): 593–601.
Griffiths-Jones S, Saini HK, van Dongen S, Enright AJ (2008) miRBase: tools for microRNA genomics. Nucleic Acids Res 36 (Database issue): D154–D158.
Hamamoto J, Soejima K, Yoda S, Naoki K, Nakayama S, Satomi R, Terai H, Ikemura S, Sato T, Yasuda H, Hayashi Y, Sakamoto M, Takebayashi T, Betsuyaku T (2013) Identification of microRNAs differentially expressed between lung squamous cell carcinoma and lung adenocarcinoma. Mol Med Rep 8 (2): 456–462.
Hood JD, Cheresh DA (2002) Role of integrins in cell invasion and migration. Nat Rev Cancer 2 (2): 91–100.
Hooper JD, Clements JA, Quigley JP, Antalis TM (2001) Type II transmembrane serine proteases. Insights into an emerging class of cell surface proteolytic enzymes. J Biol Chem 276 (2): 857–860.
Iorio MV, Casalini P, Piovan C, Di Leva G, Merlo A, Triulzi T, Menard S, Croce CM, Tagliabue E (2009) microRNA-205 regulates HER3 in human breast cancer. Cancer Res 69 (6): 2195–2200.
Irizarry RA, Bolstad BM, Collin F, Cope LM, Hobbs B, Speed TP (2003) Summaries of Affymetrix GeneChip probe level data. Nucleic Acids Res 31 (4): e15.
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60 (5): 277–300.
Jiang M, Zhang P, Hu G, Xiao Z, Xu F, Zhong T, Huang F, Kuang H, Zhang W (2013) Relative expression of miR-205-5p and miR-205-3p, and miR-21 in tissues and serum of non-small cell lung cancer patients. Mol Cell Biochem 383 (1-2): 67–75.
Jung H, Lee KP, Park SJ, Park JH, Jang YS, Choi SY, Jung JG, Jo K, Park DY, Yoon JH, Lim DS, Hong GR, Choi C, Park YK, Lee JW, Hong HJ, Kim S, Park YW (2008) TMPRSS4 promotes invasion, migration and metastasis of human tumor cells by facilitating an epithelial-mesenchymal transition. Oncogene 27 (18): 2635–2647.
Kebebew E, Peng M, Reiff E, Duh QY, Clark OH, McMillan A (2005) ECM1 and TMPRSS4 are diagnostic markers of malignant thyroid neoplasms and improve the accuracy of fine needle aspiration biopsy. Ann Surg 242 (3): 353–361, (discussion 361-3).
Kim S, Kang HY, Nam EH, Choi MS, Zhao XF, Hong CS, Lee JW, Lee JH, Park YK (2010) TMPRSS4 induces invasion and epithelial-mesenchymal transition through upregulation of integrin alpha5 and its signaling pathways. Carcinogenesis 31 (4): 597–606.
Kloosterman WP, Plasterk RH (2006) The diverse functions of microRNAs in animal development and disease. Dev Cell 11 (4): 441–450.
Larzabal L, Nguewa PA, Pio R, Blanco D, Sanchez B, Rodriguez MJ, Pajares MJ, Catena R, Montuenga LM, Calvo A (2011) Overexpression of TMPRSS4 in non-small cell lung cancer is associated with poor prognosis in patients with squamous histology. Br J Cancer 105 (10): 1608–1614.
Lebanony D, Benjamin H, Gilad S, Ezagouri M, Dov A, Ashkenazi K, Gefen N, Izraeli S, Rechavi G, Pass H, Nonaka D, Li J, Spector Y, Rosenfeld N, Chajut A, Cohen D, Aharonov R, Mansukhani M (2009) Diagnostic assay based on hsa-miR-205 expression distinguishes squamous from nonsquamous non-small-cell lung carcinoma. J Clin Oncol 27 (12): 2030–2037.
Lim LP, Lau NC, Garrett-Engele P, Grimson A, Schelter JM, Castle J, Bartel DP, Linsley PS, Johnson JM (2005) Microarray analysis shows that some microRNAs downregulate large numbers of target mRNAs. Nature 433 (7027): 769–773.
Lujambio A, Calin GA, Villanueva A, Ropero S, Sanchez-Cespedes M, Blanco D, Montuenga LM, Rossi S, Nicoloso MS, Faller WJ, Gallagher WM, Eccles SA, Croce CM, Esteller M (2008) A microRNA DNA methylation signature for human cancer metastasis. Proc Natl Acad Sci USA 105 (36): 13556–13561.
Majid S, Saini S, Dar AA, Hirata H, Shahryari V, Tanaka Y, Yamamura S, Ueno K, Zaman MS, Singh K, Chang I, Deng G, Dahiya R (2011) MicroRNA-205 inhibits Src-mediated oncogenic pathways in renal cancer. Cancer Res 71 (7): 2611–2621.
Markou A, Tsaroucha EG, Kaklamanis L, Fotinou M, Georgoulias V, Lianidou ES (2008) Prognostic value of mature microRNA-21 and microRNA-205 overexpression in non-small cell lung cancer by quantitative real-time RT-PCR. Clin Chem 54 (10): 1696–1704.
Maschler S, Wirl G, Spring H, Bredow DV, Sordat I, Beug H, Reichmann E (2005) Tumor cell invasiveness correlates with changes in integrin expression and localization. Oncogene 24 (12): 2032–2041.
Matsushima K, Isomoto H, Yamaguchi N, Inoue N, Machida H, Nakayama T, Hayashi T, Kunizaki M, Hidaka S, Nagayasu T, Nakashima M, Ujifuku K, Mitsutake N, Ohtsuru A, Yamashita S, Korpal M, Kang Y, Gregory PA, Goodall GJ, Kohno S, Nakao K (2011) MiRNA-205 modulates cellular invasion and migration via regulating zinc finger E-box binding homeobox 2 expression in esophageal squamous cell carcinoma cells. J Transl Med 9: 30.
Nam EH, Lee Y, Park YK, Lee JW, Kim S (2012) ZEB2 upregulates integrin alpha5 expression through cooperation with Sp1 to induce invasion during epithelial-mesenchymal transition of human cancer cells. Carcinogenesis 33 (3): 563–571.
Netzel-Arnett S, Hooper JD, Szabo R, Madison EL, Quigley JP, Bugge TH, Antalis TM (2003) Membrane anchored serine proteases: a rapidly expanding group of cell surface proteolytic enzymes with potential roles in cancer. Cancer Metastasis Rev 22 (2-3): 237–258.
Park SM, Gaur AB, Lengyel E, Peter ME (2008) The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev 22 (7): 894–907.
Ponz-Sarvise M, Nguewa PA, Pajares MJ, Agorreta J, Lozano MD, Redrado M, Pio R, Behrens C, Wistuba II, Garcia-Franco CE, Garcia-Foncillas J, Montuenga LM, Calvo A, Gil-Bazo I (2011) Inhibitor of differentiation-1 as a novel prognostic factor in NSCLC patients with adenocarcinoma histology and its potential contribution to therapy resistance. Clin Cancer Res 17 (12): 4155–4166.
Ramirez RD, Sheridan S, Girard L, Sato M, Kim Y, Pollack J, Peyton M, Zou Y, Kurie JM, Dimaio JM, Milchgrub S, Smith AL, Souza RF, Gilbey L, Zhang X, Gandia K, Vaughan MB, Wright WE, Gazdar AF, Shay JW, Minna JD (2004) Immortalization of human bronchial epithelial cells in the absence of viral oncoproteins. Cancer Res 64 (24): 9027–9034.
Roman J, Ritzenthaler JD, Roser-Page S, Sun X, Han S (2010) alpha5beta1-integrin expression is essential for tumor progression in experimental lung cancer. Am J Respir Cell Mol Biol 43 (6): 684–691.
Roy R, Yang J, Moses MA (2009) Matrix metalloproteinases as novel biomarkers and potential therapeutic targets in human cancer. J Clin Oncol 27 (31): 5287–5297.
Sawada K, Mitra AK, Radjabi AR, Bhaskar V, Kistner EO, Tretiakova M, Jagadeeswaran S, Montag A, Becker A, Kenny HA, Peter ME, Ramakrishnan V, Yamada SD, Lengyel E (2008) Loss of E-cadherin promotes ovarian cancer metastasis via alpha 5-integrin, which is a therapeutic target. Cancer Res 68 (7): 2329–2339.
Song H, Bu G (2009) MicroRNA-205 inhibits tumor cell migration through down-regulating the expression of the LDL receptor-related protein 1. Biochem Biophys Res Commun 388 (2): 400–405.
Szabo R, Bugge TH (2008) Type II transmembrane serine proteases in development and disease. Int J Biochem Cell Biol 40 (6–7): 1297–1316.
Tellez CS, Juri DE, Do K, Bernauer AM, Thomas CL, Damiani LA, Tessema M, Leng S, Belinsky SA (2011) EMT and stem cell-like properties associated with miR-205 and miR-200 epigenetic silencing are early manifestations during carcinogen-induced transformation of human lung epithelial cells. Cancer Res 71 (8): 3087–3097.
Valencia K, Ormazabal C, Zandueta C, Luis-Ravelo D, Anton I, Pajares MJ, Agorreta J, Montuenga LM, Martinez-Canarias S, Leitinger B, Lecanda F (2012) Inhibition of collagen receptor discoidin domain receptor-1 (DDR1) reduces cell survival, homing, and colonization in lung cancer bone metastasis. Clin Cancer Res 18 (4): 969–980.
Wallrapp C, Hahnel S, Muller-Pillasch F, Burghardt B, Iwamura T, Ruthenburger M, Lerch MM, Adler G, Gress TM (2000) A novel transmembrane serine protease (TMPRSS3) overexpressed in pancreatic cancer. Cancer Res 60 (10): 2602–2606.
Wu H, Mo YY (2009) Targeting miR-205 in breast cancer. Expert Opin Ther Targets 13 (12): 1439–1448.
Wu H, Zhu S, Mo YY (2009) Suppression of cell growth and invasion by miR-205 in breast cancer. Cell Res 19 (4): 439–448.
Yanaihara N, Caplen N, Bowman E, Seike M, Kumamoto K, Yi M, Stephens RM, Okamoto A, Yokota J, Tanaka T, Calin GA, Liu CG, Croce CM, Harris CC (2006) Unique microRNA molecular profiles in lung cancer diagnosis and prognosis. Cancer Cell 9 (3): 189–198.
Acknowledgements
We thank the Proteomics and Bioinformatics Unit at CIMA for performing the microarrays and for the analysis of the microarray data. This work has been funded by ‘UTE’ project CIMA, by grants (RD12/0036/0040) from Red Temática de Investigación Cooperativa en Cáncer (RTICC and PI 10/00166), Instituto de Salud Carlos III (ISCIII), Spanish Ministry of Economy and Competitiveness & European Regional Development Fund (ERDF) ‘Una manera de hacer Europa’, Gobierno de Navarra, and PIUNA (ref 12028402). LL was supported by a Gobierno Vasco fellowship and ALA by Asociación de Amigos (Universidad de Navarra) fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Larzabal, L., de Aberasturi, A., Redrado, M. et al. TMPRSS4 regulates levels of integrin α5 in NSCLC through miR-205 activity to promote metastasis. Br J Cancer 110, 764–774 (2014). https://doi.org/10.1038/bjc.2013.761
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.761
Keywords
This article is cited by
-
TMPRSS4 is a novel biomarker and correlated with immune infiltration in thyroid carcinoma
BMC Endocrine Disorders (2022)
-
Identification and validation of a novel prognostic model of inflammation-related gene signature of lung adenocarcinoma
Scientific Reports (2022)
-
Inhibition Sequence of miR-205 Hinders the Cell Proliferation and Migration of Lung Cancer Cells by Regulating PETN-Mediated PI3K/AKT Signal Pathway
Molecular Biotechnology (2021)
-
LncRNA EWSAT1 Regulates the Tumorigenesis of NSCLC as a ceRNA by Modulating miR-330-5p/ITGA5 Axis
Biochemical Genetics (2021)
-
Transcriptomic response of primary human airway epithelial cells to flavoring chemicals in electronic cigarettes
Scientific Reports (2019)