Abstract
Background:
Nomograms are predictive tools that are widely used for estimating cancer prognosis. The aim of this study was to develop a nomogram for the prediction of overall survival (OS) in patients diagnosed with cervical cancer.
Methods:
Cervical cancer databases of two large institutions were analysed. Overall survival was defined as the clinical endpoint and OS probabilities were estimated using the Kaplan–Meier method. Based on the results of survival analyses and previous studies, relevant covariates were identified, a nomogram was constructed and validated using bootstrap cross-validation. Discrimination of the nomogram was quantified with the concordance probability.
Results:
In total, 528 consecutive patients with invasive cervical cancer, who had all nomogram variables available, were identified. Mean 5-year OS rates for patients with International Federation of Gynecologists and Obstetricians (FIGO) stage IA, IB, II, III, and IV were 99.0%, 88.6%, 65.8%, 58.7%, and 41.5%, respectively. Seventy-six cancer-related deaths were observed during the follow-up period. FIGO stage, tumour size, age, histologic subtype, lymph node ratio, and parametrial involvement were selected as nomogram covariates. The prognostic performance of the model exceeded that of FIGO stage alone and the model’s estimated optimism-corrected concordance probability was 0.723, indicating accurate prediction of OS. We present the prediction model as nomogram and provide a web-based risk calculator (http://www.ccc.ac.at/gcu).
Conclusion:
Based on six easily available parameters, a novel statistical model to predict OS of patients diagnosed with cervical cancer was constructed and validated. The model was implemented in a nomogram and provides accurate prediction of individual patients’ prognosis useful for patient counselling and deciding on follow-up strategies.
Similar content being viewed by others
Main
The annual incidence of invasive cervical cancer is 6.6/100 000 women in Austria. Within the year 2009, 394 new cases of cervical cancer were diagnosed (Statistik Austria, 2011). Clinical stage based upon the International Federation of Gynecologists and Obstetricians (FIGO) system reflects the strongest prognostic parameter in patients with cervical cancer (Benedet et al, 2000). The FIGO staging system is based upon clinical examination and the system’s limitations are well appreciated (Hricak et al, 2005). A number of other clinico-pathological parameters were shown to have additional prognostic value in predicting patients’ prognosis (Lagasse et al, 1980). Besides FIGO stage, the most notable prognostic factors are lymph node status and the number of positive lymph nodes, tumour size, parametrial involvement, histologic type, and patients’ age (Delgado et al, 1990; Inoue and Morita, 1990; Takeda et al, 2002; Quinn et al, 2006). The prognostic relevance of other additional parameters such as lymph vascular space invasion (LVSI), histologic grade, and depth of cervical stromal invasion is controversial (Creasman and Kohler, 2004; Kastritis et al, 2007).
Prognostic nomograms have been recently introduced for numerous malignancies, including gynaecologic cancers, to obtain reliable prognostic information tailored to each individual patient (Chi et al, 2008; Abu-Rustum et al, 2010). Several nomograms were shown to compare favourably to traditional staging systems and their use has been suggested in addition to or even as an alternative to disease stage and other established prognosticators (Iasonos et al, 2008; Abu-Rustum et al, 2010). For patients with cervical cancer, a nomogram to predict overall survival (OS) through stages I–IV has not been published so far. The aim of this study was to develop and validate a nomogram for individual prediction of OS in patients diagnosed with invasive cervical cancer.
Patients and Methods
Patients
All consecutive patients diagnosed with cervical cancer at the University Hospitals Vienna and Innsbruck, Austria between 1996 and 2009 were eligible for this study. Clinical data were extracted from the institutions’ prospectively maintained, electronic databases. Institutional review board approval was obtained before the study (IRB approval numbers: 246-2009 (Ethics Committee Medical University of Vienna) and UN4144 (Ethics Committee Medical University of Innsbruck)).
Clinical management
Patients were treated and followed according to the international guidelines (Committee on Practice Bulletins-Gynecology, 2002; Greer et al, 2008). Briefly, patients diagnosed at stage IA1 disease were treated with conization or simple hysterectomy. If final pathology revealed the presence of LVSI, systematic pelvic and/or paraaortic lymphadenectomy was performed. Patients with stage IA2 were treated either by conization or simple hysterectomy plus systematic pelvic and/or paraaortic lymphadenectomy. Early stage disease FIGO IB1-IIA was managed by radical hysterectomy or trachelectomy plus systematic pelvic and/or paraaortic lymphadenectomy. Patients with positive lymph nodes, parametrial involvement, and positive or close surgical margins were treated with adjuvant, postoperative radiotherapy – with or without concurrent chemotherapy. Cervical cancer FIGO IIB-IV was treated with primary radio-chemotherapy. In these patients, pelvic and/or paraaortic lymphadenectomy was performed before radio-chemotherapy to allow individualised planning of the radiation field. Extended field radiation was administered to patients with positive lymph nodes in the common iliac region (when paraaortic lymphadenectomy was not performed) or to patients with positive paraaortic lymph nodes (Pötter et al, 2011).
Statistical analysis
Values are given as mean (standard deviation (s.d.)) when normally distributed or as median (interquartile range (IQR)) at the presence of skewed distribution. P-values of <0.05 were considered statistically significant. We used the statistical software R 2.12.2 for Windows (R Foundation for Statistical Computing, Vienna, Austria).
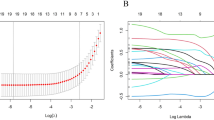
Overall survival, defined as the time from diagnosis to date of cancer-related death or date of last follow-up for patients who were alive and censored, was defined as the clinical endpoint. Overall survival probabilities were estimated using the Kaplan–Meier method. The following predictors were selected for model development based on previous multivariable analyses (Polterauer et al, 2011): age (continuous variable), FIGO stage (IV vs III vs II vs IB), the presence of positive lymph nodes (positive vs negative), and at the presence of positive lymph nodes lymph node ratio (LNR; continuous variable), parametrial involvement (positive vs negative), and tumour size (⩽2 vs >2 cm). Lymph node ratio was defined as the ratio of positive and totally removed lymph nodes, as previously described (Polterauer et al, 2010). FIGO stages IA were excluded from predictive modelling, as only one event was observed in this group. The model was constructed by estimating a Cox regression model, maximising a likelihood function with a ridge (sum of squared regression coefficients) penalty term to prevent against over-fitting potentially caused by the small number of events in our study (76 events). This type of analysis can deal with data sets in which the number of events per variable is much less than 10, as it prevents overfitting by shrinking the coefficients compared with those by standard Cox regression (Ambler et al, 2012). The tuning parameter that controls the amount of shrinkage of regression coefficients by the ridge penalty was optimised by maximising the average of the 10-fold cross-validated partial likelihood over 10 different random partitions of the data into 10-folds (Ambler et al, 2012). We decided to include all preselected variables irrespective of significance as nomogram parameters as even non-significant variables must be assumed to have a non-zero effect on survival. Correlation analysis between clinical variables was performed using Spearman and Kendall tau-b rank correlation coefficients. Interactions of any predictors with FIGO stage were evaluated by comparing the cross-validated partial likelihood with and without these interactions. Likewise, we checked for non-linear effects of age or LNR by employing the technique of fractional polynomials and compared the cross-validated partial likelihood with and without nonlinear modelling (Royston and Altman, 1994). We used the R package glmnet (R Foundation for Statistical Computing) for estimating the model coefficients (Simon et al, 2011).
Model validation
To determine calibration and discrimination of the model corrected for optimism, we generated 1000 bootstrap samples, which were used as training sets in a bootstrap validation procedure. Specifically, a model was built on each of the 1000 training sets following the same process as described above. The 1000 models were then evaluated on the original data (test set) without modification, estimating 5-year survival probabilities for each patient. For each of the validation models, we constructed a time-dependent receiver operating characteristic (ROC) curve using the survival ROC package of R (Heagerty et al, 2000). As a measure of discrimination, we computed the median and IQR over the optimism-corrected time-dependent areas under the ROC curves (the c-indices) obtained in each of the models and provide a summary c-index as described previously (Steyerberg, 2009 and Uno et al, 2011). The calibration of the prediction model was assessed by stratifying the patients, by their risk score, into four quartiles, and evaluating the observed 3- and 5-year survival probability in each quartile by Kaplan–Meier analysis. The mean predicted 3- and 5-year survival probabilities, averaged over the 1000 models, were compared with the averaged observed survival probabilities in calibration plots. If the model is well calibrated, this plot should demonstrate agreement of the predicted and observed survival probabilities.
Results
Patients
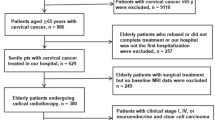
A total of 692 consecutive patients with invasive cervical cancer, who were treated at the two institutions between January 1999 and December 2009, were identified. Of these, 528 patients (Department of Gynecology, Comprehensive Cancer Center Vienna, Medical University of Vienna, Vienna, Austria, n=335 and Innsbruck Medical University, Tirol, Austria, n=193) had all nomogram variables available and were included into the analysis. Patients’ characteristics and treatment modalities are shown in Tables 1 and 2, respectively.
Survival analyses
Median follow-up time was 45.7 months. Patients’ status at last follow-up and recurrence status are shown in Table 1. Five-year OS rates (standard error) for patients with FIGO stage IA, IB, II, III, and IV were 99.0% (1.0), 88.6% (3.0), 65.8% (5.2), 58.7% (11.0), and 41.5% (14.7), respectively. Figure 1 shows cervical cancer-specific survival with number of patients at risk for cancer-related death for each of the follow-up time points.
Construction and validation of the prediction model
The FIGO stage, tumour size, age, histologic subtype, LNR, and parametrial involvement were predefined as predictors. The FIGO stage was strongly correlated with tumour size (tau=0.82, P<0.001), parametrial involvement (tau=0.71, P<0.001), LNR (rho=0.42, P<0.001), and age (rho=0.33, P<0.001). Univariate hazard ratios with 95% confidence intervals estimated from univariate Cox regressions are shown in Table 3. From the multivariable penalised Cox regression model, we computed nomogram points for each predictor by dividing the shrinked coefficients by the largest shrinked coefficient obtained in the analysis (that of LNR), and multiplying by 100 (Figure 2). Including interactions of FIGO stage with the other predictors did not improve the cross-validated partial likelihood, and neither did the consideration of non-linear effects for LNR or age (data not shown).
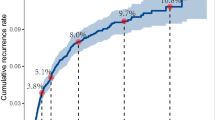
The prediction model was internally validated using bootstrap resampling, assessing its optimism-corrected discrimination and calibration. Across the 1000 bootstrap repetitions, the median optimism-corrected summary c-index for predicting survival was 0.723 (25th and 75th percentiles, 0.701 and 0.743, respectively). Figure 3 shows a plot of the time-dependent optimism-corrected c-index, indicating constant and adequate discriminative ability of our prediction model for prediction horizons between 1 and 5 years. The bootstrap-predicted and the actual OS probabilities at 3 and 5 years are shown in the calibration plots (Figures 4A and B, respectively). The calibration plots describe how far predictions are from actual outcomes and how the prediction model fits the data. The performance of the model appears to be very accurate, within the actual outcomes.
Cervical cancer OS nomogram calibration plots: (A) 3-year and (B) 5-year nomogram calibration curve. Nomogram-predicted OS rates are plotted on the x-axis, actual OS are plotted on the y-axis. The dashed line represents the ideal fit where the nomogram-predicted probability matches the observed probability from Kaplan–Meier estimates.
It is important to note that all six covariates must be available to use the nomogram and predict individual patients’ OS. For example, a 45-year-old (7.2 points) with stage IB (0 points), tumour size ⩽2 cm (0 points), squamous cell carcinoma (0 points) with negative lymph nodes (0 points) has a total of 7.2 points, which corresponds to the 3- and 5-year OS probabilities of 95% and 91.8%, respectively. On the other hand, a 45-year-old (7.2 points), with stage IIB (20 points), tumour size ⩽2 cm (0 points), 3 positive out of 15 removed nodes (LNR 0.2 corresponding to 50 points), squamous cell carcinoma (0 points), and parametrial involvement (24 points) has a total of 101.2 points, which corresponds to the 3- and 5-year OS probabilities of 81.1% and 70.5%, respectively.
Figure 5 provides predicted 5-year OS probability sub-grouped by 2009 FIGO stage. We show that, although FIGO stage is an important predictor of 5-year survival probability, the other predictors used in our model add further information useful to discriminate patients with poor or favourable prognosis. Overall, our prediction model combines prognostic factors in a multivariate setting, and thus it is able to discriminate high-, moderate-, and low-risk patients in a detailed way through individualised predictions.
Discussion
Accurate prediction of cancer control after definitive treatment for cervical cancer is important for patient counselling, follow-up, and treatment planning. We constructed a novel nomogram based on a model to predict 3- and 5-year OS for patients with invasive cervical cancer after surgical staging. The nomogram can be used to predict patients’ prognosis individually and more accurate than FIGO stage alone and is based on the following six easily available parameters: FIGO stage, tumour size, histologic type, LNR, age, and parametrial involvement. The model was derived from a European cohort with the entirety of the age spectrum.
FIGO stage is the most important prognostic parameter in patients diagnosed with cervical cancer. Many, but not all, of the known prognostic factors are captured by the FIGO staging system. The FIGO staging system is largely based upon physical examination and a limited number of diagnostic studies (Pecorelli et al, 2009). The limitations of FIGO clinical staging are well appreciated and under-staging occurs (Hricak et al, 2005; Quinn et al, 2006). Tumour size is an established prognostic parameter that is independent of stage and was originally reflected in FIGO stages IA-IB2. During the 2009 FIGO staging system changes tumour size was added as parameter for stage IIA to distinguish between tumour diameters smaller (IIA1) and larger (IIA2) than 4 cm tumours due to its considerable prognostic value (Delgado et al, 1990; Pecorelli et al, 2009). The effect of tumour histology on outcome for women with cervical cancer has been actively debated. Recent studies have shown that adenocarcinomas are more aggressive and are associated with decreased survival for both early and advanced-stage carcinomas (Galic et al, 2012).
Lymph node ratio is a parameter incorporating not only information on the number of positive nodes but also the number of removed nodes. Lymph node ratio is a useful prognostic parameter for patients with cervical cancer and allows stratification of patients into distinctive outcome groups (Polterauer et al, 2010). It is important to highlight that assigning LNR requires surgical staging with node dissection. The authors are aware that the therapeutic value of pretreatment surgical lymph node staging for patients with advanced stage cervical cancer is still controversial (Brockbank et al, 2011). At our institution extended-field radiotherapy is recommended when paraaortic nodal disease is proven and we observed excellent pelvic control in these high-risk patients using this concept (Pötter et al, 2011). For patients with stage IA1 disease lymph node, dissection was only performed when LVSI was present. As previous studies have shown that the risk for nodal involvement is less than 1% for patients with stage IA1 disease and without LVSI, we assumed negative nodal status and this group of patients was allocated a LNR of 0.0.
Recent studies suggested that younger age is an unfavourable prognostic factor, especially in more advanced stages (Chen et al, 1999). Survival analysis revealed that younger patients showed impaired survival in cohort and therefore age was included into our model. Parametrial involvement significantly influences outcome of patients with cervical cancer but is not reflected in FIGO stages III-IV (Takeda et al, 2002). In the Gynecologic Oncology Group (GOG), 49 study patients with apparent stage I disease with and without parametrial involvement were shown to have 70% and 85% 3-years disease-free intervals, respectively (Delgado et al, 1990). Patients found to have parametrial involvement will usually receive primary or adjuvant radiation therapy after surgery (Committee on Practice Bulletins-Gynaecology, 2002).
A nomogram is a graphic prediction tool that incorporates clinical risk factors already included in established staging systems, as well as other additional, clinical, and pathologic factors known to have an impact on outcome. A distinct advantage of a nomogram is that all the critical variables that determine outcome can be graphically displayed (Iasonos et al, 2008). Prognostic nomograms attempt to combine important clinical factors to quantify the risk as precisely as possible to accurately predict clinical outcome. Clinical nomograms have been developed as predictive tools for outcomes in gynaecologic malignancies such as endometrial and ovarian cancer (Chi et al, 2008; Abu-Rustum et al, 2010). For the estimation of outcome of patients with cervical cancer, few nomograms have been published so far (Kim et al, 2010; Tseng et al, 2010). This nomogram is the first to predict OS through stages I–IV that was constructed based on data of a mainly Caucasian patient cohort.
Despite having achieved prognostic accuracy, our study is not devoid of limitations. The multi-institutional nature of our data set may be interpreted as a limitation, given that it groups the contribution of multiple surgeons and pathologists and relies on different surgical approaches, in addition to other differences that might distinguish the two contributing centres. However, this limitation could also be seen as strength, as it makes our conclusions more general and increases the available sample size, which is important given the low event rate. Despite combining data from two institutions, we observed a limited number of events (i.e., cancer-related deaths). To take this into account, the model coefficients were computed using the recently developed ‘ridge’ method. This approach was originally designed to deal with situations where the number of predictors exceeds the number of events by large (‘P>>n’) such as in genomic applications, and was recently found to be superior to other methods also for prediction in ‘classical’ (‘P<n’) settings, where less than 10 events per variable are available (Ambler et al, 2012). In ridge regression, the amount of penalisation is driven by predictive performance in cross-validation (cross-validated partial likelihood). This ‘automatism’ guards against over-fitting a model. However, shortage of data, caused by too many variables compared with the number of events, may lead to higher penalisation, and reduce ability of a model to predict the outcome in the extremes. Therefore, we created calibration plots based on internal cross-validation by bootstrap resampling, which showed an almost perfect agreement of observed and predicted event rates. Nevertheless, external validity of our model is a crucial prerequisite to clinical applicability, and can only be assessed by confirming results in a reasonably large independent validation cohort with an adequate follow-up period. Another potential limitation of our model as typical for nomograms is that construction is based on retrospective data. Therefore, our study might be limited by biases such as lack of random assignment, patient selection, and incomplete data acquisition. Nomogram variables were missing in a significant number (n=164) of patients of our cohort. Mostly information on parametrial involvement and exact tumour size was incompletely documented in the cases that were excluded from analysis, especially in patients with advanced stage cervical cancer.
In summary, we present the first model to predict 3- and 5-year survival for patients with cervical cancer after surgical staging that is applicable through stages I–IV. The model was developed in a relatively large European, mainly Caucasian, cohort and can be applied for prediction by means of the presented nomogram or, more conveniently, by an online prediction tool (available at http://www.ccc.ac.at/gcu).
Change history
18 August 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abu-Rustum NR, Zhou Q, Gomez JD, Alektiar KM, Hensley ML, Soslow RA, Levine DA, Chi DS, Barakat RR, Iasonos A (2010) A nomogram for predicting overall survival of women with endometrial cancer following primary therapy: toward improving individualized cancer care. Gynecol Oncol 116: 399–403
Ambler G, Seaman S, Omar R (2012) An evaluation of penalised survival methods for developing prognostic models with rare events. Stat Med 31: 1150–1161
Benedet JL, Bender H, Jones H, Ngan HY, Pecorelli S (2000) FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet 70: 209
Brockbank E, Kokka F, Bryant A, Pomel C, Reynolds K (2011) Pre-treatment surgical para-aortic lymph node assessment in locally advanced cervical cancer. Cochrane Database Syst Rev 4: CD008217
Chen RJ, Lin YH, Chen CA, Huang SC, Chow SN, Hsieh CY (1999) Influence of histologic type and age on survival rates for invasive cervical carcinoma in Taiwan. Gynecol Oncol 73: 184–190
Chi DS, Palayekar MJ, Sonoda Y, Abu-Rustum NR, Awtrey CS, Huh J, Eisenhauer EL, Barakat RR, Kattan MW (2008) Nomogram for survival after primary surgery for bulky stage IIIC ovarian carcinoma. Gynecol Oncol 108: 191–194
Committee on Practice Bulletins-Gynecology. ACOG practice bulletin (2002) Diagnosis and treatment of cervical carcinomas, number 35, May 2002. Obstet Gynecol 99: 855
Creasman WT, Kohler MF (2004) Is lymph vascular space involvement an independent prognostic factor in early cervical cancer? Gynecol Oncol 92: 525
Delgado G, Bundy B, Zaino R, Sevin BU, Creasman WT, Major F (1990) Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a Gynecologic Oncology Group study. Gynecol Oncol 38: 352
Galic V, Herzog TJ, Lewin SN, Neugut AI, Burke WM, Lu YS, Hershman DL, Wright JD (2012) Prognostic significance of adenocarcinoma histology in women with cervical cancer. Gynecol Oncol 125 (2): 287–291
Greer BE, Koh WJ, Abu-Rustum N, Bookman MA, Bristow RE, Campos S, Cho KR, Copeland L, Eifel P, Huh WK, Jaggernauth W, Kapp DS, Kavanagh J, Lipscomb GH, Lurain JR, Morgan M, Morgan RJ, Powell CB, Remmenga SW, Reynolds RK, Secord AA, Small W, Teng N, National Comprehensive Cancer Network Cervical cancer (2008) J Natl Compr Canc Netw 6: 14–36
Heagerty PJ, Lumley T, Pepe MS (2000) Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 56: 337–344
Hricak H, Gatsonis C, Chi DS, Amendola MA, Brandt K, Schwartz LH, Koelliker S, Siegelman ES, Brown JJ, McGhee RB, Iyer R, Vitellas KM, Snyder B, Long HJ, Fiorica JV, Mitchell DG, American College of Radiology Imaging Network 6651; Gynecologic Oncology Group 183 (2005) Role of imaging in pretreatment evaluation of early invasive cervical cancer: results of the intergroup study American College of Radiology Imaging Network 6651-Gynecologic Oncology Group 183. J Clin Oncol 23: 9329–9337
Iasonos A, Schrag D, Raj GV, Panageas KS (2008) How to build and interpret a nomogram for cancer prognosis. J Clin Oncol 26: 1364–1370
Inoue T, Morita K (1990) The prognostic significance of number of positive nodes in cervical carcinoma stages IB, IIA, and IIB. Cancer 65: 1923
Kastritis E, Bamias A, Bozas G, Koutsoukou V, Voulgaris Z, Vlahos G, Rodolakis A, Gika D, Papadimitriou C, Dimopoulos MA (2007) The impact of age in the outcome of patients with advanced or recurrent cervical cancer after platinum-based chemotherapy. Gynecol Oncol 104: 372–376
Kim MK, Jo H, Kong HJ, Kim HC, Kim JW, Kim YM, Song YS, Kang SB, Mok JE, Lee HP (2010) Postoperative nomogram predicting risk of recurrence after radical hysterectomy for early-stage cervical cancer. Int J Gynecol Cancer 20: 1581–1586
Lagasse LD, Creasman WT, Shingleton HM, Ford JH, Blessing JA (1980) Results and complications of operative staging in cervical cancer: experience of the Gynecologic Oncology Group. Gynecol Oncol 9: 90
Pecorelli S, Zigliani L, Odicino F (2009) Revised FIGO staging for carcinoma of the cervix. Int J Gynaecol Obstet 105: 107–108
Pötter R, Georg P, Dimopoulos JC, Grimm M, Berger D, Nesvacil N, Georg D, Schmid MP, Reinthaller A, Sturdza A, Kirisits C (2011) Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol 100: 116–123
Polterauer S, Hefler L, Seebacher V, Rahhal J, Tempfer C, Horvat R, Reinthaller A, Grimm C (2010) The impact of lymph node density on survival of cervical cancer patients. Br J Cancer 103: 613–626
Quinn MA, Benedet JL, Odicino F, Maisonneuve P, Beller U, Creasman WT, Heintz AP, Ngan HY, Pecorelli S (2006) Carcinoma of the cervix uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet 95: 103
Royston P, Altman DG (1994) Regression using fractional polynomials of continuous covariates: parsimonious parametric modelling. Applied Statistics 43: 429–467
Simon N, Friedman J, Hastie T, Tibshirani R (2011) Regularization Paths for Cox’s Proportional Hazards Model via Coordinate Descent. J Stat Software 39: 1–13
Statistik Austria (2011) Krebsinzidenz und Krebsmortalität in Österreich 2010. (ISBN 978-3-902703-42-2)
Steyerberg EW (2009) Clinical Prediction Models. A Practical Approach to Development, Validation, and Updating. Series title: Statistics for Biology and Health, p.95f. Springer: New York, ISBN: 978-0-387-77243-1 doi:10.1007/978-0-387-77244-8
Takeda N, Sakuragi N, Takeda M, Okamoto K, Kuwabara M, Negishi H, Oikawa M, Yamamoto R, Yamada H, Fujimoto S (2002) Multivariate analysis of histopathologic prognostic factors for invasive cervical cancer treated with radical hysterectomy and systematic retroperitoneal lymphadenectomy. Acta Obstet Gynecol Scand 81: 1144–1151
Tseng JY, Yen MS, Twu NF, Lai CR, Horng HC, Tseng CC, Chao KC, Juang CM (2010) Prognostic nomogram for overall survival in stage IIB-IVA cervical cancer patients treated with concurrent chemoradiotherapy. Am J Obstet Gynecol 202 (2): 174.e1–e7
Uno H, Cai T, Pencina MJ, D’Agostino RB, Wei LJ (2011) On the C-statistics for evaluating overall adequacy of risk prediction procedures with censored survival data. Stat Med 30: 1105–1117
Acknowledgements
We thank Andrea Wolf and Gustav Nowotny for prospectively maintaining the institutions’ databases, both supported by the Ludwig Boltzman Institute for Oncology (Head: Robert Zeillinger PhD). The funding source had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in decision to publish the article. S Polterauer had full access to all the data in the study and had final responsibility to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Polterauer, S., Grimm, C., Hofstetter, G. et al. Nomogram prediction for overall survival of patients diagnosed with cervical cancer. Br J Cancer 107, 918–924 (2012). https://doi.org/10.1038/bjc.2012.340
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.340
Keywords
This article is cited by
-
A prognostic model using FIGO 2018 staging and MRI-derived tumor volume to predict long-term outcomes in patients with uterine cervical squamous cell carcinoma who received definitive radiotherapy
World Journal of Surgical Oncology (2023)
-
Glycolysis-Metabolism-Related Prognostic Signature for Ewing Sarcoma Patients
Molecular Biotechnology (2023)
-
Development and validation of nomograms to recurrence and survival in patients with early-stage cervical adenocarcinoma
Journal of Cancer Research and Clinical Oncology (2023)
-
Internal Validation of a Predictive Model for Overall Survival in Patients with FIGO stages I–IV Cervical Cancer
Indian Journal of Gynecologic Oncology (2023)
-
Development of a prognostic metabolic signature in stomach adenocarcinoma
Clinical and Translational Oncology (2022)