Key Points
-
Cone beam computed tomography is not only being used in the hospital setting but also in primary care for dental patients.
-
Reviews the development of cone beam computed tomography in dentistry.
-
Highlights the advantages of this imaging modality in respect of diagnostic yield and reduced radiation dose.
Abstract
Cone beam computed tomography (CBCT) is a rapidly emerging imaging modality in dentistry that offers the advantages of high diagnostic yield with short scanning times and a radiation dose significantly lower than conventional CT. Clinical applications of CBCT are numerous and they are being used both within the hospital and the primary care setting. The need for complete interpretation of CBCT images is essential. This report presents two patients for whom CBCT was carried out for orthodontic related purposes and incidental findings of cervical vertebrae clefts diagnosed. CBCT wherever they are undertaken should be reported by someone who has undergone adequate training in their interpretation particularly when machines using a large field of view are employed.
Similar content being viewed by others
Introduction
Conventional computed tomography (CT) was originally developed by British engineer Sir Geoffrey Hounsfield1 who was later awarded the Nobel Peace Prize and honoured with a Knighthood for his contributions to medicine and science. In conventional CT, an X-ray source and solid-state detector are mounted on a rotating gantry. Data are acquired using a narrow fan-shaped X-ray beam. The patient is imaged slice-by-slice, usually in the axial plane, and interpretation of the images is achieved by stacking the slices to obtain multiple two-dimensional representations. The data acquired in one scan can subsequently be manipulated to provide multiplanar and 3D reconstructions. Although providing excellent image resolution, the limiting factors for their use in dento-maxillofacial radiology are the relatively high radiation dose to the patient,2 its relative high cost and limited portability.
Cone Beam Computed Tomography (CBCT) evolved from conventional CT in the 1990s and uses a beam which radiates from the X-ray source in a cone shape, thus encompassing a large volume with a single rotation about the patient. Instead of having to stack multiple image slices as in conventional CT, CBCT allows a single rotation of the radiation source to capture an entire region of interest.3 The images are then reconstructed using algorithms to produce three-dimensional images at high resolution. The CBCT volumetric data set comprises a three-dimensional block of cuboid structures known as voxels, each representing a specific degree of X-ray absorption. The size of the voxels determines the resolution of the image. In conventional CT the voxels are anisotropic or rectangular in shape. All CBCT units are isotropic, ie equal in all three dimensions, which can produce superb sub-millimetre resolution.4 In addition, the radiation dose of CBCT is approximately four times less than conventional CT scanning.5 Other advantages include that the patient can sit upright or stand during CBCT, as opposed to supine in conventional CT, and therefore a more representative examination of the soft tissue outline is obtained.
There are already a number of clinical applications of CBCT that have been reported in the literature including the precise location of ectopic canines,6 the assessment of alveolar bone heights and volume for implant placement,7 the assessment of bone graft quality following alveolar grafting in cleft lip and palate,8 airway analysis,9 and temporomandibular joint morphology.10 More recently, CBCT has been advocated for use in dental practice for endodontic applications.11
Although the high diagnostic yield and additional information provided by CBCT can offer an accurate diagnosis, more incidental findings are possible. A recent study found that overall rate of incidental findings in the maxillofacial area with three-dimensional CBCT was 24.6%.12
Two case reports are presented of patients who both underwent CBCT of the maxilla to aid dental diagnosis. Subsequent radiological reporting revealed rare anomalies of the cervical vertebrae. The implications of the findings are discussed and the importance of access to formal interpretation of CBCT for dental clinicians is highlighted.
Case 1
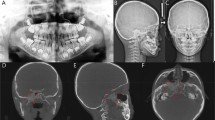
An 11-year-old female was referred to the Orthodontic Department by a specialist orthodontic practitioner regarding the management of an unerupted upper right first premolar. The practitioner had also noticed a bony anomaly in the right maxilla surrounding the tooth on a plain film radiograph. Clinical examination revealed the patient to have a significant Class II division 1 incisor relationship on a Skeletal 2 base in the late mixed dentition. The upper right first deciduous molar was retained and radiographic examination revealed an unerupted upper right permanent first premolar associated with a dense radiopaque bony lesion in the right maxilla (Fig. 1). The floor of the antrum was displaced superiorly by the lesion. The root morphology of the unerupted upper right first premolar was not well demonstrated by the plain film radiograph. In order to assess the lesion and its effect on the adjacent structures, a CBCT of the maxilla was carried out. This showed a radiopaque mass in the right maxilla extending from the tuberosity to the upper right permanent canine and superiorly to involve the base of the antrum. There was mild buccal and palatal expansion of the alveolus. The upper right first premolar and the unerupted upper right third molar were both involved in the lesion (Fig. 2). Overall the bony changes were consistent with fibrous dysplasia. Orthodontic treatment plan included the removal of the deciduous right first molar and the permanent first premolar along with a bone biopsy to confirm the diagnosis. An additional finding on the CBCT was a cleft in the posterior arch of the atlas (Figs 3 and 4).
Case 2
A 10-year-old boy was referred by his general dental practitioner (GDP) regarding failure of eruption of the upper left central incisor. There was a previous history of trauma to the upper left deciduous incisors which were removed under general anaesthesia when the patient was aged two years. Plain film radiographic examination revealed the upper left central incisor to be unerupted and dilacerated (Fig. 5). A CBCT of the maxilla was carried out to assess prognosis of the unerupted tooth. This showed that the tooth was markedly dilacerated and that enamel was present along half of its palatal 'root surface' (Fig. 6). In view of the position and morphology of the central incisor arrangements were made to remove the tooth and the GDP was asked to provide the patient with a partial denture. In addition to the dental findings however, the CBCT also showed a cleft in the anterior arch of the atlas (Figs 7 and 8).
Discussion
The first cervical vertebrae (C1) or atlas can be anatomically divided into three parts – the anterior arch, the lateral masses and the posterior arch. The atlas is formed from three primary ossification centres. Of these, one ossification centre appears in each lateral mass at the seventh week of gestation, and extends dorsally. At birth, these portions of bone are separated from one another by a narrow cartilaginous cleft. Between the third and fourth years they unite either directly or through the medium of a separate centre developed in the cartilage and signify completion of ossification.13
At birth, the anterior arch consists of cartilage. A separate ossification centre appears at the end of the first year after birth to join the lateral masses. Occasionally there is no separate centre, the anterior arch being formed by the forward extension and ultimate junction of the two lateral masses. Ossification is usually complete by the age of ten.13
Anomalies of the cervical vertebrae include clefts and aplasias and although rare, have been reported in the literature as early as 1941.14 Clefts present where there have been defects in the ossification centres of the vertebrae. Median clefts of the posterior arch are the most common and have been found in approximately 4% of adults, while anterior arch clefts are much rarer and found in 0.1% of the population, and can often be accompanied by posterior clefts.15 Cervical vertebrae anomalies can occur more frequently in individuals with cleft lip, cleft palate or both16 and have also been reported to occur with conditions such as thalassaemia minor.17 These vertebral anomalies may be discovered as incidental findings, or they may have a pattern of presentation varying from transient neck pain to different degrees of cord compression including myelopathy.18,19 No particular type of arch defect seems more prone to develop symptoms than others.18
An important aspect relating to clefts of the atlas is that they are known to simulate fractures.19,20,21 Fractures however show irregular edges with associated soft-tissue swelling – there may also be a history of trauma. Congenital clefts are smooth with an intact cortical wall22 as illustrated in both of our cases.
The advantages of CBCT in diagnostic yield and reduced radiation exposure have been well documented3 and outlined using two case reports in this review. Here, CBCT was used to supplement plain film radiographs to enable an accurate diagnosis and formulate an appropriate orthodontic treatment plan. The incidental findings of cervical vertebral clefts arose from full radiological reporting of the data set and although rare in presentation, did not result in any subsequent intervention. However, this may not always be the situation as other patients diagnosed with dentally related problems have had potentially life-threatening conditions diagnosed following conventional CT imaging.23
Although not explicitly stated in the Ionising Radiation (Medical Exposure) Regulations,24 reporting of radiographs is regarded as forming part of the 'operator role'. It follows then that anyone reporting CBCT scans should be adequately trained to carry out this task. With large field of view CBCT scanners, areas outside of the jaws including the inner ear, cervical spine and paranasal sinuses are well demonstrated. These areas are challenging to interpret and as such, general and maxillofacial radiologists will be taught to interpret these regions as part of their specialist training. Although when CBCT scanners are installed training is given regarding their practical use, no training is given in their interpretation. Perhaps specific training courses could be provided by the manufacturers. As an alternative, arrangements could be made between the dental practitioner and the local radiologists to allow the radiologist to report the scans. Web-based instruction for clinicians by radiologists in the interpretation of anatomy of images acquired with CBCT could be another option.25
As technological advances are made within the field of dento-maxillofacial imaging, the use of CBCT provides an opportunity for dental practitioners to access three-dimensional radiographic assessment for their patients. However, robust procedures must be in place to ensure that the whole of the imaging volume is examined and reported upon.
References
Hounsfield G . Computerized transverse axial scanning (tomography). 1. Description of the system. Br J Radiol 1973; 46: 1016–1022.
Pendlebury M E, Horner K, Eaton K A (eds). Selection criteria for dental radiography. London: Faculty of General Dental Practitioners (UK), Royal College of Surgeons of England, 2004.
Palomo J M, Kau C H, Palomo L B, Hans M G . Three-dimensional cone beam computerized tomography in dentistry. Dent Today 2005; 25: 130.
Scarfe W C, Farman A G, Sukovic P . Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc 2006; 72: 75–80.
Schulze D, Heiland M, Thurmann H, Adam G . Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol 2004; 33: 83–86.
Mah J, Enciso R, Jorgensen M . Management of impacted cuspids using 3-D volumetric imaging. J Can Dent Assoc 2003; 31: 835–841.
Hatcher D, Dial C, Mayorga C . Cone Beam CT for presurgical assessment of implant sites. J Can Dent Assoc 2003; 31: 825–833.
Hamada Y, Kondoh T, Noguchi K . Application of limited cone beam computed tomography to clinical assessment of alveolar bone grafting: a preliminary report. Cleft Palate Craniofac J 2005; 42: 128–137.
Aboudara C, Hatcher D, Nielsen I L, Miller A . A three-dimensional evaluation of the upper airway in adolescents. Orthod Craniofac Res 2003; 6 (Suppl 1): 173–175.
Tsiklakis K, Syriopoulos K, Stamatakis H . Radiographic examination of the temporomandibular joint using cone beam computed tomography. Dentomaxillofac Radiol 2004; 33: 196–201.
Cotton T P, Geisler T M, Holden D T, Schwartz S A, Schindler W G . Endodontic applications of cone-beam volumetric tomography. J Endod 2007; 33: 1121–1132.
Cha J Y, Mah J, Sinclair P . Incidental findings in the maxillofacial area with 3-dimensional cone-beam imaging. Am J Orthod Dentofacial Orthop 2007; 132: 7–14.
Von Torklus D, Gehle W . The upper cervical spine. New York: Grune and Stratton, 1972.
Brown C E . Complete absence of the posterior arch of the atlas. Anat Rec 1941; 81: 499–503.
Geipel P . Zur Kenntnis der Spaltbildungen das Atlas und Epistropheus. Teil IV. Zentralbl Allg Pathol 1955; 94: 19–84.
Ugar D A, Semb G . The prevalence of anomalies of the upper cervical vertebrae in subjects with cleft lip, cleft palate, or both. Cleft Palate Craniofac J 2001; 38: 498–503.
Schrodel M H, Braun V, Stolpe E, Hertlein H . Coincidental deficiency of the posterior arch of the atlas and thalassaemia minor: possible pitfalls in a trauma victim. Emerg Med J 2005; 22: 526–528.
Currarino G, Rollins N, Diehl J T . Congenital defects of the posterior arch of the atlas: a report of seven cases including an affected mother and son. [erratum appears in AJNR Am J Neuroradiol 1994; 15: A9] AJNR Am J Neuroradiol 1994; 15: 249–254.
Phan N, Marras C, Midha R, Rowed D . Cervical myelopathy caused by hypoplasia of the atlas: two case reports and review of the literature. Neurosurgery 1998; 43: 629–633.
Dorne H L, Lander P H . CT recognition of anomalies of the posterior arch of the atlas vertebra: differentiation from fracture. AJNR Am J Neuroradiol 1986; 7: 176–7.
Pick R Y . Cleft arch of atlas simulating fracture of the odontoid process. Spine 1981; 6: 419–422.
Hosalkar H S, Gerardi J A, Shaw B A . Combined asymptomatic congenital anterior and posterior deficiency of the atlas. Pediatr Radiol 2001; 31: 810–813.
Nair M K, Pettigrew J C Jr, Mancuso A A. Intracranial aneurysm as an incidental finding. Dentomaxillofac Radiol 2007; 36: 107–112.
The Ionising Radiation (Medical Exposure) Regulations. Vol. SI 2000. London: The Stationery Office, 2000.
Al-Rawi W et al. Evaluation of web-based instruction for anatomical interpretation in maxillofacial cone beam computed tomography. Dentomaxillofac Radiol 2007; 36: 459–464.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Popat, H., Drage, N. & Durning, P. Mid-line clefts of the cervical vertebrae – an incidental finding arising from cone beam computed tomography of the dental patient. Br Dent J 204, 303–306 (2008). https://doi.org/10.1038/bdj.2008.199
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bdj.2008.199