Key Points
-
Zygomatic implants may be considered as an alternative to bone augmentation procedures in the management of severe maxillary atrophy.
-
The zygomatic implant placement procedure does not require any adjunctive procedure.
-
These implants could be successfully used to support a maxillary overdenture or a fixed bridge.
Abstract
Rehabilitation of the severely resorbed maxilla poses a difficult challenge, for both restorative and surgical colleagues, as the typically large maxillary sinuses in this group of patients require extensive bone grafting if root form dental implant placement is considered. Acceptance is low, due to disadvantages associated with: i) an additional surgical procedure for an iliac bone graft harvesting and, ii) an overall delay in delivery of the final implant-supported prosthesis. The zygomatic implant placement procedure does not require any adjunctive procedures. Furthermore, the ability to immediately use existing dentures and the lack of need for bone grafting and prolonged hospitalisation makes this treatment modality more acceptable to the patient. Four cases are reported that demonstrate the successful treatment of a severely atrophic maxilla with either a fixed prosthesis supported by two zygomatic and a minimum of three standard dental implants or an overdenture supported by two zygomatic and one standard dental implant.
Similar content being viewed by others
Introduction
Placement of dental implants in the posterior maxilla is often jeopardised by the size and extension of the sinus cavities and inadequate amounts of bone. Atrophic processes can be accelerated by removable dentures as well.1 Surgical procedures were therefore developed to elevate the floor of the sinus and fill the hereby created cavity with bone or a substitute material, in order to subsequently install dental implants.2 Autogenous bone, harvested from the iliac crest, remains the optimum bone grafting procedure including maxillary sinus augmentation techniques. In view of the extreme maxillary atrophy, the conventional surgical approach would have been maxillary augmentation with or without a titanium mesh and particulate cancellous bone marrow graft from the iliac bone.3 Another option could have been a Le Fort I osteotomy with an interpositional iliac corticocancellous block graft.4
Extraoral bone harvesting necessitates increased hospitalisation, financial costs, donor site morbidity and functional limitations. Moreover, there is up to 8.6%5 risk of complications following iliac crest bone graft harvesting. Even higher morbidity rates6 including pain (14%) and neurosensory deficits (26%) have been reported lately. Finally, unpredictable reduction in size of the bone graft, because of resorption, is a frequent finding.7
The acceptance of this approach is low by both patients and clinicians due to the following reasons:
-
1
The psychological fear of being subjected to a relatively major surgical procedure
-
2
The need for hospitalisation and morbidity associated with a distant donor site, particularly the restricted mobility associated with an iliac bone graft
-
3
Inability to use the existing denture during the graft healing period. This precaution is intended to minimise graft resorption by eliminating transmission of occlusal loads to the grafted site during the healing phase
-
4
Increased costs of the procedure including the cost of hospital stay, use of in-patient operating facilities and a second surgical team for the bone harvest
-
5
Extended treatment time with delayed implant placement four to six months following the grafting procedure. Simultaneous placement of dental implants at the time of bone grafting is avoided due to a lower success rate than delayed placement.
An alternative treatment for this group of patients is the zygomaticus implant, introduced by Branemark in 19898 (Nobel Biocare AB, Gothenburg, Sweden). The implant is a titanium endosteal implant ranging in length from 30 mm to 52.5 mm. The surgical procedure is carried out under general anaesthesia as described elsewhere.9 Briefly, following bilateral elevation of the buccal mucoperiosteal tissue, removal of the lateral sinus bony window posteriorly and reflection of the antral mucosal lining, two zygomatic implants are inserted engaging the dense bone of the body of zygomatic arch, emerging intraorally in the upper premolar region just palatal to the alveolar crest. Each implant is introduced into the second premolar area, traversing the maxillary sinus, and is placed into the body of the zygomatic bone.
Synchronous placement of a minimum of four dental implants in the canine and the central incisor maxillary area, allows for fabrication of a fixed hybrid prosthesis. Alternatively, placement of two zygomatic implants and at least two standard dental implants at the pyriform buttresses allows construction of a bar to support a maxillary overdenture without the need for any bone grafting. In case more root form dental implants can be placed in the pre-maxilla a fixed prosthesis could be fabricated. The following case reports help to illustrate the above.
Case report 1
Fixed prosthesis supported by two zygomatic and four root form implants
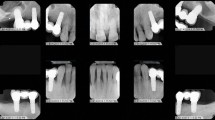
A 52-year-old patient was referred to the Oral Surgery Clinic (Eastman Dental Hospital and Institute) in 1999 complaining of a loose maxillary denture. On clinical examination there was severe maxillary atrophy which was treated with a fixed maxillary prosthesis supported by two zygomatic (Nobel Biocare, Gothenburg, Sweden) and four pre-maxillary machined surface Branemark System implants (Mk III, Nobel Biocare, Gothenburg, Sweden) placed in right and left lateral incisor and canine sites. His medical history included asthma and chronic sinusitis for which he had already received treatment in 1991. The postoperative period was uneventful.
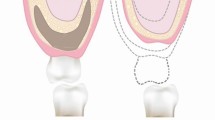
At second stage surgery all implants were exposed and cover screws were replaced by multiunit abutments (MU, Nobel Biocare, Gothenburg, Sweden) of appropriate length (Fig. 1). Additionally the remaining right upper lateral incisor and canine roots were extracted under local anaesthesia. Finally, the patient received a fixed maxillary denture on a gold bar nine months after implant placement (Fig. 2).
Case report 2
Fixed prosthesis supported by two zygomatic and three pre-maxillary root form implants
A 55-year-old patient had severe maxillary atrophy which was treated with a fixed maxillary prosthesis in 2003. This was supported by two zygomatic implants (Nobel Biocare, Gothenburg, Sweden) splinted to three root form machined surface Branemark System implants (Mk III, Nobel Biocare, Gothenburg, Sweden) placed in the anterior maxilla. Initially, a fourth posterior left root form dental implant was placed in the pre-maxilla at the same time of zygomatic implant placement (Fig. 3) however, that implant failed to osseointegrate.
Following placement of the zygomatic implant fixtures, a mixture of Bio-Oss (Geistlich Biomaterials, Inc) with 10 ml of venous blood was used to augment both maxillary sinuses. This was considered appropriate for anticipation of any zygoma fixture failure to osseointegrate, which would necessitate residual maxillary bone of adequate volume for root form implant placement. Two years following implant placement all implants remain osseointegrated with no signs of inflammation and new bone formation in the Bio-Oss augmented sinuses (Fig. 4).
Furthermore, the patient has been satisfied in terms of maxillary prosthesis function and aesthetics (Fig. 5) with minimal encroachment of the palatal space. The prosthodontist provided a framework specifically designed to reduce the palatal bulk of the maxillary prosthesis (Fig. 6).
Case report 3
Fixed prosthesis supported by two zygomatic and six root form implants
A 74-year-old patient with a long history of heavy smoking was referred to the Oral Surgery Clinic (Eastman Dental Hospital and Institute) in 2001 because of a loose maxillary denture with poor stability on two failing dental implants. His medical history was complex involving treatment for Ca of the prostate, nasal trauma and right maxillary sinus surgery. On examination, both implants were loose and there was severe maxillary bone atrophy on the left side and a flabby ridge. Because of his failing dental implants and the history of heavy smoking the patient was not considered suitable for bone augmentation of the maxilla prior to root form dental implant placement. Instead, the patient chose to have a fixed maxillary prosthesis supported by two zygomatic implants (Nobel Biocare, Gothenburg, Sweden) and at least six root form Branemark System implants (Mk III, Nobel Biocare, Gothenburg, Sweden), as the risk of implant failure was considered high.
At the time of operation eight root form implants were placed including one in the incisive maxillary canal and one in the upper right second molar region (Fig. 7). However, it was not considered mandatory to include these last two implants in the final restorative plan as all of the rest of the implants were found to be osseointegrated at second stage surgery six months later. Following cover screw removal 5 mm and 7 mm multi-unit abutments (Nobel Biocare, Gothenburg, Sweden) were attached under local anaesthesia and IV sedation.
Case report 4
Removable over-denture supported by two zygomatic and one root-form implant
A 59-year-old female teacher was referred to the Oral Surgery Clinic (Eastman Dental Hospital and Institute, London) in 2002 for an iliac bone graft in order to augment the severely atrophic maxilla. Her main complaint was inability to tolerate a conventional upper denture and she had unsuccessfully tried six sets of full upper dentures over the last 10-year period. Her last dentist referred her to an implantologist who had placed several endosteal dental implants in the anterior maxilla all of which had failed. The ensuing infection and the surgical procedure for removal of the failed implants had led to an extensive degree of bone resorption. The panoramic radiograph shows the maxillary alveolus completely resorbed down to the level of the sinus and nasal floors (Fig. 8).
Clinical examination demonstrated severe maxillary atrophy to the extent that the labial and buccal sulci were absent. Having explained the risks and the associated morbidity of an extroral bone graft harvesting procedure, as well as the prolonged duration of the treatment, the patient chose the option of an overdenture to be supported by two zygomatic implants and two dental implants placed in the anterior maxilla.
The patient's medical history was non-contributory except for a tentative diagnosis of osteoporosis. Her only medication was hormone replacement therapy. Two 45 mm zygomatic implants (Nobel Biocare AB, Gothenburg, Sweden) were placed engaging the dense bone of the body of zygomatic arch. Anteriorly, the nasal lining was reflected and two 13 mm Mk III regular platform Branemark System implants (Nobel Biocare AB, Gothenburg, Sweden) were inserted in the pyriform buttresses. The dental implants of 13 mm length were completely covered by bone at the time of placement. Despite severe atrophy in both terms of height and width of the anterior maxilla, it is usually feasible to place a root form implant along the pyriform rim at the junction of the maxillary sinus and nasal cavity using a bone expansion technique. The postoperative panoramic and occipitomental views (Fig. 9) show the position and direction of the implants.
The second stage surgery was completed after six months under local anaesthesia. All implants were found to be successfully osseointegrated. A few months later the upper left premaxillary implant became painful and had to be removed. A standard dolder bar was fabricated splinting the two zygomatic implants and the remaining upper right premaxillary implant (Fig. 10). This has provided adequate support and stability for a maxillary overdenture, which the patient has been wearing successfully for the past three years.
Discussion
These case reports demonstrate the value of zygomatic implants in rehabilitation of the severely atrophic maxilla in patients who are unsuitable or unwilling to undergo an extensive bone grafting procedure. In all four cases clinical examination had demonstrated severe maxillary atrophy to the extent that the labial and buccal sulci were absent. Having explained the risks and the associated morbidity of an extraoral bone graft harvesting procedure, as well as the prolonged duration of the treatment, all patients chose the option of a prosthesis to be supported by two zygomatic implants and a minimum of two dental implants placed in the anterior maxilla. The number of pre-maxillary root form implants was further explored following evaluation of the following parameters:
-
Maxillary anatomy and severity of pre-maxillary bone atrophy
-
Pre-existing infection and/or previous surgery
-
Implant positioning based on bone availability
-
Final decision based on type of prosthesis ie fixed or removable taking into account the patients preference and overall costs.
Recently, Bedrossian and coworkers11 performed the procedure successfully in 22 patients under intravenous sedation, which in terms of cost effectiveness is rather beneficial. However, the practice of deep sedation is not common practice in UK hospitals and a day case general anaesthetic or an overnight hospital stay is usually indicated.
The survival rate of zygomatic implants seems higher than the standard premaxillary implants (100% compared to 91.25% respectively).11 Parel and coworkers8 have reported an overall success rate of 97.6% with the placement of over 200 zygomatic implants during the period 1989 to 2001. It has been confirmed by clinical11,12 and anatomical13 studies that the zygomatic bone can offer a predictable anchorage and support function for an implant-supported prosthesis in severely resorbed maxillae.
To improve the success rate, cross-arch stabilisation of the zygomatic implants and the pre-maxillary implants is recommended at second stage surgery. Traditionally two zygomatic implants splinted to two conventional root form pre-maxillary implants have been recommended as the minimum prerequisite for support of a maxillary overdenture. In the fourth patient, despite of the failure of one pre-maxillary implant, an overdenture was successfully supported by two zygomatic implants and the one remaining dental implant.
In addition to their initial use in providing support for maxillary obturators or overdentures, zygomatic implants have also been successfully used to provide a fixed maxillary hybrid prosthesis as was demonstrated in the first three case reports. One criticism to fixed prostheses supported by zygomatic implants has been their bulky palatal emergence and likelihood of reducing the tongue space (Fig. 2). Modifications of implant head angulation design10 or new implant placement techniques with more axial implant inclination were suggested in order to avoid this problem. The Branemark System zygomatic implant has a 45° angulated head which allows for the platform of the implant to be in the same plane as the conventional root form implants in the premaxilla. Lately, a modified zygomatic implant (Southern Implants, SA) with a head angulation of 55° has been designed in order to improve the emergence profile and decrease the buccal cantilever at the level of the occlusal plane.10
Recent advances include: i) a more accurate zygoma implant placement using computer and CT-assisted navigation,18 and ii) a placement appliance,10 which has been designed to facilitate implant placement closer to the alveolar crest, thus enhancing the restorative stages. Additionally, surface enhanced zygomatic implants with either TiU or SLA surfaces along the entire fixture length10 are currently available in order to maximise bone-implant contact and speed the osseointegration process.
Although there is a lack of prospective and comparative studies regarding implant and sinus floor augmentation treatment in large groups of patients with a long-term follow-up, retrospective data14 indicate a success rate of 90% with dental implants placed in augmented sinuses after three years of prosthetic load. However, vital questions regarding the time of implant placement and the ability of regenerated bone to achieve functional osseointegration require further investigation.19 As the residual bone height is often less than 4-5 mm in largely resorbed posterior maxillae, excluding synchronous implant placement at the time of sinus augmentation, the latter takes place six to 12 months following bone graft healing and maturation. Since the accepted healing time for dental implants in the posterior maxilla is six months, the overall treatment time is extended considerably, compared to the shorter time that treatment with zygomatic implants offers.
Despite the success rates well above 90% with zygomatic implants, some surgeons prefer to augment the maxillary sinus at the same time with zygomatic implant placement. This anticipates potential osseointegration failure of the zygomatic fixture and eliminates the need for a subsequent sinus augmentation approach prior to conventional root form implant placement (Fig. 4).
Significant improvement of the quality of life, comparable to maxillary reconstruction with autogenous bone, has also been reported with zygomatic implants placed in patients undergoing maxillectomy and tumour ablation.15 Lately, a modification with insertion of two zygomatic implants in one zygoma was introduced for patients who have undergone maxillectomy.16 Even the possibility of placing double zygomatic implants bilaterally,17 in addition to dental implants in the anterior maxilla, was shown to be successful in a patient who had previously undergone an iliac crest bone graft transplant, which had resorbed.
Additionally, an important benefit of this treatment modality is that unlike the bone grafting procedure, which requires the patient to accept a prolonged period of wearing a modified conventional denture, the patient can wear the old denture immediately after the surgical procedure with only a minor adjustment and reline.
Conclusion
The zygomatic implants seem a predictable and useful alternative to extensive bone grafting procedures in rehabilitation of severely atrophic maxilla. The advantages include:
-
No need for any adjunctive procedure
-
Use of the existing denture immediately
-
No need for prolonged hospitalisation
-
Safety and minimal morbidity in the hands of experienced
-
Cost effectiveness.
Even in a rare case of failure of one of the dental implants, the two zygomatic implants and the one remaining dental implant can still provide a viable long-term solution for an implant supported maxillary overdenture.
Provision of dental prostheses in rehabilitation of these patients by Mr Richard Welfare (Consultant in Restorative Dentistry, Eastman Dental Hospital) and Dr Heilbron (Specialist Prosthodontist) is acknowledged. We would like to thank Professor Malcolm Harris (Oral and Maxillofacial Surgery) for his assistance in preparing the manuscript.
References
Chanavaz M . Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology-Eleven years of surgical experience (1979-1990). J Oral Implantol 1990; 16: 199–209.
Tatum H J . Maxillary and sinus implant reconstruction. Dent Clin North Am 1986; 30: 207–229.
Gongloff R K, Cole M, Whitlow W et al. Titanium mesh and particulate cancellous bone and marrow grafts to augment the maxillary alveolar ridge. Int J Oral Maxillofac Surg 1986; 15: 263–268.
Isaksson S, Ekfeldt A, Alberious P et al. Early results from reconstruction of severely atrophic (class VI) maxillas by immediate endosseous implants in conjunction with bone grafting and Le Fort I osteotomy. J Oral Maxillofac Surg 1993: 22: 144–148.
Younger E M, Chapman M W . Morbidity at bone graft donor sites. J Orthop Trauma 1989; 3: 192–195.
Joshi A, Kostakis G C . An investigation of postoperative morbidity following iliac crest graft harvesting. Br Dent J 2004; 196: 167–171.
Nystrom E, Legrell P E, Forssell A et al. Combined use of bone grafts and implants in the severely resorbed maxilla. Postoperative evaluation by computed tomography. Int J Oral Maxillofac Surg 1995; 24: 20–25.
Parel S M, Branemark P I, Ohrnell L O et al. Remote implant anchorage for the rehabilitation of maxillary defects. J Prosthet Dent 2001; 86: 377–381.
Darle C . Branemark System Nobel Biocare. 2nd edn. Gothenburg, Sweden: Nobel Biocare AB, 2000.
Boyes-Varley J G, Howes D G, Lownie J F et al. Surgical modifications to the Branemark Zygomaticus Protocol in the treatment of the severely resorbed maxilla: a clinical report. Int J Oral Maxillofac Implants 2003; 18: 232–237.
Bedrossian E, Stumpel L III, Beckely M et al. The zygomatic implant: preliminary data on treatment of severely resorbed maxillae. A clinical report. Int J Oral Maxillofac Implants 2002; 17: 861–865.
Malevez C, Abarca M, Durdu F et al. Clinical outcome of 103 consecutive zygomatic implants: a 6-48 months follow-up study. Clin Oral Implants Res 2004; 15: 18–22.
Nkenke E, Hahn M, Lell M et al. Anatomic site evaluation of the zygomatic bone for dental implant placement. Clin Oral Implants Res 2003; 14: 72–79.
Jensen O T, Sculman L B, Block M S et al. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants 1998; 13(supplement): 11–45.
Landes C A . Zygoma implant-supported midfacial prosthetic rehabilitation: a 4-year follow-up study including assessment of quality of life. Clin Oral Implants Res 2005; 16: 315–325.
Nakai H, Okazaki Y, Ueda M . Clinical application of zygomatic implants for rehabilitation of the severely resorbed maxilla: a clinical report. Int J Oral Maxillofac Implants 2003; 18: 566–570.
Balshi T J, Wolfinger G J, Petropoulos V C . Quadruple zygomatic implant support for retreatment of resorbed iliac crest bone graft transplant. Implant Dent 2003; 12: 47–53.
Van Steenberghe D, Malevez C, Cleynenbreugel J et al. Accuracy of drilling guides for transfer from three-dimensional CT-based planning to placement of zygoma implants in human cadavers. Clin Oral Implants Res 2003; 14: 131–136.
Esposito M, Worthington H V, Coulthard P . Interventions for replacing missing teeth: dental implants in zygomatic bone for the rehabilitation of the severely deficient edentulous maxilla. The Cochrane Database of Systematic Reviews 2005; 4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Aghabeigi, B., Bousdras, V. Rehabilitation of severe maxillary atrophy with zygomatic implants. Clinical report of four cases. Br Dent J 202, 669–675 (2007). https://doi.org/10.1038/bdj.2007.479
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bdj.2007.479
This article is cited by
-
Survival and complications of zygomatic implants: a systematic review
Oral and Maxillofacial Surgery (2013)
-
Zygomatic implants: a critical review of the surgical techniques
Oral and Maxillofacial Surgery (2013)