Key Points
-
Provides the first longitudinal study on oral health in ESRD patients.
-
Increases our knowledge concerning the importance of maintained oral health investigations in patients awaiting a renal transplant.
-
Salivary flow rates are only temporary suppressed and increase after renal transplantation.
-
After renal transplantation xerostomia and thirst return to normal, suggesting an important contribution to quality of life.
Abstract
Objectives To compare oral health, salivary flow rate, xerostomia and thirst in end stage renal disease (ESRD) patients remaining on dialysis treatment and after renal transplantation.
Design Longitudinal observation.
Setting ESRD patients recruited from dialysis centres in Amsterdam, The Hague and Utrecht, The Netherlands.
Method At baseline and after two years, salivary flow rates, xerostomia and thirst were determined in 43 ESRD patients. The number of decayed missing filled teeth/surfaces (DMFT/DMFS) was recorded, and periodontal status assessed.
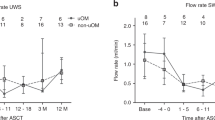
Results After renal transplantation (n = 20), the salivary flow rate increased significantly from UWS = 0.30 ± 0.21 ml/min to 0.44 ± 0.29 ml/min (p <0.001) and the level of xerostomia and thirst decreased. After two years, the percentage of bleeding on probing in dialysis patients (n = 23) decreased from 29.5 ± 25.4% to 10.3 ± 12.3%, (p <0.05). No differences in DMFT and DMFS were observed between dialysis and renal transplant patients.
Conclusions DMFT, dental plaque, gingival bleeding and periodontal indices did not change remarkably after two years, comparing dialysis and renal transplant patients. Renal transplantation enhances salivary flow and decreases symptoms of xerostomia and thirst, and hence enhances the potential to improve the quality of life of affected individuals.
Similar content being viewed by others
Introduction
Over the last decades, the prevalence and incidence of patients with end stage renal disease (ESRD) has increased.1 Due to improvements in medical care and prolonged life expectancy, patients with renal disorders are increasingly encountered in the dental practice.2
A broad variety of oral manifestations have been reported in ESRD patients including gingivitis, xerostomia, ammonia-like smell, mucosal pallor and lesions, tooth mobility, malocclusion and an increased risk of dental erosion due to frequent regurgitation.3,4,5,6,7 Systemic and salivary changes due to chronic renal failure, the use of multiple medication, vomiting and reduced oral self care could all potentially affect oral health in these patients.8,9
The kidneys are essential to remove metabolic waste products, electrolytes and water. When the function of the kidneys is impaired towards 5-10% of the original capacity, ESRD occurs, requiring either haemodialysis (HD) or peritoneal dialysis treatment (PD) or renal transplantation (TX). In HD, an extra-corporal device is used, whereas in PD the peritoneal membrane acts as a filter. TX patients receive their allograft from living or cadaveric donors. To prevent allograft rejection, immunosuppressant therapy is required including the use of prednisolone, ciclosporin or tacrolimus, which could also affect the oral health.4
Relatively little is known about the long-term effects of dialysis treatment on oral health. In addition, most studies on oral health and salivary flow rate in transplantation patients have had a cross-sectional set-up, comparing different renal replacement therapies with healthy controls.7,10,11
Therefore, the aim of this study was to longitudinally compare oral health, salivary flow rate, xerostomia and thirst in dialysis patients with those ESRD patients who were transplanted during this period.
Materials and methods
Participants
ESRD patients undergoing renal replacement therapy for at least three months were asked to participate in a longitudinal study to assess thirst, oral dryness and oral health. One hundred and twenty-six dialysis patients (HD, n = 95; (C)APD, n = 31) gave informed consent to participate in this study. Excluded were 29 patients (23%) because they were edentulous, in addition thirteen participants (10%) were physically not able to participate in the clinical dental investigation. This resulted in 84 patients that were enrolled in this study, which was approved by the Medical Ethical Committee of the Vrije Universiteit Medical Center, Amsterdam, The Netherlands. However, 26 patients died during the two-year study period and 15 subjects were lost to follow up or withdrew. After two years, the data of in total 43 dentate ESRD patients were available for analysis.
Saliva, xerostomia and thirst
Unstimulated whole saliva (UWS) was collected according to the spitting method12 with small modifications, as described previously.13,14 All subjects were instructed to refrain from smoking, eating, drinking and tooth brushing for one hour prior to the three saliva collection periods. Before collection, the mouth was rinsed with tap water. The collection started with the instruction to void the mouth of saliva by swallowing. Subsequently, saliva was allowed to accumulate on the floor of the mouth and the subjects were instructed to spit out into the pre-weighed test tubes every 30 seconds. Each saliva collection period was five minutes long.
Chewing stimulated whole saliva (SWS) was also collected for five minutes using a flat piece of parafilm (5 × 5 cm; 0.30 g; Parafilm “M”, American National CAL, Chicago, USA). During the saliva collection period, the subjects chewed at their own natural pace and stimulated saliva was collected in the same way as the unstimulated samples. The volume of saliva was determined gravimetrically (assuming 1 g = 1 ml) and the pH was determined within five minutes after saliva collection (Sentron pH-system 1001, Roden, The Netherlands).
A validated xerostomia inventory (XI) was used to quantify the level of xerostomia and consisted of 11 items, each with a five point Likert-type scale (never = 1 to very often = 5). Examples of the XI are eg 'My mouth feels dry', 'My lips feel dry' and 'I sip liquids to aid in swallowing food'. The summed scores provide an individual XI score ranging from 11 (no dry mouth) to 55 (extremely dry mouth).14,15
The short-version of the dialysis thirst inventory (DTI) was used to assess the level of thirst. The DTI questionnaire has four items, each with a five point Likert-type scale (never = 1 to very often = 5) providing a DTI score from 4 (no thirst) to 20 (extremely thirsty). The DTI questions are: 'Thirst is a problem for me', 'I am thirsty during the day', 'I am thirsty during the night', and 'My social life is influenced because of my thirst feelings'.16
Oral health assessment
The oral health of the dialysis patients was measured independently by two dentists at a dental office nearby one of the dialysis centres, as described previously.17 The teeth were dried with air and inspected with a standard dental mirror and oral health was determined with several generally accepted oral health indices, such as the decayed, missing, filled teeth index (DMFT), the decayed, missing, filled surfaces index (DMFS) and the simplified oral hygiene index (SOHI).18,19,20 In addition, the periodontal status (bleeding on probing and pocket depth) was assessed using a split mouth model.
Statistical methods
All data are presented as means ± SD. UWS and SWS flow rates showed a skewed distribution and were logarithmically transformed (log10) before statistical analyses. For readability, the original (untransformed) data are presented in Table 1. The patients who remained on dialysis treatment (DIAL-2yr) were compared with those who had received a kidney transplant (TX-2yr). Values of dialysis patients at baseline (DIAL-base) and after two years (DIAL-2yr), and those who were transplanted (TX-2yr) were compared with Student's t-tests. To explore the effects of each treatment modality (DIAL-2yr and TX-2yr) on the main outcome variables, a general linear model of ANOVA (repeated measures design, followed by paired t-tests as a post-hoc procedure) was performed. The statistical analysis was performed using the statistical software package SPSS (version 10.0; SPSS Inc., Chicago, IL. USA). Levels of significance were set at p <0.05 and p <0.001).
Results
Participants
In total 43 chronic dialysis patients participated in this study, 30 men (mean age 54.0 ± 15.7 years) and 13 women (mean age 48.9 ± 17.2 years). At baseline, the mean time on dialysis was 33.0 ± 28.6 months. The main pathologies causing ESRD, classified according to the European Dialysis and Transplantation Association-European Renal Association,21 were polycystic kidney disease – adult type – (14.0%), IgA nephropathy (11.6%), glomerulonephritis (7.0%), miscellaneous (27.9%) and unknown (39.5%). After the two-year study period, 20 patients were transplanted on average 13.5 ± 7.1 months before the second measurement took place. Two TX patients developed gingival overgrowth within renal transplantation. In total 23 patients maintained on dialysis treatment, awaiting a renal transplant.
Saliva, xerostomia and thirst
The salivary flow rate of patients after renal transplantation (TX-2yr) increased significantly from UWS = 0.30 ± 0.21 ml/min at baseline to UWS = 0.44 ± 0.29 ml/min after renal transplantation (p = 0.002, Table 1). In the same patients, the salivary pH of UWS decreased from pH = 7.36 ± 0.49 to 6.74 ± 0.40 (p <0.001). The same pattern was observed for SWS. In patients who remained on dialysis during the study, the salivary flow rate of both UWS and CH-SWS was not altered.
At baseline, the XI values in those who remained on dialysis were higher (XI = 29.5 ± 7.5) than those who would receive a renal transplant (XI = 24.9 ± 7.5) (p <0.05, Table 1). No other baseline differences were observed. In TX patients, the XI-scores decreased from 24.9 ± 8.1 to 21.4 ± 7.6, after two years (p = 0.065). No changes were observed for the XI-scores after two years follow up, in patients who remained on dialysis. Also thirst in TX patients decreased significantly from DTI = 10.6 ± 4.4 to DTI = 8.1 ± 2.6, (p = 0.02). In patients maintaining on dialysis, no changes occurred and the DTI-score did not change (Table 1).
Oral health
Although the average DMFS and DMFT values slightly increased after two years, no statistically significant differences were observed between TX and dialysis patients (Table 2). In those patients who remained on dialysis, an increase in the number of missing surfaces (MS) was found from MS = 18.5 ± 2.9 to MS = 20.6 ± 25.6, after two years (p = 0.017). Subsequently, the DMFS value of these patients increased significantly (Table 2).
In both groups, the percentage of teeth without dental plaque remained stable throughout the study (Table 3). The average percentage of explored sites that showed immediate bleeding on probing decreased significantly from 29.5 ± 25.4% to 10.3 ± 12.3% in patients continuing dialysis treatment. Also, in TX patients, the percentage bleeding on probing decreased by 10%, although no statistically significant difference was found. In addition, no differences were found between TX patients and those who remained on dialysis with respect to the pocket depth and bleeding measurements.
Discussion
To our knowledge, this is the first longitudinal study to compare the course and changes in salivary flow rate, xerostomia, thirst and oral health of patients who remained on dialysis treatment, with those who received a renal transplant (TX). It was revealed that oral dryness and thirst decreased after renal transplantation. In patients who remained on dialysis, the salivary variables and levels of xerostomia and thirst remained the same throughout the two-year study period. This indicates that thirst and oral dryness is a continuing problem in these patients. In dialysis patients, a significant increase in the number of MS and DMFS, and a reduction of bleeding on probing was found after the two-year observation period.
It was found that the salivary flow rates (both UWS and SWS) increased in the TX patients, while remaining the same in patients on dialysis. Other studies have shown reduced salivary flow rates in HD patients compared to healthy controls.7,22,23,24 Our observation that the salivary flow rates increase after renal transplantation does not support the suggestion that dialysis treatment affects the salivary glands.25 In the present study, we have shown that the reduced salivary flow rates are reversible and restore after transplantation. The salivary flow rates in TX patients might even have been underestimated since several studies have indicated that long term use of immunosuppressant therapy such as ciclosporin could suppress the salivary flow rate.26,27
A decrease in salivary pH after transplantation is probably due to the reduced concentration of urea in saliva which can be hydrolysed by oral bacteria into ammonia (with a relatively high pH).28 A high salivary pH and buffering capacity in dialysis patients could potentially enhance remineralisation, although we could not demonstrate this effect in the present study.29,30,31,32
As initially expected, we have found decreased oral dryness and thirst in patients after renal transplantation. After renal transplantation, the physiological function of the kidney should restore electrolyte levels, fluid balance, thirst, xerostomia and serum composition to normal. Previously, we have demonstrated in haemodialysis patients that salivary flow rate and xerostomia are significantly correlated.14 Therefore an increase in UWS salivary flow rate after renal transplantation could explain a decreased level of xerostomia.33
The number of MS increased in those who remained on dialysis therapy, and no changes occurred in the transplantation group after two years. This might be explained since most patients awaiting a renal transplant have to undergo an oral examination to become foci free, which is part of the preoperative evaluation.6 Furthermore, the continued xerostomia may have contributed to the increase in dental disease in patients remaining on dialysis. In addition, we have previously found no differences for the DMFS, DMFT and periodontal indices between ESRD patients and a matched (age and educational status) control group.17 In two patients, markedly increased gingival overgrowth was found after renal transplantation. Many other studies have reported this phenomenon in ESRD patients after renal transplantation.34,35 Thomason and colleagues35 reported gingival overgrowth in 30% of transplanted patients after the use of ciclosporin. As an alternative, tacrolimus can be used which has been shown to be successful as an immunosuppressant with less gingival overgrowth.36
Although renal transplantation is a permanent solution in approximately half of the patients with ESRD, the long term use of immunosuppressive medication may have serious disadvantages such as an increased risk of opportunistic infections and immunosuppression-related tumours.37 Although two patients had gingival overgrowth, the average bleeding scores did not increase but slightly decreased in the TX group after renal transplantation. In a study with 32 transplant patients on immunosuppressive therapy, it was found that pocket depths, plaque and gingivitis scores did not change significantly before and after renal transplantation.38 In our study, the percentage of teeth which showed bleeding on probing decreased in both the dialysis and transplanted patients. A study comparing 36 HD patients with 36 controls revealed no statistically significant difference for the periodontal status between these two groups.11 The decreased levels of bleeding on probing we have found, illustrate less acute inflammation of the gingiva. This might be associated with improved oral hygiene procedures, reduced dental plaque scores or the immunosuppressive drugs.11,39 The oral hygiene measures, however, remained the same throughout the study period (data not shown). Also the level of dental plaque did not differ between baseline and after two years, which is in accordance with Rahman and colleagues,10 who found no differences in sulcular bleeding index score or gingival index score between healthy subjects, patients on HD or those after renal transplantation.
In conclusion, oral health aspects such as caries, dental plaque, gingival bleeding and periodontal indices did not change remarkably after a two-year period in ESRD patients remaining on dialysis and those who received a renal transplant. Regular dental examination and instruction in patients awaiting a renal transplantation is of vital importance to ensure optimal oral health, in order to remain foci free to prevent rejection of the allograft after transplantation. Decreased levels of xerostomia and thirst were observed in patients after renal transplantation, which could add to the quality of life of these patients.
References
Feest T G, Rajamahesh J, Byrne C et al. Trends in adult renal replacement therapy in the UK: 1982-2002. QJM 2005; 98: 21–28.
Greenwood M, Meechan J G, Bryant D G. General medicine and surgery for dental practitioners. Part 7: renal disorders. Br Dent J 2003; 195: 181–184.
Naugle K, Darby M L, Bauman D B, Lineberger L T, Powers R. The oral health status of individuals on renal dialysis. Ann Periodontol 1998; 3: 197–205.
Proctor R, Kumar N, Stein A, Moles D, Porter S. Oral and dental aspects of chronic renal failure. J Dent Res 2005; 84: 199–208.
Clark D B. Dental findings in patients with chronic renal failure. An overview. J Can Dent Assoc 1987; 53: 781–785.
Naylor G D, Fredericks M R. Pharmacologic considerations in the dental management of the patient with disorders of the renal system. Dent Clin North Am 1996; 40: 665–683.
Gavalda C, Bagan J, Scully C, Silvestre F, Milian M, Jimenez Y. Renal hemodialysis patients: oral, salivary, dental and periodontal findings in 105 adult cases. Oral Dis 1999; 5: 299–302.
Atassi F. Oral home care and the reasons for seeking dental care by individuals on renal dialysis. J Contemp Dent Pract 2002; 3: 31–41.
Epstein S R, Mandel I, Scopp I W. Salivary composition and calculus formation in patients undergoing hemodialysis. J Periodontol 1980; 51: 336–338.
Rahman M M, Caglayan F, Rahman B. Periodontal health parameters in patients with chronic renal failure and renal transplants receiving immunosuppressive therapy. J Nihon Univ Sch Dent 1992; 34: 265–272.
Marakoglu I, Gursoy U K, Demirer S, Sezer H. Periodontal status of chronic renal failure patients receiving hemodialysis. Yonsei Med J 2003; 44: 648–652.
Navazesh M. Methods for collecting saliva. Ann N Y Acad Sci 1993; 694: 72–77.
Bosch J A, Brand H S, Ligtenberg T J, Bermond B, Hoogstraten J, Nieuw Amerongen A V. Psychological stress as a determinant of protein levels and salivary-induced aggregation of Streptococcus gordonii in human whole saliva. Psychosom Med 1996; 58: 374–382.
Bots C P, Brand H S, Veerman E C I et al. Interdialytic weight gain in patients on hemodialysis is associated with dry mouth and thirst. Kidney Int 2004; 66: 1662–1668.
Thomson W M, Chalmers J M, Spencer A J, Williams S M. The xerostomia inventory: a multi-item approach to measuring dry mouth. Community Dent Health 1999; 16: 12–17.
Bots C P, Brand H S, Veerman E C I et al. Chewing gum and a saliva substitute alleviate thirst and xerostomia in patients on hemodialysis. Nephrol Dial Transplant 2005; 20: 578–584.
Bots C P, Poorterman J H G, Brand H S et al. The oral health status of dentate patients with chronic renal failure undergoing dialysis therapy. Oral Dis 2006; 12: 176–180.
Greene J C, Vermillion J R. The simplified oral hygiene index: a method for classifying oral hygiene status. J Am Dent Assoc 1964; 68: 7–13.
World Health Organisation. Oral health survey. Basic methods. Geneva: WHO, 1987.
Marks R G, Magnusson I, Taylor M, Clouser B, Maruniak J, Clark W B. Evaluation of reliability and reproducibility of dental indices. J Clin Periodontol 1993; 20: 54–58.
EDTA-ERA and WHO diagnostic codes. Nephrol Dial Transplant 1993; 6: 524–525.
Bayraktar G, Kazancioglu R, Bozfakioglu S, Ecder T, Yildiz A, Ark E. Stimulated salivary flow rate in chronic hemodialysis patients. Nephron 2002; 91: 210–214.
Kho H S, Lee S W, Chung S C, Kim Y K. Oral manifestations and salivary flow rate, pH, and buffer capacity in patients with end-stage renal disease undergoing hemodialysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 88: 316–319.
Postorino M, Catalano C, Martorano C et al. Salivary and lacrimal secretion is reduced in patients with ESRD. Am J Kidney Dis 2003; 42: 722–728.
Rothstein D, Yudis M, Shaw A S, Onesti G. Massive neck swelling secondary to uremic submaxillary gland involvement. Oral Surg Oral Med Oral Pathol 1969; 27: 333–336.
Benderli Y, Erdilek D, Koray F, Telci A, Turan N. The relation between salivary IgA and caries in renal transplant patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89: 588–593.
Dehpour A R, Shirzad N, Ghafourifar P, Abdollahi M. Effects of ciclosporine A on the functions of submandibular and parotid glands of rats. Gen Pharmacol 1996; 27: 887–890.
Burne R A, Marquis R E. Alkali production by oral bacteria and protection against dental caries. FEMS Microbiol Lett 2000; 193: 1–6.
Narhi T O, Ainamo A, Meurman J H. Salivary yeasts, saliva, and oral mucosa in the elderly. J Dent Res 1993; 72: 1009–1014.
Al Nowaiser A, Roberts G J, Trompeter R S, Wilson M, Lucas V S. Oral health in children with chronic renal failure. Pediatr Nephrol 2003; 18: 39–45.
Peterson S, Woodhead J, Crall J. Caries resistance in children with chronic renal failure: plaque pH, salivary pH, and salivary composition. Pediatr Res 1985; 19: 796–799.
Edgar W M, Higham S M. Role of saliva in caries models. Adv Dent Res 1995; 9: 235–238.
Dawes C. How much saliva is enough for avoidance of xerostomia? Caries Res 2004; 38: 236–240.
Spratt H, Boomer S, Irwin C R et al. Ciclosporin associated gingival overgrowth in renal transplant recipients. Oral Dis 1999; 5: 27–31.
Thomason J M, Seymour R A, Ellis J. The periodontal problems and management of the renal transplant patient. Ren Fail 1994; 16: 731–745.
James J A, Jamal S, Hull P S et al. Tacrolimus is not associated with gingival overgrowth in renal transplant patients. J Clin Periodontol 2001; 28: 848–852.
London N J, Farmery S M, Will E J, Davison A M, Lodge J P. Risk of neoplasia in renal transplant patients. Lancet 1995; 346: 403–406.
Tollefsen T, Johansen J R. Periodontal status in patients before and after renal allotransplantation. J Periodontal Res 1985; 20: 227–236.
Been V, Engel D. The effects of immunosuppressive drugs on periodontal inflammation in human renal allograft patients. J Periodontol 1982; 53: 245–248.
Acknowledgements
The authors would like to thank the nephrologists Dr R. M. Valentijn (RKZ, The Hague), Dr P. F. Vos (Dianet, Utrecht) and Dr J. A. Bijlsma (Dianet, Amsterdam) for providing access to the patients and their valuable contribution to the project. We are also indebted to the staff of LAKS (AMC Hospital, Amsterdam) for analysing the electrolytes in saliva. Furthermore, we would like to thank Dr P. D. Bezemer (KEB, VUMC, Amsterdam) for advice with the design of this study and F. Tromp (Diasoft, Leusden) for retrieving clinical data from the Diamant® database.
This study was financially supported by grants from the Dutch Kidney Foundation and The Netherlands Institute for Dental Sciences (IOT).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Bots, C., Brand, H., Poorterman, J. et al. Oral and salivary changes in patients with end stage renal disease (ESRD): a two year follow-up study. Br Dent J 202, E7 (2007). https://doi.org/10.1038/bdj.2007.47
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bdj.2007.47
This article is cited by
-
Otorhinolaryngological dysfunctions induced by chronic kidney disease in pre- and post-transplant stages
European Archives of Oto-Rhino-Laryngology (2020)
-
Oral behavior, dental, periodontal and microbiological findings in patients undergoing hemodialysis and after kidney transplantation
BMC Oral Health (2016)
-
Xerostomia in patients on chronic hemodialysis
Nature Reviews Nephrology (2012)