Abstract
Acetylthevetin B (ATB), a cardiac glycoside from the seed of Thevetia peruviana (Pers) K Schum (yellow oleander), exhibits not only antitumor activity but also potential cardiac toxicity. In the present study, we attempted to enhance its antitumor action and decrease its adverse effects via chitosan-Pluronic P123 (CP) micelle encapsulation. Two ATB-loaded CP micelles (ATB-CP1, ATB-CP2) were prepared using an emulsion/solvent evaporation technique. They were spherical in shape with a particle size of 40–50 nm, showed a neutral zeta potential, and had acceptable encapsulation efficiency (>90%). Compared to the free ATB (IC50=2.94 μmol/L), ATB-loaded CP micelles exerted much stronger cytotoxicity against human lung cancer A549 cells with lower IC50 values (0.76 and 1.44 μmol/L for ATB-CP1 and ATB-CP2, respectively). After administration of a single dose in mice, the accumulation of ATB-loaded CP1 micelles in the tumor and lungs, respectively, was 15.31-fold and 9.49-fold as high as that of free ATB. A549 xenograft tumor mice treated with ATB-loaded CP1 micelles for 21 d showed the smallest tumor volume (one-fourth of that in the control group) and the highest inhibition rate (85.6%) among all the treatment groups. After 21-d treatment, no significant pathological changes were observed in hearts and other main tissues. In summary, ATB may serve as a promising antitumor chemotherapeutic agent for lung cancer, and its antitumor efficacy was significantly improved by CP micelles, with lower adverse effects.
Similar content being viewed by others
Introduction
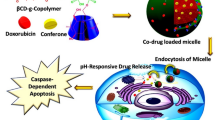
Cardiac glycosides (CGs) are a class of natural products with a steroid-like structure containing an unsaturated lactone ring and a sugar chain, and they are considered amphiphilic molecules1. CGs are traditionally used in cardiology for the treatment of cardiac congestion and some types of cardiac arrhythmias2. Recent in vitro and ex vivo experiments have revealed that several CGs can induce potent and selective anticancer effects at standard therapeutic doses3. Therefore, CGs may be utilized as anticancer agents. However, many CGs that show strong antitumor activity in vitro have not passed Phase I clinical trials, primarily because the CGs show a lack of tumor selectivity and severe adverse effects, particularly cardiotoxicity4,5. Therefore, the exploration of effective delivery systems is necessary to enhance the antitumor efficacy and decrease the adverse effects of CGs.
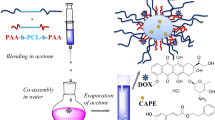
Nanotechnology-based drug delivery systems have received increasing attention because of their ability to load therapeutics and deliver drugs to the site of action, thereby improving the pharmacokinetics of the loaded drugs and reducing off-target toxicity. Among these systems, amphiphilic block co-polymers that spontaneously form self-assembled micellar structures have shown favorable biocompatibility and solubilization effects for amphiphilic drug molecules, including CGs6. In addition, unlike small molecules, which diffuse in and out of the interstitial space of tumors, nanocarriers (between 10 and 100 nm) have long circulatory properties that enable polymeric micelles to accumulate in tumor tissue via a passive targeting phenomenon, commonly referred to as an enhanced permeability and retention (EPR) effect7,8. Inspired by the superiority of nanosized micelles, we intended to deliver CGs to tumor cells using polymeric micelles, which may enhance antitumor efficacy and decrease the cardiotoxicity associated with these drugs.
In a previous study, we observed that acetylthevetin B (ATB), a CG isolated from the seeds of Thevetia peruviana (Pers) K Schum (yellow oleander), showed strong cytotoxicity toward three cancer cell lines (human lung cancer cells P15, human gastric cancer cells MGC-803, and human pancreatic cancer cells SW1990) but not toward the normal hepatocyte LO2 cell line9. To increase targeting potential toward lung cancer and decrease cardiac toxicity, we attempted to establish a nanotechnology-based drug delivery model for ATB. Previous studies have reported the wide exploitation of certain polymeric materials in lung-targeting delivery systems7,10,11,12,13,14,15,16,17,18,19,20,21,22. Chitosan reportedly exhibits exceptional adhesion ability with lung cancer cells through H-bonding interaction and biotic stickiness23,24,25,26. In addition, Pluronic copolymers, which have a hydrophilic and flexible nature similar to PEG27,28,29, are often used to prevent the adsorption of plasma protein, resulting in increased accumulation at the tumor site30,31,32,33,34. Thus, we sought to exploit and combine the biotic stickiness of chitosan and the enhanced accumulation effect of PEGylation to generate polymer micelles to promote the affinity and cellular uptake of ATB toward lung tumor cells. The cellular uptake, inhibitory effects on A549, in vitro cytotoxicity, A549 targeting potential, and in vivo antitumor activity of ATB-loaded CP micelles were evaluated.
Materials and methods
Materials
Acetylthevetin B (ATB) was obtained from the seeds of Thevetia peruviana (Pers) K Schum (yellow oleander)9, with a purity >98% according to the HPLC analysis (Figure S1, S2, S3, S4, S5).
Pluronic® P123 (PEO20-PPO70-PEO20, MW 5800 Da, PEO 30 wt%) was obtained from Sigma Aldrich (St Louis, MO, USA). Chitosan (CS, MW 10 kDa, deacetylation degree: >90%) was obtained from the Zhejiang Golden Shell Pharmaceutical Co, Ltd (Yuhuan, China). N,N'-Disuccinimidyl carbonate (DSC), 4-dimethylaminopyridine (DMAP), coumarin-6, acetonitrile, diethyl ether, isopropanol, and ethanol were obtained from the Sinopharm Chemical Reagent Co, Ltd (Shanghai, China). Hoechst 33342, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), the cell cycle and apoptosis analysis kit were purchased from the Beyotime Institute of Biotechnology (Shanghai, China). Dulbecco's modified Eagle's medium (DMEM), fetal bovine serum (FBS), penicillin/streptomycin, and 1×trypsin EDTA solution (0.25%, trypsin with 0.53 mmol/L EDTA) were purchased from Life Technologies Co (Grand Island, NY, USA). Alexa Fluor® 555 conjugate WGA and 1,1'-dioctadecyl-3,3,3',3'-tetramethylindotricarbocyanine iodide (DIR) were obtained from Invitrogen (Carlsbad, CA, USA). The water used for all experiments and analyses was deionized and filtered using a 0.22-μm pore size polycarbonate syringe filter (Millipore, Billerica, MA). All chemicals were of reagent grade and used without further purification or modification.
Preparation of ATB-based formulations
ATB-based micelles were prepared using the following procedure. Briefly, 9 μmol of CS, 3 μmol of P123 and 15 mg of ATB were dissolved in 15 mL of ethanol, followed by desiccation and subsequent rehydration at a concentration of 1 mg/mL ATB-CP1 in 15 mL of phosphate-buffered saline (PBS) (pH 7.4). The mixture was homogenized using a high-pressure homogenizer (Nanodebee, South Easton, MA, USA) for three cycles under 600 psi. For ATB-CP2 micelles, 3 μmol of CS and 9 μmol of P123 were used, and all other materials and procedures were the same as described for the preparation of ATB-CP1 micelles.
Characterization
The particle size distribution and zeta potential of micelles were determined using a Zetasizer Nano ZS analyzer (Malvern, Worcestershire, UK). The micelles were evaluated for shape using transmission electron microscopy (TEM) (Tecnai G2 Spirit Twin, FEI, USA).
The entrapment efficiency (EE, %) was determined using an ultrafiltration-centrifugation technique35. The recovery of this method was validated. The ATB loaded micelles (500 μL) were placed into filter units (10 000 MW, Millipore, Massachusetts, USA) and centrifuged at 3000 r/min for 30 min. Free ATB not incorporated into micelles was separated in the ultrafiltrate. The content of free or total ATB in the micelles was determined using HPLC. Subsequently, the EE% was calculated according to the following Eq:

where WT is the weight of total drug in the micelles and WF is the weight of free drug in the ultrafiltrate after centrifugation.
The in vitro release behavior of ATB from micelles was measured using a dialysis method36. One milliliter of ATB solution, ATB-CP1, and ATB-CP2 were placed separately into a dialysis tube with a molecular weight cut off of 8 000–14 000 (Sinopharm Chemical Reagent, Shanghai, China) and dialyzed in 20 mL of PBS (pH 7.4, 37 °C). At various times (1, 2, 4, 8, 12, and 24 h), all buffers were replaced with an equal volume of fresh PBS, and the concentration of ATB in the dialysis buffer was analyzed using HPLC.
Cell line and cell culture
The human lung carcinoma cell line A549 was obtained from the Shanghai Institutes for Biological Sciences. The cells were cultured in DMEM medium with 10% FBS and 0.01% penicillin-streptomycin. The cells were maintained at 37 °C in a humidified atmosphere (air supplemented with 5% CO2) and passaged using 0.25% trypsin at a subcultivation ratio of 1:3.
Cellular uptake of ATB-based formulations
To determine the cellular uptake of the micelles, ATB-CP1 and ATB-CP2 micelles were labeled with coumarin-6. First, 0.75 mg of coumarin-6 and CP polymer were dissolved in ethanol, dried to a thin film and subjected to the same procedure as described above (section 2.2, preparation of ATB-based formulations).
For confocal analysis, A549 cells were seeded onto 10 mm2 glass coverslips in 24-well plates at a density of approximately 1×105 cells per well and subsequently incubated for 24 h to enable attachment. The cells were initially incubated with Hoechst 33242 at 37 °C to visualize the nuclei. After 30 min of incubation with coumarin-6-labeled CP1 and CP2 micelles, the medium was removed, and the cells were washed three times with PBS. The cells were subsequently incubated with Alexa Fluor® 555 conjugate WGA to visualize the membrane. The intracellular distribution of CP micelles was observed using a FluoView FV1000 Confocal Microscope (Olympus, Tokyo, Japan).
The cellular uptake of CP1 and CP2 micelles was measured by flow cytometry (FCM). A549 cells were seeded onto 24-well plate and cultured until a confluent monolayer formed. After removing the culture medium, the cells were incubated with coumarin-6-labeled CP1 and CP2 micelles for 30 min at 37 °C. The cells were subsequently washed three times with PBS (pH 7.4), trypsinized, and centrifuged at 2000×g. The harvested cells were re-suspended and analyzed using FACScan flow cytometry (BD, Franklin Lakes, NJ, USA).
Cytotoxicity assay in vitro
To measure the cytotoxicity of ATB solutions and ATB-CP1 and ATB-CP2 micelles, an MTT cell viability assay was performed36. A549 cells were plated onto 96-well plates at a density of 1×104 cells per well and incubated for 24 h to enable attachment. Subsequently, the growth medium was removed, and free ATB, ATB-CP1, and ATB-CP2 micelles at various ATB concentrations of 1, 3, 5, 10, and 20 μg/mL were added. The MTT assay was performed after incubating cells for 24 and 48 h at 37 °C.
Cell cycle analysis
Cell cycle distribution was analyzed through flow cytometry. A549 cells were seeded onto 12-well plates at 1×106 cells per well and further incubated for 12 h. A549 cells were treated with free ATB, ATB-CP1, and ATB-CP2 micelles at an ATB concentration of 10 μg/mL for 12 h. The cells were trypsinized, washed three times with PBS, and subsequently fixed in 70% ethanol for at least 1 h at -20 °C. The fixed cells were washed with PBS and re-suspended in 0.5 mL propidium iodide (PI) staining solution (69 mmol/L PI, 38 mmol/L sodium citrate and 0.7 mg/mL RNase A, pH 7.4) for 30 min at 37 °C in the dark. The stained cells were processed through flow cytometry.
Animals
Male BALB/c nu/nu nude mice (4–6 weeks old, 20±2 g) were obtained from the Animal Facility of the Shanghai Institute of Materia Medica (Shanghai, China) and housed in a 12-h/12-h light-dark cycle at a room temperature of 23±2 °C with a relative humidity of 55%±15%. Food and water were provided ad libitum throughout the acclimatization and experimental periods. The animal experiments were reviewed and approved through the Institutional Animal Care and Use Committee (IACUC) of the Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai, China.
Examination of biodistribution through in vivo imaging
A549 cells (5×106 cells) were subcutaneously (sc) implanted into the fourth mammary fat pads of 4–6 weeks old male BALB/c nu/nu nude mice to establish xenograft tumors. Two weeks after tumor implantation, the mice were randomized into three treatment groups of free ATB, ATB-CP1, and ATB-CP2 micelles (3 mice per group).
The biodistribution of free ATB, ATB-CP1, and ATB-CP2 micelles was analyzed using a non-invasive in vivo optical imaging technique37. The mice were treated with NIR fluorescent-labeled ATB and micelles. DIR, a recently introduced carbocyanine lipophilic NIR fluorescent membrane dye, was used to label the free ATB and micelles38. DIR-labeled ATB solution was prepared by dissolving 0.25 mg of DIR and 12.5 mg of ATB in 2.5 mL of ethanol, followed by dilution at a concentration of 5 mg/mL ATB in 50 mL of saline. DIR-labeled micelles were prepared by dissolving DIR, ATB and polymers in ethanol, followed by drying to a thin film, according to the procedure described above (section 2.2, preparation of ATB-based formulations). The final concentration of DIR was 100 μg/mL in each formulation.
Free DIR, DIR-ATB, and DIR-labeled micelles (DIR-ATB-CP1 and DIR-ATB-CP2) were administered through intravenous (iv) injection by tail (10 μg DIR of each mouse). At 15 min and 6 h post injection, the biodistributions of DIR-labeled formulations in live (15 min and 6 h post injection) and euthanized animals (6 h post injection) were investigated using the IVIS® Spectrum System (Caliper Cor, Waltham, Massachusetts, USA). The excitation and emission wavelengths were 745 and 800 nm, respectively.
The results were analyzed using Living Image® Software Version 4.3.1 (Caliper Corp, Waltham, Massachusetts, USA). All experiments were repeated in three different animals, and representative pictures are shown19.
In vivo antitumor activity and cytotoxicity in an A549 xenograft model
A549 cells (5×106 cells) were implanted (sc) into the fourth mammary fat pads of 4–6-week-old male BALB/c nu/nu nude mice to establish xenograft tumors. Two weeks after tumor implantation, the mice were randomly divided into four groups (6 mice per group; free ATB, ATB-CP1, ATB-CP2 and control) and administered ATB-based formulations for 3 weeks. The drug-treated groups received 1.5 mg/kg of ATB through iv injection via the tail vein every 3 d. The control mice received the same volume of physiological saline. The body weights were monitored every 3 d. The tumor-bearing mice were euthanized through CO2 asphyxiation on d 22, and the livers were excised. The tumors were detached and weighed, and the tumor volume was determined using a slide gauge according to the following formula39:

Tumor tissues were removed from the euthanized mice and weighed to calculate the tumor inhibition rate:

where Wt and Wc are the mean tumor weights of the treated groups and the negative control group, respectively. Moreover, the main tissues, including heart, liver, spleen, lung, and kidney, were rinsed with normal saline, fixed in 10% formalin, and subsequently embedded in paraffin blocks for slicing and staining with hematoxylin and eosin (H&E). The sections were observed under a microscope for histopathological evaluation40.
Statistical analysis
The data from each treatment and control group are present as the mean±SD. Statistical analysis was performed using Student's t-test and ANOVA.
Results
Characterization of ATB-loaded micelles
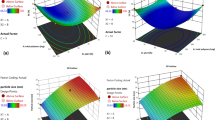
The ATB concentration in ATB-CP1 and ATB-CP2 micelles was 1 mg/mL. The physicochemical characteristics and entrapment efficiency (EE, %) parameters for ATB-CP1 and ATB-CP2 are summarized in Table 1. The two types of micelles had a mean particle size of approximately 40–50 nm. All formulations exhibited a similar neutral surface charge (∼0 mV). ATB was encapsulated into the two different micelles with high EE% of >90%. As presented in Figure 1A, the micelles imaged using TEM had spherical shapes, and the size correlated well with the results of laser diffraction (Table 1).
(A) Transmission electron microscopy (TEM) images of CP1 and CP2 micelles. (B) Release profile of acetylthevetin B (ATB) from free ATB, ATB-CP1, and ATB-CP2 in phosphate buffer solution (PBS) (pH 7.4) at 37 °C.
In the present study, PBS was applied as the release medium. The in vitro cumulative release profiles of ATB from different formulations are shown in Figure 1B. The free ATB released from the solution was investigated as a control. The results showed that approximately 100% ATB in the stock solution was released within 4 h, suggesting that ATB could freely diffuse through the dialysis membrane. The 4-h cumulative ATB release from ATB-CP1 was 60.3%±0.9%, compared with 50.3%±2.5% for ATB-CP2, suggesting the prolonged release of ATB from the micelle preparation.
Cellular uptake of micelles
To investigate the cellular uptake of ATB-based formulations, A549 lung tumor cells were incubated with coumarin-6 labeled CP micelles, followed by confocal microscopy and quantitative analysis using flow cytometry. The nuclei were stained with Hoechst. The green fluorescence showed the micelle uptake by the cells, and the membranes were stained with red. As shown in Figure 2, the CP micelles distributed in the cytoplasm after intake by A549 cells. CP1 showed stronger colocalization with the membrane of A549 cells compared to CP2. The CP1 uptake in A549 cells was markedly higher than that of CP2. The mean fluorescent intensity of CP1 micelles in A549 was 2.82 times higher than that of CP2, with a statistical significant difference between CP1 and CP2 (733.33 vs 260.00, P<0.01).
(A) Confocal microscopy images of A549 cells after 30 min incubation with coumarin-6 labeled CP1 and CP2 micelles and the correlation scatter plot of the intensities of coumarin-6 and Alexa Fluor® 555 WGA. (B) The cellular uptake of CP1 micelles are shown in light blue and the cellular uptake of CP2 micelles are shown in dark blue while the black line represents the negative control. The error is the standard deviation from the mean. n=3. **P<0.01.
Enhanced cytotoxicity and apoptosis of A549 cells induced through ATB-based formulations
The above data demonstrates that ATB-CP1 could enhance cellular uptake in A549 cells. As a result, the delivery of ATB with CP1 micelles can markedly increase the concentration of the free drug in A549 cells, thereby increasing drug cytotoxicity. To determine the cytotoxic effects, we incubated free ATB, ATB-CP1, and ATB-CP2 with A549 cells. All ATB formulations showed dose-dependent and time-dependent toxicity (Figure 3A, 3B). In addition, free ATB showed obvious cytotoxicity against A549 cells (IC50=2.94 μmol/L) after incubation for 48 h, and ATB-CP1 had significantly increased cytotoxicity (IC50=0.76 μmol/L) compared with free ATB and ATB-CP2 (IC50=1.44 μmol/L). This finding might result from the enhanced cellular ATB retention.
In vitro cytotoxicity of free acetylthevetin B (ATB), ATB-CP1, and ATB-CP2 against A549 cells. Cell viability of A549 cells after incubating with free ATB, ATB-CP1, and ATB-CP2 at different concentrations for 24 h (A) and 48 h (B). (C) Cell cycle distribution of A549 cells treated with ATB solution, ATB-CP1, and ATB-CP2 at a concentration of 10 μg/mL for 12 h by flow cytometry.
To evaluate the mechanism of cytotoxic effects, the DNA content of A549 cells (after treatment with various formulations) was examined using FCM to assess cell cycle progression. As shown in Figure 3C, the cell cycle distribution revealed that 50.18% of the control cells were in G0/G1 phase, whereas the G0/G1 population decreased to 49.68%, 21.46%, and 40.92% for the free ATB solution, ATB-CP1, and ATB-CP2, respectively. Moreover, 32.98% of the control cells were in the S phase, close to the 26.28% of free ATB solution-treated cells, whereas the S population increased to 55.61% and 56.01% for ATB-CP1 and ATB-CP2, respectively.
Biodistribution of micelles in mice bearing orthotopic xenograft tumors
DIR integrates with high stability into micelles and remains attached, even when in contact with other membranes. To determine the real-time biodistribution of micelles, free DIR solution, DIR-labeled free ATB (DIR is an amphiphilic material similar to ATB, which micellizes with ATB; its amount in formulation is controlled at far below the amount of ATB to ensure that the distribution of this formulation could reflect the distribution of free ATB), and micelles were intravenously injected into mice bearing A549 orthotopic xenograft tumor; the in vivo targeting efficacy of the formulations was observed using non-invasive NIRF imaging in live animals (Figure 4A). The selected ICG filter facilitated the precise detection of the DIR fluorophore, as all autofluorescence signals were effectively blocked (Figure 4A and 4B). After the iv administration of DIR-labeled formulations, a strong NIRF signal from DIR-ATB-CP1 and DIR-ATB-CP2 micelles was observed in the tumor (the position of the tumor is shown as a black circle in Figure 4A), whereas fewer signals from the free DIR solution and DIR-labeled free ATB solution could be observed in the orthotopic xenograft tumor. At the 6-h time point, no obvious NIRF signal from the ATB solution was observed in the tumor, whereas DIR-ATB-CP1 and DIR-ATB-CP2 micelles remained accumulated at the tumor site.
Biodistribution of 1,1′-dioctadecyl-3,3,3′,3′-tetramethylindotricarbocyanine iodide (DIR)-labeled formulations after intravenous (iv) injection in mice. (A) Real-time in vivo fluorescence images of mice after iv injection of free DIR, DIR labeled acetylthevetin B (ATB) solution (DIR-ATB), DIR-labeled CP1 (DIR-ATB-CP1), and DIR-labeled CP2 (DIR-ATB-CP2) (lex= 745 nm; lem=800 nm). (B) Fluorescence images of organs excised at 6 h post injection; Biodistribution of DIR-labeled formulations in tumor (C), lung (D), and heart (E) excised from mice at 6 h post injection. The error is the standard deviation from the mean. n=3. *P<0.05, **P<0.01.
For a more accurate measurement, major internal organs (heart, liver, spleen, lung, and kidney) were removed at 6 h post injection and analyzed directly using a fluorescent imager (Figure 4B). The mean fluorescent intensity concentration of DIR-ATB-CP1 micelles (14.24×109/g) in the A549 solid tumor increased approximately 15.31-fold compared with the free ATB solution (0.93×109/g) and 2.24-fold compared with DIR-ATB-CP2 micelles (6.36×109/g). However, the distribution in the lungs requires further attention, as this distribution reflects the organ selectivity of the formulations. DIR-ATB-CP1 micelles (30.75×109/g) showed a 9.49-fold increase in fluorescent intensity compared to the free ATB solution (3.24×109/g) in the lungs. The fluorescent intensity of DIR-ATB-CP1 micelles in the lungs was 2.21-fold higher than that of DIR-ATB-CP2 micelles. Importantly, the distribution of DIR-ATB-CP1 micelles in the heart (1.32×109/g) was significantly less than that of free ATB (4.39×109/g, 3.33-fold) and DIR-ATB-CP2 micelles (2.48×109/g, 1.88-fold) (P<0.01).
Antitumor efficacy and toxicity of ATB-based formulations
The antitumor activity of free ATB, ATB-CP1, and ATB-CP2 was validated using the A549 xenograft tumor model in BALB/c nude mice. As shown in Figure 5A, the tumor volume of the control group exhibited linear growth in the later period indicating a high degree of malignancy. Compared with the control, tumor growth was inhibited in all the groups treated with ATB formulations. ATB-CP1 demonstrated the highest inhibitory effect on tumor growth compared to control, and the tumor volume significantly decreased from (436.48±34.93) mm3 to (106.5±9.79) mm3 (4.10-fold decrease compared to the control group). In addition, ATB-CP1 also showed the lowest tumor volume compared with free ATB solution and ATB-CP2 micelles. The pictures of the tumors from each group are shown in Figure 5D, and the tumor volume of the ATB-CP1 group was the smallest among the treatment groups. In addition, the tumor weight at the end of the experiment showed the same trend. The inhibition rates for free ATB solution, ATB-CP1, and ATB-CP2 were 43.8%, 85.6%, and 59.7%, respectively, compared to the control group. The ATB-CP1 group showed the lowest tumor weight and the highest inhibition rate among all treatment groups (Figure 5C).
Effect of intravenous (iv) injection of acetylthevetin B (ATB)-based formulations on tumor growth in BALB/c nude mice with A549 drug resistant xenograft tumors. (A) The average values of the relative rumor volume V/V0. Each data point represents the mean±SD of 6 different mice. **P<0.01, significantly different from the ATB or control injection group. (B) Body weights of the mice over the experimental period. n=6. (C) Tumor weight after 21 d of treatment with the ATB solution, ATB-CP1, or ATB-CP2. n=6. **P<0.01. (D) Tumor pictures of the mice treated with free ATB, ATB-CP1, and ATB-CP2. (E) Hematoxylin and eosin (H&E) stained tumor slices from mice on d 22 after treatments with saline, free ATB, ATB-CP1, and ATB-CP2. Images were obtained under Leica DMRE light microscopy using a 400× objective.
At the end of the experiment, the tumors were removed and sectioned for pathological analysis. Histological examination of the tumor tissues from each group further confirmed the successful destruction of tumor cells by ATB-CP1. As shown in Figure 5E, the tumor tissue treated with normal saline revealed malignancy. The nuclei of the cancer cells were large and oval-shaped, with increased chromatin and visible binucleolates. In contrast, tumor sections treated with ATB-CP1 clearly showed severe apoptosis across a large tumor area. In mice injected with ATB-CP2, tumor apoptosis was somewhat increased beyond that in ATB-treated mice, but this effect was not as significant as observed in mice treated with ATB-CP1. These findings suggested that ATB-CP1 exhibited the greatest therapeutic efficacy among all treatment groups.
After 21 d of treatment, the survival rates of each group were 100%. The body weight of mice is shown in Figure 6B, and no significant body weight loss was observed in mice injected with free ATB, ATB-CP1, and ATB-CP2 during the treatment. Based on the results of the QPatch™ assay of ATB toward the potassium channel, the cardiotoxicity of ATB was far less than that of cisapride (a positive control). However, the toxicity of ATB toward CHO-hERG cells indicated that this compound might cause weak cardiotoxicity because the inhibition rate of the ATB group was higher than that of digoxin (Table S1, S2). Histopathological evaluation was required to confirm the toxicity of ATB on rat hearts and other tissues. Representative pathological images of the hearts and other tissues are presented in Figure 6 and Figure S6, S7, S8, S9. Notably, after treatment for 21 d, no significant pathological changes were observed in the hearts and other main tissues in all treatment groups. These results suggest that all ATB-based formulations have relatively weak toxic effects on the heart and other main tissues.
Hematoxylin and eosin (H&E) stained heart slices from mice on day 22 after treatments with saline, free ATB, ATB-CP1, and ATB-CP2. Images were obtained under Leica DMRE light microscopy using a 400× objective.
Discussion
ATB is a typical CG containing a hydrophobic steroidal aglycone and hydrophilic glycosyl functionality, which confers its amphiphilic nature3,41,42. For the driving force of micellization, Pluronic copolymers consist of hydrophilic poly(ethylene oxide) (PEO) and hydrophobic poly(propylene oxide) (PPO) tri-block structures; thus, the driving force is the hydrophobic interaction between PPO blocks28. The particle sizes were correlated well with Pluronic-type micelles, whose average hydrodynamic diameter ranged from 20 to 80 nm43. For the in vitro cumulative release profiles of the ATB formulations, the steric protection effect of the PEO-PPO-PEO chain on the surface of micelles minimizes premature drug leakage, enabling the accumulation of drug molecules at the targeted site44.
In the cellular uptake study, the results indicated that the transportation of ATB across the A549 cell membrane can be markedly improved by CP1 micelles, and higher cellular accumulation of the drug will be reached. The cytotoxic studies suggested that all ATB formulations induced the arrest of cell growth at different levels, indicating that ATB has antitumor activity, with ATB-CP1 exhibiting superior efficacious S-phase arrest and a significant reduction in the G0/G1 phase. These findings demonstrated that CP1 micelles significantly improved the membrane transportation ability of ATB. Thus, the enhanced accumulation of cellular ATB played a pivotal role in enhancing cell cycle arrest, which is consistent with the in vitro cytotoxicity results.
Furthermore, we used an A549 xenograft tumor model in BALB/c nude mice to study the antitumor activity of ATB in vivo. The biodistribution study suggested that the distribution of ATB could be changed by CP1 micelles, and its distribution in solid tumors and the lungs could be largely improved through CP1. In addition, the decreased amount of CP1 in the heart indicated that the cardiac toxicity of ATB might be decreased to some extent. The prolonged tumor inhibition effect of ATB and its formulations was evaluated, and the results indicated that ATB-CP1 exhibited the strongest antitumor activity toward A549 solid tumors. The cellular uptake and distribution of ATB in tumor and lung tissues were enhanced by the affinity toward A549 cells and the EPR effect7,8 of micelles. The CP1 package also decreased the distribution of ATB in the heart, liver and spleen. Thus, the in vivo antitumor efficacy of ATB was markedly enhanced without significant toxicity in normal tissues. Previous studies have reported that the affinity of nanocarriers for cells or organs may attribute to their interaction with cell membranes30,31,32,33,34. Moreover, this effect is conducive for ATB to play a strong tumor curative effect in lung cancer.
The CP1 micelle, reflecting its strong affinity toward the A549 cell membrane, increased the intracellular ATB concentration to levels exceeding that of free ATB or the drug being delivered by the CP2 micelle. Moreover, ATB and its formulation ATB-CP1 were preliminarily confirmed to induce no significant damage to main organ tissues after 21 d of treatment. Studies on the long-term effects of ATB toward normal organs are still required. From a clinical viewpoint, ATB-CP1 exhibited high antitumor efficacy and low cytotoxicity in vivo and may serve as an antitumor formulation for the treatment of lung cancer.
In summary, we have successfully prepared CG formulations for the treatment of lung cancer. ATB was successfully loaded in a biofunctionalized polymeric micelle, and its antitumor activity and cytotoxicity were evaluated in vitro and in vivo. The ability of ATB to transport across the A549 cell membrane was improved by the CP1 micelle, leading to the increased cellular accumulation of the drug. In A549 cells, the antitumor efficacy of ATB was enhanced by the formulation. In A549 cell tumor-bearing mice, the results of the biodistribution study showed that the CP1 micelle could enhance the retention time and concentration of ATB in tumor tissue, and reduce its distribution in the heart. In the in vivo study, ATB-CP1, benefiting from the strong affinity of CP1 towards tumor cells, showed markedly improved therapeutic effects and no apparent side effects. Based on these findings, we anticipate the contribution of the CP1 micelle to the development of CGs in clinical applications. However, the total synthesis and specific anti-tumor mechanism of ATB should be further studied for the future application of this compound.
Author contribution
Jing-jing ZHU performed most of the experiments and drafted the manuscript. Xin-xin ZHANG modified the technical aspects of the manuscript. Yun-qiu MIAO assisted in the cell culture experiments. Shu-fang HE assisted in the analysis of the cell culture results. Dan-mei TIAN and Xin-sheng YAO assisted in the extraction, isolation and characterization of ATB. Xin-xin ZHANG, Jin-shan TANG, and Yong GAN designed and directed the study and participated in the overall editing and approval of the paper. All authors reviewed the manuscript.
Supplementary information
The chemical structure of ATB, HRESIMS, 1H and 13C NMR spectra, signal assignment of ATB, and other information are provided in the supporting information at the website of Acta Pharmacologica Sinica.
Change history
21 February 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Prassas I, Diamandis EP . Novel therapeutic applications of cardiac glycosides. Nat Rev Drug Discov 2008; 7: 926–35.
Newman RA, Yang PY, Pawlus AD, Block KI . Cardiac glycosides as novel cancer therapeutic agents. Mol Interv 2008; 8: 36–49.
Haux J . Digitoxin is a potential anticancer agent for several types of cancer. Med Hypotheses 1999; 53: 543–8.
Zhang HY, Xu WQ, Wang YW, Omari-Siaw E, Wang Y, Zheng YY, et al. Tumor targeted delivery of octreotide-periplogenin conjugate: synthesis, in vitro and in vivo evaluation. Int J Pharm 2016; 502: 98–106.
Tian X, Yin H, Zhang S, Luo Y, Xu K, Ma P, et al. Bufalin loaded biotinylated chitosan nanoparticles: an efficient drug delivery system for targeted chemotherapy against breast carcinoma. Eur J Pharm Biopharm 2014; 87: 445–53.
Biswas S, Kumari P, Lakhani PM, Ghosh B . Recent advances in polymeric micelles for anti-cancer drug delivery. Eur J Pharm Sci 2016; 83: 184–202.
Wang X, Yang C, Zhang Y, Zhen X, Wu W, Jiang X . Delivery of platinum (IV) drug to subcutaneous tumor and lung metastasis using bradykinin-potentiating peptide-decorated chitosan nanoparticles. Biomaterials 2014; 35: 6439–53.
Liu J, Jiang ZZ, Zhang SM, Saltzman WM . Poly(omega-pentadecalactone-co-butylene-co-succinate) nanoparticles as biodegradable carriers for camptothecin delivery. Biomaterials 2009; 30: 5707–19.
Tian DM, Cheng HY, Jiang MM, Shen WZ, Tang JS, Yao XS . Cardiac glycosides from the seeds of Thevetia peruviana. J Nat Prod 2016; 79: 38–50.
Sadhukha T, O'Brien TD, Prabha S . Nano-engineered mesenchymal stem cells as targeted therapeutic carriers. J Control Release 2014; 196: 243–51.
Naguib YW, Rodriguez BL, Li X, Hursting SD, Williams RO 3rd, Cui Z . Solid lipid nanoparticle formulations of docetaxel prepared with high melting point triglycerides: in vitro and in vivo evaluation. Mol Pharm 2014; 11: 1239–49.
Ganesh S, Iyer AK, Morrissey DV, Amiji MM . Hyaluronic acid based self-assembling nanosystems for CD44 target mediated siRNA delivery to solid tumors. Biomaterials 2013; 34: 3489–502.
Ganesh S, Iyer AK, Gattacceca F, Morrissey DV, Amiji MM . In vivo biodistribution of siRNA and cisplatin administered using CD44-targeted hyaluronic acid nanoparticles. J Control Release 2013; 172: 699–706.
Karra N, Nassar T, Ripin AN, Schwob O, Borlak J, Benita S . Antibody conjugated PLGA nanoparticles for targeted delivery of paclitaxel palmitate: efficacy and biofate in a lung cancer mouse model. Small 2013; 9: 4221–36.
Haisung L, Dong Kee Y . A study of Gd loaded silica nanoparticles for both optical and magnetic resonance imaging of cells. Mater Lett 2013; 100: 98–101.
Tobin LA, Xie Y, Tsokos M, Chung SI, Merz AA, Arnold MA, et al. Pegylated siRNA-loaded calcium phosphate nanoparticle-driven amplification of cancer cell internalization in vivo. Biomaterials 2013; 34: 2980–90.
Ruiz A, Hernandez Y, Cabal C, Gonzalez E, Veintemillas-Verdaguer S, Martinez E, et al. Biodistribution and pharmacokinetics of uniform magnetite nanoparticles chemically modified with polyethylene glycol. Nanoscale 2013; 5: 11400–8.
Ruiz A, Salas G, Calero M, Hernandez Y, Villanueva A, Herranz F, et al. Short-chain PEG molecules strongly bound to magnetic nanoparticle for MRI long circulating agents. Acta Biomater 2013; 9: 6421–30.
Zhang XX, Guo SY, Fan R, Yu MR, Li FF, Zhu CL, et al. Dual-functional liposome for tumor targeting and overcoming multidrug resistance in hepatocellular carcinoma cells. Biomaterials 2012; 33: 7103–14.
Wei PR, Cheng SH, Liao WN, Kao KC, Weng CF, Lee CH . Synthesis of chitosan-coated near-infrared layered double hydroxide nanoparticles for in vivo optical imaging. J Mater Chem 2012; 22: 5503–13.
Esmaeili F, Dinarvand R, Ghahremani MH, Ostad SN, Esmaily H, Atyabi F . Cellular cytotoxicity and in-vivo biodistribution of docetaxel poly(lactide-co-glycolide) nanoparticles. Anti-Cancer Drug 2010; 21: 43–52.
Hwang HY, Kim IS, Kwon IC, Kim YH . Tumor targetability and antitumor effect of docetaxel-loaded hydrophobically modified glycol chitosan nanoparticles. J Control Release 2008; 128: 23–31.
Ladet S, David L, Domard A . Multi-membrane hydrogels. Nature 2008; 452: 76–9.
Pavinatto FJ, Pavinatto A, Caseli L, dos Santos DS, Nobre TM, Zaniquelli MED, et al. Interaction of chitosan with cell membrane models at the air-water interface. Biomacromolecules 2007; 8: 1633–40.
Khor E, Lim LY . Implantable applications of chitin and chitosan. Biomaterials 2003; 24: 2339–49.
Huang M, Ma Z, Khor E, Lim LY . Uptake of FITC-chitosan nanoparticles by A549 cells. Pharm Res 2002; 19: 1488–94.
Otsuka H, Nagasaki Y, Kataoka K . PEGylated nanoparticles for biological and pharmaceutical applications. Adv Drug Deliver Rev 2012; 64: 246–55.
Kabanov AV, Lemieux P, Vinogradov S, Alakhov V . Pluronic block copolymers: novel functional molecules for gene therapy. Adv Drug Deliv Rev 2002; 54: 223–33.
Barreto JA, O'Malley W, Kubeil M, Graham B, Stephan H, Spiccia L . Nanomaterials: applications in cancer imaging and therapy. Adv Mater 2011; 23: H18–40.
Pelaz B, del Pino P, Maffre P, Hartmann R, Gallego M, Rivera-Fernandez S, et al. Surface functionalization of nanoparticles with polyethylene glycol: effects on protein adsorption and cellular uptake. ACS Nano 2015; 9: 6996–7008.
Dai Q, Walkey C, Chan WCW . Polyethylene glycol backfilling mitigates the negative impact of the protein corona on nanoparticle cell targeting. Angew Chem Int Edit 2014; 53: 5093–6.
Treuel L, Brandholt S, Maffre P, Wiegele S, Shang L, Nienhaus GU . Impact of protein modification on the protein corona on nanoparticles and nanoparticle-cell interactions. ACS Nano 2014; 8: 503–13.
Torrisi V, Graillot A, Vitorazi L, Crouzet Q, Marletta G, Loubat C, et al. Preventing corona effects: multiphosphonic acid poly(ethylene glycol) copolymers for stable stealth iron oxide nanoparticles. Biomacromolecules 2014; 15: 3171–9.
Walkey CD, Olsen JB, Guo H, Emili A, Chan WC . Nanoparticle size and surface chemistry determine serum protein adsorption and macrophage uptake. J Am Chem Soc 2012; 134: 2139–47.
Zhuang CY, Li N, Wang M, Zhang XN, Pan WS, Peng JJ, et al. Preparation and characterization of vinpocetine loaded nanostructured lipid carriers (NLC) for improved oral bioavailability. Int J Pharm 2010; 394: 179–85.
Rudra A, Deepa RM, Ghosh MK, Ghosh S, Mukherjee B . Doxorubicin-loaded phosphatidylethanolamine-conjugated nanoliposomes: in vitro characterization and their accumulation in liver, kidneys, and lungs in rats. Int J Nanomed 2010; 5: 811–23.
Morgan NY, English S, Chen W, Chernomordik V, Russo A, Smith PD, et al. Real time in vivo non-invasive optical imaging using near-infrared fluorescent quantum dots 1. Acad Radiol 2005; 12: 313–23.
Christian DA, Garbuzenko OB, Minko T, Discher DE . Polymer vesicles with a red cell-like surface charge: microvascular imaging and in vivo tracking with near-infrared fluorescence. Macromol Rapid Comm 2010; 31: 135–41.
Michaelis M, Zimmer A, Handjou N, Cinatl J, Cinatl J . Increased systemic efficacy of aphidicolin encapsulated in liposomes. Oncol Rep 2005; 13: 157–60.
Lo A, Lin CT, Wu HC . Hepatocellular carcinoma cell-specific peptide ligand for targeted drug delivery. Mol Cancer Ther 2008; 7: 579–89.
McConkey DJ, Lin Y, Nutt LK, Ozel HZ, Newman RA . Cardiac glycosides stimulate Ca2+ increases and apoptosis in androgen-independent, metastatic human prostate adenocarcinoma cells. Cancer Res 2000; 60: 3807–12.
Yeh JY, Huang WJ, Kan SF, Wang PS . Inhibitory effects of digitalis on the proliferation of androgen dependent and independent prostate cancer cells. J Urol 2001; 166: 1937–42.
Nagarajan R . Solubilization of hydrocarbons and resulting aggregate shape transitions in aqueous solutions of Pluronic (R) (PEO-PPO-PEO) block copolymers. Colloid Surface B 1999; 16: 55–72.
Alvarez-Lorenzo C, Sosnik A, Concheiro A . PEO-PPO block copolymers for passive micellar targeting and overcoming multidrug resistance in cancer therapy. Curr Drug Targets 2011; 12: 1112–30.
Acknowledgements
Financial support was obtained from the National Natural Science Foundation of China (No 81571796, 81673320), the Youth Innovation Promotion Association (No 2015229), the SA-SIBS Scholarship Program, and the State Key Laboratory of Drug Research (No SIMM1403KF-15 and SIMM1601KF-09). The authors would like to thank Dr Zhuang WEI for generously providing lung carcinoma A549 cells.
Author information
Authors and Affiliations
Corresponding authors
Supplementary information
Supplementary Figure S1
The structure of acetylthevetin B (ATB) (DOC 149 kb)
Supplementary Figure S2
The HRESIMS spectrum of ATB (DOC 80 kb)
Supplementary Figure S3
The 1H NMR (400 MHz, pyridine-d6) spectrum of ATB (DOC 108 kb)
Supplementary Figure S4
The 13C NMR (100 MHz, pyridine-d6) spectrum of ATB (DOC 99 kb)
Supplementary Figure S5
The 13C and DEPT 135 NMR (100 MHz, pyridine-d6) spectra of ATB (DOC 137 kb)
Supplementary Figure S6
Hematoxylin and eosin (H&E) stained liver slices from mice on Day 22 after treatments with saline, free ATB, ATB-CP1, ATB-CP2. (DOC 11039 kb)
Supplementary Figure S7
Hematoxylin and eosin (H&E) stained spleen slices from mice on Day 22 after treatments with saline, free ATB, ATB-CP1, ATB-CP2. (DOC 10208 kb)
Supplementary Figure S8
Hematoxylin and eosin (H&E) stained lung slices from mice on Day 22 after treatments with saline, free ATB, ATB-CP1, ATB-CP2. (DOC 6959 kb)
Supplementary Figure S9
Hematoxylin and eosin (H&E) stained kidney slices from mice on Day 22 after treatments with saline, free ATB, ATB-CP1, ATB-CP2. (DOC 10204 kb)
Supplementary Table S1
The inhibited effect of ATB and Digoxin towards hERG potassium current (DOC 532 kb)
Supplementary Table S2
The toxicity of ATB and Digoxin towards CHO-hERG cells (DOC 42 kb)
Rights and permissions
About this article
Cite this article
Zhu, Jj., Zhang, Xx., Miao, Yq. et al. Delivery of acetylthevetin B, an antitumor cardiac glycoside, using polymeric micelles for enhanced therapeutic efficacy against lung cancer cells. Acta Pharmacol Sin 38, 290–300 (2017). https://doi.org/10.1038/aps.2016.113
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2016.113
Keywords
This article is cited by
-
Applications and advancements of nanoparticle-based drug delivery in alleviating lung cancer and chronic obstructive pulmonary disease
Naunyn-Schmiedeberg's Archives of Pharmacology (2023)
-
Treating breast cancer metastasis with cabazitaxel-loaded polymeric micelles
Acta Pharmacologica Sinica (2017)
-
Co-delivery of docetaxel and silibinin using pH-sensitive micelles improves therapy of metastatic breast cancer
Acta Pharmacologica Sinica (2017)