Abstract
Aim:
To investigate the pharmacokinetics and dopamine/acetylcholine-releasing effects of ginsenoside Re (Re) in brain regions related to learning and memory, and to clarify the neurochemical mechanisms underlying its anti-dementia activity.
Methods:
Microdialysis was conducted on awake, freely moving adult male SD rats with dialysis probes implanted into the hippocampus, medial prefrontal cortex (mPFC) or the third ventricle. The concentrations of Re, dopamine (DA) and acetylcholine (ACh) in dialysates were determined using LC-MS/MS.
Results:
Subcutaneous administration of a single dose of Re (12.5, 25 or 50 mg/kg) rapidly distributed to the cerebrospinal fluid and exhibited linear pharmacokinetics. The peak concentration (Cmax) occurred at 60 min for all doses. Re was not detectable after 240 min in the dialysates for the low dose of 12.5 mg/kg. At the same time, Re dose-dependently increased extracellular levels of DA and ACh in the hippocampus and mPFC, and more prominent effects were observed in the hippocampus.
Conclusion:
The combined study of the pharmacokinetics and pharmacodynamics of Re demonstrate that increase of extracellular levels of DA and ACh, particularly in the hippocampus, may contribute, at least in part, to the anti-dementia activity of Re.
Similar content being viewed by others
Introduction
Alzheimer's disease (AD) is the main cause of dementia and cognitive dysfunction among the elderly and is becoming a major threat to human health. The pathogenesis of AD involves multiple mechanisms that still have not been clarified. An imbalance of different neurotransmitters, such as acetylcholine, dopamine, glutamate and serotonin, has been proposed as the neurobiological basis of the behavioral symptoms in AD1,2. The central cholinergic pathways play a prominent role in memory processes3,4, and it is generally accepted that progressive neurodegeneration of the cholinergic system underlies, at least in part, the cognitive deterioration caused by AD5,6,7. Acetylcholinesterase (AChE) inhibition is considered one of the most important approaches to therapy, due to the enhancement of acetylcholine (ACh) levels in brain8,9. The dopaminergic system has also been found to be impaired in AD10,11. Shu et al12 found that AD patients have significantly decreased levels of dopamine (DA) in six cortical regions, including the frontal and temporal lobes. It has been reported that selective activation of D1/D5 receptors could protect synapses in AD. An association has also been observed between D2 receptor availability in the right hippocampus and cognitive performance in AD13,14.
The central nervous system (CNS) pharmacokinetics (PK) of a drug are important determinants in the time course and intensity of its effects, if the action compartment of which is in CNS. Understanding how different drugs are metabolized in the brain is important because it can provide valuable insights pertaining to the pharmacological activities of a drug. Thus, the combined study of PK and pharmacodynamics (PD) is of growing importance in the evaluation of drugs acting on CNS targets15,16.
To date, therapeutic drugs intended to remedy neurotransmitter deficits have been studied extensively17,18,19. Ginseng, the root of Panax ginseng C A Meyer (Araliaceae), has been used as a nootropic and anti-aging agent for more than 2000 years in China, and it is widely used as a medicinal supplement in Asia, Europe and the United States20. Among the complex constituents of ginseng, ginsenosides are the major components responsible for its biochemical and pharmacological actions, which include the regulation of neurotransmitters relevant to dementia17,21,22,23,24. Ginsenoside Re (Re), one of the six major ginsenosides, comprises greater than 70% of the total ginsenoside content25. Re, Rg1, and protopanaxatriol (PPT) belong to the same group of ginsenosides26. It has been confirmed that Re has improved cognitive function in several rat models of memory impairment, as well as in natural aging and streptozotocin-induced diabetic models21,22,27. The inhibition of AChE activity and the promotion of long-term potentiation are believed to underlie these effects. However, several questions remain. What are the underlying neurobiochemical mechanisms of the anti-dementia effects of Re? Does Re display direct activity on the neurotransmitters relevant to dementia, and can Re pass through the brain-blood barrier (BBB)? What is the relationship between the PK and PD of Re in its target regions? Our study focuses on these questions.
We investigated the intracerebral PK of Re in the present study, as well as the effects of acute administration of Re on DA and ACh release in the mPFC and HIP, which are target regions for the treatment of AD. The relationship between the PK and PD for Re was also explored. For these purposes, the present study was carried out by in vivo microdialysis on freely moving rats following the administration of Re using HPLC-ECD and LC-MS/MS.
Materials and methods
Animals and treatment protocol
Adults male Sprague Dawley rats (Taconic) were obtained from Vital River Laboratories (Beijing, China) and weighed 230–250 g at the start of the experiment. The rats were housed in groups of two in plastic wire mesh cages (50 cm×30 cm×18 cm) in the animal house. They were maintained in a temperature controlled environment with a 12:12 h light/dark cycle and continuous access to food and water. Re was injected once, subcutaneously, in a volume of 1 mL/kg saline at doses of 50, 25, or 12.5 mg/kg. The control group received the same volume of saline alone. The animals used in this study were cared for in accordance with internationally accepted principles for laboratory animal use and care (NIH publication No 86–23, revised 1985).
Drugs and reagents
Re (98.5% purity) was obtained from Beijing Xinliheng Pharmaceutical Technology Development Co, Ltd. Digoxin [internal standard (IS)], DA standard and d9-ACh were purchased from Sigma (USA). HPLC-grade methanol, methanoic acid, ethanoic acid, isopropanol and acetonitrile were all from Tedia (Fairfield, USA). Water was purified with a Milli-Q system (Millipore, France).
Surgery and microdialysis
Microdialysis experiments were conducted according to the procedures outlined by Li et al26. Briefly, the rats were anesthetized with sodium pentobarbital (50 mg/kg, ip) and placed in a stereotaxic frame (RWD Life Science, China). Stainless steel guide cannulas with dummy probes were implanted according to the methods described by Paxinos and Watson (1998). The rats received cannula implantations for the mPFC [AP=−3.2 mm; L=1.4 mm (10° inclination); DV=−1.2 mm from the bregma], HIP (AP=5.6 mm; L=5.0 mm; DV=−5.2 mm from the bregma), or the third ventricle (AP=4.5 mm; L=−2.4 mm (18° inclination); DV=−5.7 mm from the bregma). The implanted cannulas were anchored by two screws driven into the skull and fixed by dental acrylic cement.
On the second or third day after cannulation, dialysis probes were implanted into the mPFC, HIP or the third ventricle, and a thin tube with incisions was embedded under the skin on the back while the animals were administered slight anesthesia with diethyl ether. The rats were housed individually overnight in a dialysis cage, and the probes were perfused with artificial cerebrospinal fluid (Dulbecco's: 138 mmol/L NaCl, 8.1 mmol/L Na2HPO4, 2.7 mmol/L KCl, 1.5 mmol/L KH2PO4, 0.5 mmol/L MgCl2, and 1.2 mmol/L CaCl2 without cholinesterase inhibitor) at 0.4 μL/min overnight.
On the experimental days, the perfusion rates were increased to 1.5 μL/min. After 1 h of equilibration, dialysates were collected in polyethylene vials every 30 min throughout the experiments. The first three samples obtained from the mPFC or HIP before administration were used to establish the baseline values of DA or ACh (samples from −60, and −30 min), and the first two samples from the third ventricle (samples from −60 and −30 min) were used to establish the baseline levels of Re in the brain prior to its administration. Subsequently, the rats received one subcutaneous injection of drug or vehicle. The samples collected from 0 to 210 min in the mPFC or HIP were used for neurotransmitter analysis, and the dialysates of cerebrospinal fluid from 0 to 360 min were analyzed to describe the pharmacokinetics of Re in the brain. The locations of the dialysis probes were verified at the end of each experiment by brain dissection.
Ginsenoside Re detection in brain microdialysis samples
The analytical method for Re detection was developed based on Liu's study27.
Liquid chromatographic conditions
The LC-MS/MS system consisted of a Waters auto-sampler, a Waters 2795 LC pump, a Quattro premier triple-quadrupole mass spectrometer and a Waters MassLynx™ 4.0 workstation (Waters, USA). Chromatographic separations were performed using a Waters Symmetry C18 Column (2.1 mm×50 mm, 3.5 μm), the temperature of which was maintained at 22 °C. An injection volume (20 μL) of sample was kept in an auto sampler at 4 °C. Separation of the analytes was achieved using a gradient elution (0.05% methanoic acid-water-acetonitrile, each organic phase containing 0.05% ethanoic acid) at a flow rate of 0.3 mL/min with continuous 5% acetonitrile and a linear gradient of 12%–85% methanol for 2 min, 85% methanol for 2 min, and 12% methanol for 4 min. The retention time (Table 1) was approximately 2.82 min for Re and 3.10 min for the internal standard (IS).
Mass spectrometric conditions
The positive ionization mode in electrospray MS/MS was chosen, and data were acquired using multiple reaction monitoring (MRM) incorporating a molecular weight scan from m/z 100 to 1100. The electrospray MS/MS parameters were applied as follows: electrospray capillary voltage was 3.5 kV; ultrapure nitrogen (500 L/h) was used as the nebulizer; cone gas was administered at a rate of 50 L/h; and source and desolvation temperatures were set at 105 and 350 °C, respectively. With the collision energy off, the analytes yielded predominantly [M+Na]+ for Re and protonated molecular ions for the IS. Each of the precursor ions was subjected to collision-induced dissociation (CID) to determine the resulting daughter ions. Argon was used as the collision gas at a flow rate of 0.24 mL/min. The acquired data were quantified using Masslynx 4.0 (Waters Corp, USA). The monitor ion and collision energy are shown in Table 1.
Biochemical assay
Sample preparation
The dialysate sample (10 μL) was transferred to a 200 μL microtube, and 5 μL DA stabilizing agent (10% methanoic acid) was added. Then, the sample was vortex mixed for 30 s and prepared for DA detection. The dialysate sample (20 μL) was transferred to a 96-well plate, added to 5 nmol/L ACh-d9 in 50 μL diluent (isopropanol:acetonitrile 4:6, 0.1% methanoic acid), vortexed for 30 s and prepared for ACh detection.
Determination of DA26,28,29
The pH-adjusted supernatant (20 μL) was directly applied to a high-performance liquid chromatography system (10AD, SHIMADZU, Japan) with an electrochemical detector (5200A Coulochem II, ESA, USA) and analyzed with a CLASS-VP workstation (SHIMADZU, Japan). DA was separated on an analytical reverse phase column (Atlantis™ HILIC Silica, 2.1×100 mm, 3 μm, Waters, USA). The mobile phase (75 mmol/L sodium acetate trihydrate, 24 mmol/L citric acid, 1.2 mmol/L sodium dodecyl sulfate, 0.5 mmol/L EDTA-2Na, 10 mol/L NaOH, pH=5.4) was degassed (Eicom DG-300) and pumped at a flow rate of 0.3 mL/min.
Determination of ACh30,31
A liquid chromatography-tandem mass spectrometry method has been developed and validated for the determination of ACh in rat brain dialysate sampling by microdialysis. The LC–MS/MS analysis system was described above. The separation of ACh was carried out using a Symmetry C18 column (50 mm×2.10 mm, 3.50 μm, Waters, USA) which was maintained at 25 °C. The mobile phase consisted of 200 mmol/L ammonium formate in water, CH3CN and water (4:75:21) for 2.82 min with a flow rate of 0.30 mL/min. The injection volume was 20 μL.
The eluates were detected using a triple-quadrupole mass spectrometer equipped with an electrospray ionization (ESI) source at 105 °C. Nitrogen was used as sheath gas and auxiliary gas and was delivered at 45 psi and 2 L/min, respectively. The capillary temperature was 400 °C. The collision gas, argon, had a flow rate of 0.24 mL/min. The analysis was carried out using selected reaction monitoring mode that was set to detect a specific transition for ACh (m/z 146→87) and IS (d9-ACh m/z 155→87).
Statistical analysis
The average baseline levels of DA or ACh (time points of −60, −30, and 0 min) were designated as 100%, and the ratio of the concentration of each sample to the average baseline levels was calculated. The levels of DA and ACh were analyzed using the repeated measures analysis of variance (ANOVA) procedure of the general linear model (SPSS 16.0). Fisher's protected least significant difference post hoc pairwise comparison was used to determine group differences. Percentage of AUC (pAUC), represented the changes of the neurotransmitters affected by Re, was analyzed by one-way ANOVA. A probability P<0.05 was considered significant. All results are given as the mean±SD.
Pharmacokinetic parameters of Re in dialysate samples were determined using Drug and Statistics for Windows software (DAS Version 2.0). Drug concentrations below the LLOQ were deemed to be zero.
Results
Pharmacokinetics of Re in the brain
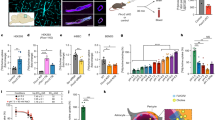
After subcutaneous administration, Re was detected in CSF dialysates. The peak concentration (Cmax) occurred at 60 min for all doses (Figure 1). Re was not detectable after 240 min in the dialysates of the 12.5 mg/kg group. The pharmacokinetic parameters of Re were calculated using the DAS software and are shown in Table 2.
The concentration-time curve of ginsenoside Re in dialysates of cerebrospinal fluid. Re at dose of 12.5, 25, and 50 mg/kg was subcutaneously injected to rats at 0 min, and the dialysates collected at from −30 min to 360 min were detected of Re using LC-MS/MS. Data are Mean±SD (n=3) of the concentration of Re in CSF.
The baseline levels of DA and ACh in the mPFC and HIP
Basal extracellular DA levels were 1.89±1.90 (fmol/10 μL) and 3.90±2.77 (fmol/10 μL) in the dialysates obtained from the mPFC and HIP, respectively. The basal extracellular ACh levels were 1.80±0.54 (fmol/10 μL) and 4.16±0.60 (fmol/10 μL) in the mPFC and HIP, respectively.
The effects of Re on DA in the mPFC and HIP
As shown in Figure 2A, dose-dependent increases in extracellular DA concentrations were detected in the mPFC after Re 12.5, 25, and 50 mg/kg was given (F(1,8)=107.156, P<0.0001; F(1,9)=626.494, P<0.0001; F(1,8)=1259, P<0.0001, respectively). The maximum increments were 24.08%±3.93% (12.5 mg/kg, n=5), 55.48%±2.70% (25 mg/kg, n=6), and 65.44%±4.82% (50 mg/kg, n=5) compared to the control group.
Time-course effects of ginsenoside Re (12.5, 25, and 50 mg/kg, sc) on extracellular dopamine in the mPFC (A) and in the HIP (B). The arrows indicate drug injection times. Each sample was collected at a flow rate of 1.5 μL/min for 30 min. Data are Mean±SD (n=5−6) of the dialysate dopamine levels, expressed as a percentage of each predrug baseline dopamine value.
As shown in Figure 2B, after subcutaneous injection of ginsenoside Re at 12.5, 25, and 50 mg/kg, extracellular DA concentrations in the HIP were also significantly increased in a dose-dependent manner [F(1,8)=191.739, P<0.0001; F(1,9)=1556, P<0.0001; F(1,8)=746.091, P<0.0001, respectively]. The maximum increments were 28.73%±1.48% (12.5 mg/kg, n=5), 63.05%±2.82% (25 mg/kg, n=6), and 64.76%±1.51% (50 mg/kg, n=5), respectively, compared to the control group.
The effect of Re on ACh in the mPFC and HIP
Ginsenoside Re (12.5, 25, and 50 mg/kg, sc) also dose-dependently increased extracellular ACh concentrations in the mPFC [F(1,8)=21.866, P=0.002; F(1,8)=90.542, P<0.0001; F(1,8)=99.488, P<0.0001, respectively]. The maximum increments were 32.98%±9.25% (12.5 mg/kg, n=5), 58.994%±0.92% (25 mg/kg, n=6), and 80.86%±8.80% (50 mg/kg, n=5), respectively, compared to the control group (Figure 3A).
Time-course effects of ginsenoside Re (12.5, 25, and 50 mg/kg, sc) on extracellular acetylcholine in the mPFC (A) and in the HIP (B). The arrows indicate drug injection times. Each sample was collected at a flow rate of 1.5 μL/min for 30 min. Data are Means±SD (n=5) of the dialysate acetylcholine levels, expressed as a percentage of each predrug baseline acetylcholine value.
Release of ACh was also increased by Re (12.5, 25, and 50 mg/kg, sc) in the HIP [F(1,8)=359.054, P<0.0001; F(1,9)=162.954, P<0.0001; F(1,8)=153.966, P<0.0001, respectively]. The maximum increments were 34.89%±0.28% (12.5 mg/kg, n=5), 64.70%±1.04% (25 mg/kg, n=6), 89.27%±1.51% (50 mg/kg, n=5), respectively, compared to the control group (Figure 3B).
Comparison of the effects of Re on extracellular DA or ACh levels in the mPFC and HIP
Percentage of AUC was used to assess the effect of Re on DA and ACh levels in the mPFC and HIP. As shown in Figure 4A, Re (50 mg/kg, sc) had stronger effects on the release of ACh in the HIP than in the mPFC (P<0.05, compared with ACh levels in the mPFC). The same trends were observed for DA levels (Figure 4B), though the differences were not statistically significant.
Discussion
Ginsenoside Re has recently been studied extensively; however, the metabolic and pharmacokinetic profiles of this compound have not yet been completely described22. The rapid absorption and low bioavailability of Re in rats have been reported in preclinical studies. Liu et al report that Rg1, F1, Rh1, and PPT are metabolites of Re that can be detected in the plasma and urine of healthy subjects after oral administration27. However, as a nootropic agent, nothing is known about the pharmacokinetic characteristics of Re in brain, which is deemed to be the target region for its action that affects cognitive processes. No evidence has been reported previously on whether Re and other ginsenosides cross the BBB. In this study, Re was detected in CSF dialysate soon after subcutaneous administration and reached peak CSF concentrations in 60 min. Both the AUC and Cmax increased proportionally with dose. These results suggest that Re can rapidly pass through the BBB and that the kinetic parameters show linear features in the brain. Thus, we report that Re can transverse the BBB and that its PK parameters in the brain provide evidence for the pharmacological actions of Re on the CNS. Whether the metabolites of Re can traverse the BBB and whether they are also involved in its pharmacological actions are important issues we will continue to explore32.
Re has proved to have potential as a cognition enhancer, but the mechanisms underlying its cognitive effects remain unclear. It is well known that the levels of extracellular neurotransmitters in the brain are closely related to cognitive function, especially DA and ACh, which play key roles in the regulation of cognitive processes33,34,35. Therefore, in this study, we chose these two crucial neurotransmitters and two regions believed to play major roles in learning and memory to investigate intracerebral evidence for the potential anti-dementia activity of Re on neurotransmitter levels. The present study indicates that Re (12.5, 25, and 50 mg/kg, sc) can dose-dependently increase levels of DA and ACh in the mPFC and HIP 30 to 90 min after administration and that these effects gradually decline after 90 min. The changes in DA and ACh levels in selected brain areas after acute administration of Re may contribute to its anti-dementia actions. In addition, high-dose Re exhibited a stronger effect on the release of ACh in the HIP than in the mPFC. A similar trend was evident for DA levels, though there was no statistically significant difference. These results indicate that Re has a selective mode of action on the HIP.
According to the results of the CNS PK and PD studies, dose-dependent features are observed in both PK and PD of Re, suggesting a relationship between effect compartment concentrations and observed effects. However, the maximal effect of Re occurs after tmax; this hysteresis suggests the possibility that metabolites of Re participate in or dominate the pharmacological actions. Accordingly, we infer a relationship between the pharmacokinetics of Re in CSF and its effects on neurotransmitters. However, further studies on PK/PD modeling and the metabolic products of Re are necessary.
We chose the subcutaneous route of drug administration to clarify the direct effects of Re on neurotransmitters and to minimize irritation to the animals. However, this method of administration is not typical, as it bypasses the issue of bioavailability. It has been reported that the absolute bioavailability of Re is only 7.06% in rats32 and 0.19%–0.28% in mice36. This poor bioavailability is possibly due to biotransformation to Rh1 and G-F1 by intestinal microflora before absorption into the blood37. Consequently, if Re is administered orally, most of it will be degraded in the gastrointestinal tract and only a small portion will be absorbed into the blood plasma. Thus, the activity of Re in brain may be weakened or insignificant as a result of oral administration. At the same time, the metabolites of Re in the gastrointestinal tract may represent the actual cause of its systematic effects. So there is a possibility that the metabolites of Re are involved in its effects on neurotransmitter levels. However, further exploration is needed to determine whether metabolites in the gastrointestinal tract can be reabsorbed into the plasma, pass through the BBB and affect the brain. In subsequent research, we intend to compare intracerebral PD using the oral and subcutaneous routes of administration. The influence of bioavailability on intracerebral PD may then be apparent.
In conclusion, after subcutaneous administration ginsenoside Re passes through the BBB, it shows linear characteristics of PK in brain and influences cognitive mechanisms by inducing the release of DA and ACh in specific brain regions.
Author contribution
Jing SHI and Wei XUE performed the research and wrote the manuscript. Wen-jie ZHAO prepared the compounds. Ke-xin LI designed the research and revised the paper.
References
Lanari A, Amenta F, Silvestrelli G, Tomassoni D, Parnetti L . Neurotransmitter deficits in behavioural and psychological symptoms of Alzheimer's disease. Mech Ageing Dev 2006; 127: 158–65.
Chen KH, Reese EA, Kim HW, Rapoport SI, Rao JS . Disturbed neurotransmitter transporter expression in Alzheimer's disease brain. J Alzheimers Dis 2011; 26: 755–66.
Winkler J, Suhr ST, Gage FH, Thal LJ, Fisher LJ . Essential role of neocortical acetylcholine in spatial memory. Nature 1995; 375: 484–7.
Wallace TL, Porter RH . Targeting the nicotinic alpha7 acetylcholine receptor to enhance cognition in disease. Biochem Pharmacol 2011; 82: 891–903.
Davies P, Maloney AJ . Selective loss of central cholinergic neurons in Alzheimer's disease. Lancet 1976; 2: 1403.
Whitehouse PJ, Price DL, Clark AW, Coyle JT, DeLong MR . Alzheimer disease: evidence for selective loss of cholinergic neurons in the nucleus basalis. Ann Neurol 1981; 10: 122–6.
Wallace TL, Ballard TM, Pouzet B, Riedel WJ, Wettstein JG . Drug targets for cognitive enhancement in neuropsychiatric disorders. Pharmacol Biochem Behav 2011; 99: 130–45.
Sugimoto H . The new approach in development of anti-Alzheimer's disease drugs via the cholinergic hypothesis. Chem Biol Interact 2008; 175: 204–8.
Pohanka M . Cholinesterases, a target of pharmacology and toxicology. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2011; 155: 219–29.
Aalto S, Bruck A, Laine M, Nagren K, Rinne JO . Frontal and temporal dopamine release during working memory and attention tasks in healthy humans: a positron emission tomography study using the high-affinity dopamine D2 receptor ligand [11C]FLB 457. J Neurosci 2005; 25: 2471–7.
Rinne JO, Sako E, Paljarvi L, Molsa PK, Rinne UK . Brain dopamine D-2 receptors in senile dementia. J Neural Transm 1986; 65: 51–62.
Shu SY, Bao X, Li S, Niu D, Xu Z, Li Y . A new subdivision of mammalian neostriatum with functional implications to learning and memory. J Neurosci Res 1999; 58: 242–53.
Jurgensen S, Antonio LL, Mussi GE, Brito-Moreira J, Bomfim TR, De Felice FG, et al. Activation of D1/D5 dopamine receptors protects neurons from synapse dysfunction induced by amyloid-beta oligomers. J Biol Chem 2011; 286: 3270–6.
Kemppainen N, Laine M, Laakso MP, Kaasinen V, Nagren K, Vahlberg T, et al. Hippocampal dopamine D2 receptors correlate with memory functions in Alzheimer's disease. Eur J Neurosci 2003; 18: 149–54.
Raybon JJ, Boje KM . Pharmacokinetics and pharmacodynamics of gamma-hydroxybutyric acid during tolerance in rats: effects on extracellular dopamine. J Pharmacol Exp Ther 2007; 320: 1252–60.
Kielbasa W, Kalvass JC, Stratford R . Microdialysis evaluation of atomoxetine brain penetration and central nervous system pharmacokinetics in rats. Drug Metab Dispos 2009; 37: 137–42.
Zhu W, Hu H . A survey of TCM treatment for Alzheimer's disease. J Tradit Chin Med 2007; 27: 226–32.
Wu TY, Chen CP, Jinn TR . Traditional Chinese medicines and Alzheimer's disease. Taiwan J Obstet Gynecol 2011; 50: 131–5.
Howes MJ, Houghton PJ . Plants used in Chinese and Indian traditional medicine for improvement of memory and cognitive function. Pharmacol Biochem Behav 2003; 75: 513–27.
Helms S . Cancer prevention and therapeutics: Panax ginseng. Altern Med Rev 2004; 9: 259–74.
Zhao Y, Liu JP, Lu D, Zhao Y, Li PY . Improvement effect of ginsenoside Re on learning and memory abilities of natural apolexis eats and its mechanisms. Tradit Chin Drug Res Clin Pharm 2007; 18: 20–2.
Jiang HL, Yang Z, Meng Q, Hong T . Improvement and mechanism of ginsenoside Re on learning and memory deficts of mice. Chin Pharm Bull 2008; 24: 1399–40.
Li Z, Huang M, Ichikawa J, Dai J, Meltzer HY . N-desmethylclozapine, a major metabolite of clozapine, increases cortical acetylcholine and dopamine release in vivo via stimulation of M1 muscarinic receptors. Neuropsychopharmacology 2005; 30: 1986–95.
Liu L, Huang J, Hu X, Li K, Sun C . Simultaneous determination of ginsenoside (G-Re, G-Rg1, G-Rg2, G-F1, G-Rh1) and protopanaxatriol in human plasma and urine by LC-MS/MS and its application in a pharmacokinetics study of G-Re in volunteers. J Chromatogr B Analyt Technol Biomed Life Sci 2011; 879: 2011–7.
Wang A, Wang CZ, Wu JA, Osinski J, Yuan CS . Determination of major ginsenosides in Panax quinquefolius (American ginseng) using high-performance liquid chromatography. Phytochem Anal 2005; 16: 272–7.
Peng D, Wang H, Qu C, Xie L, Wicks SM, Xie J . Ginsenoside Re: Its chemistry, metabolism and pharmacokinetics. Chin Med 2012; 7: 2.
Liu YW, Zhu X, Li W, Lu Q, Wang JY, Wei YQ, et al. Ginsenoside Re attenuates diabetes-associated cognitive deficits in rats. Pharmacol Biochem Behav 2012; 101: 93–8.
Jing FC, Chen H, Li CL . Rapid determination of dopamine and its metabolites during in vivo cerebral microdialysis by routine high performance liquid chromatography with electrochemical detection. Biomed Environ Sci 2007; 20: 317–20.
Carlsson A, Sharp T, Zetterstrom T, Ungerstedt U . Determination of dopamine and its metabolites in small volumes of rat brain dialysates using small-bore liquid chromatography with electrochemical detection. J Chromatogr 1986; 368: 299–308.
Ichikawa J, Li Z, Dai J, Meltzer HY . Atypical antipsychotic drugs, quetiapine, iloperidone, and melperone, preferentially increase dopamine and acetylcholine release in rat medial prefrontal cortex: role of 5-HT1A receptor agonism. Brain Res 2002; 956: 349–57.
DeBoer P, Abercrombie ED . Physiological release of striatal acetylcholine in vivo: modulation by D1 and D2 dopamine receptor subtypes. J Pharmacol Exp Ther 1996; 277: 775–83.
Joo KM, Lee JH, Jeon HY, Park CW, Hong DK, Jeong HJ, et al. Pharmacokinetic study of ginsenoside Re with pure ginsenoside Re and ginseng berry extracts in mouse using ultra performance liquid chromatography/mass spectrometric method. J Pharm Biomed Anal 2010; 51: 278–83.
Stormer VS, Passow S, Biesenack J, Li SC . Dopaminergic and cholinergic modulations of visual-spatial attention and working memory: Insights from molecular genetic research and implications for adult cognitive development. Dev Psychol 2012; 48: 875–89.
Vitiello B, Martin A, Hill J, Mack C, Molchan S, Martinez R, et al. Cognitive and behavioral effects of cholinergic, dopaminergic, and serotonergic blockade in humans. Neuropsychopharmacology 1997; 16: 15–24.
Levin ED, McGurk SR, Rose JE, Butcher LL . Cholinergic-dopaminergic interactions in cognitive performance. Behav Neural Biol 1990; 54: 271–99.
Li X, Wang G, Sun J, Hao H, Xiong Y, Yan B, et al. Pharmacokinetic and absolute bioavailability study of total panax notoginsenoside, a typical multiple constituent traditional Chinese medicine (TCM) in rats. Biol Pharm Bull 2007; 30: 847–51.
Bae EA, Shin JE, Kim DH . Metabolism of ginsenoside Re by human intestinal microflora and its estrogenic effect. Biol Pharm Bull 2005; 28: 1903–8.
Acknowledgements
This work was supported as a Key Project of the Eleventh National Five Year Research Program of China, “New Drug Creation and Development Program” (No 2008ZX09312).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shi, J., Xue, W., Zhao, Wj. et al. Pharmacokinetics and dopamine/acetylcholine releasing effects of ginsenoside Re in hippocampus and mPFC of freely moving rats. Acta Pharmacol Sin 34, 214–220 (2013). https://doi.org/10.1038/aps.2012.147
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.147
Keywords
This article is cited by
-
Ginseng® as a reproductive enhancer agent for African catfish, Clarias gariepinus (Burchell, 1822)
Fish Physiology and Biochemistry (2022)
-
Herbal medicine in the treatment of Alzheimer’s disease
Chinese Journal of Integrative Medicine (2015)
-
Potential Neuroprotective Activity of Ginseng in Parkinson’s Disease: A Review
Journal of Neuroimmune Pharmacology (2015)
-
Ginsenoside compound K suppresses the abnormal activation of T lymphocytes in mice with collagen-induced arthritis
Acta Pharmacologica Sinica (2014)