Abstract
Aim:
To characterize the biological profiles of MJ08, a novel selective CB1 receptor antagonist.
Methods:
Radioligand binding assays were performed using rat brain and spleen membrane preparations. CB1 and CB2 receptor redistribution and intracellular Ca2+ ([Ca2+]i) assays were performed with IN CELL Analyzer. Inverse agonism was studied using intracellular cAMP assays, and in guinea-pig ileum and mouse vas deferens smooth muscle preparations. In vivo pharmacologic profile was assessed in diet-induced obesity (DIO) mice.
Results:
In radioligand binding assay, MJ08 selectively antagonized CB1 receptor (IC50=99.9 nmol/L). In EGFP-CB1_U2OS cells, its IC50 value against CB1 receptor activation was 30.23 nmol/L (SR141716A: 32.16 nmol/L). WIN 55,212-2 (1 μmol/L) increased [Ca2+]i in the primary cultured hippocampal neuronal cells and decreased cAMP accumulation in CHO-hCB1 cells. MJ08 (10 nmol/L–10 μmol/L) blocked both the WIN 55,212-2-induced effects. Furthermore, MJ08 reversed the inhibition of electrically evoked twitches of mouse vas deferens by WIN 55,212-2 (pA2=10.29±1.05). MJ08 and SR141716A both showed an inverse agonism activity by markedly promoting the contraction force and frequency of guinea pig ileum muscle. MJ08 significantly increased the cAMP level in CHO-hCB1 cells with an EC50 value of 78.6 nmol/L, which was lower than the EC50 value for SR141716A (159.2 nmol/L). Besides the more potent pharmacological effects of cannabinoid CB1 receptor antagonism in DIO mice, such as reducing food intake, decreasing body weight, and ameliorating dyslipidemia, MJ08 (10 mg/kg) unexpectedly raised the fasted blood glucose in vivo.
Conclusion:
MJ08 is a novel, potent and selective CB1 receptor antagonist/inverse agonist with potent bioactive responses in vitro and in vivo that may be useful for disclosure the versatile nature of CB1 receptors.
Similar content being viewed by others
Introduction
Cannabinoid CB1 receptors are widely expressed in both the central and peripheral nervous systems, and they display numerous physiological effects such as behavioral, neuroprotective, immunosuppressive, and metabolic functions1, 2, 3. In the past decade, the metabolic homeostasis regulated by the cannabinoid CB1 receptor has been the focus of intensive studies. Striking advances were made in developing high affinity selective cannabinoid CB1 receptor antagonists and/or inverse agonists as therapeutic agents for obesity, diabetes and metabolic syndrome. Some selective antagonists of the cannabinoid CB1 receptor have been developed and reached various stages of clinical trials. These new chemical entities also provided useful tools for understanding the sophisticated physiological mechanism of this receptor4, 5, 6. Among them, the most representative selective antagonist/inverse agonist of the cannabinoid CB1 receptor is rimonabant (SR141716A). It was developed by Sanofi-Aventis and approved for treatment of obesity in Europe in June of 2006. Unfortunately, psychiatric side effects delayed its approval in the United States, which also led to subsequent market withdrawal of the drug in the European Union in late 2008. Hence, to circumvent the problems that have beset the current agents, some strategies such as developing non-brain penetrating and peripheral restrictive CB1 receptor antagonists or focusing on allosteric modulation of CB1 receptors are being used at present7, 8.
Previously reported cannabinoid CB1 receptor selective antagonists exhibited mainly two types of behavior9, 10. One type, expressed by SR141716A and Imidazole 24b, has effects in the opposite direction to those produced by the cannabinoid receptor agonists, ie, they are cannabinoid CB1 receptor inverse agonists11, 12. The other type is expressed by the cannabinoid CB1 receptor neutral antagonist, such as AM4113, with no intrinsic activity13. It was presumed that the inverse agonist and neutral antagonist may involve different signal transduction mechanisms. However, aside from their structural differences, the related pharmacological and toxicological effects produced by the different types of cannabinoid CB1 receptor antagonists are still not completely known.
Novel drug candidates acting against cannabinoid CB1 receptors, such as MJ08 and MJ15, were discovered in our laboratory through a series of in-vitro, ex-vivo, and in-vivo biological screenings and evaluations. Both compounds behaved as highly potent selective cannabinoid CB1 receptor antagonists. Although they have similar molecular formulas, the substitution with piperidin-1-yl at the N atom of the pyrazol 3 site (N-pyridin-3-methyl for MJ15) characterizes MJ08 (patent No CN101062919A) with different receptor-binding characteristics and bioactivities14. MJ08 exhibits an inverse agonism activity even stronger than that of SR141716A in functional assays; however, it has a relatively lower affinity than SR141716A in radioligand competitive binding analysis. In addition to its significant weight loss effect, MJ08 increases fasting blood glucose in diet-induced obesity (DIO) mice. The in vitro and in vivo pharmacological profiles of MJ08 were described in this paper.
Materials and methods
Drugs and Chemicals
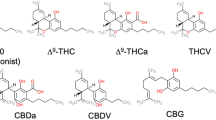
Forskolin, CP55, 940 (CB1/CB2 agonist), WIN 55,212-2 (CB1/CB2 agonist), and Fluo-3 were purchased from Sigma. [3H]-SR141716A and [3H]-WIN 55,212-2 were purchased from Amersham. SR141716A and MJ08 were synthesized and prepared by the New Drug Design Center of Beijing Institute of Pharmacology and Toxicology. The purity and structure of these two compounds were confirmed by high-performance liquid chromatography, mass spectrometry and 1H-nuclear magnetic resonance (NMR). The structure of MJ08 {[5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazol-3-yl](piperidin-1-yl)methanone} is shown in Figure 1.
Membrane preparations and radioligand competitive binding analysis
The cannabinoid CB1 and CB2 receptor membranes were prepared from rat brain and spleen, respectively, as reported in our previous paper, and stored at −80 °C until use14. Competitive binding analysis was conducted by incubating 50 μg of membrane and competing ligand (2.4 nmol/L [3H]-SR141716A for CB1 and 6.4 nmol/L [3H]-WIN 55,212-2 for CB2) in Tris-HCl (50 mmol/L, pH 7.4) at 30 °C for 1 h. Competitive binding inhibition curves were generated with different concentrations of SR141716A or MJ08. The radioactivity bound to the filters was counted with 1 mL of Biofluor liquid scintillant (New England Nuclear Corp, UK) in a LS6500 counter. Non-specific binding was determined in the presence of 25 μmol/L non-radioactive SR141716A for CB1 and CP55 940 for the CB2 receptor. The affinity of MJ08 to the CB1 or CB2 receptor was expressed as a Ki value or an inhibition of the specific binding of radioactive [3H]-SR141716A to the CB1 receptor or [3H]-WIN 55,212-2 to the CB2 receptor. Each competitive binding inhibition curve was generated from the data pooled from three independent experiments conducted in duplicate.
Assay of cannabinoid receptor antagonism at the cellular level
Thermo scientific CB1 and CB2 redistribution assays (Themo Fisher Bioimage ApS, Soeborg, Denmark) were used to analyze the antagonistic effects and the selectivity of MJ08 with SR141716A as the reference compound. The assay was performed as previously reported14. The cannabinoid CB1 and CB2 antagonist redistribution assay formats were specially designed cell models to screen agonists or antagonists of CB1 and CB2 receptors, respectively. The assay was validated with an average Z′=0.55±0.21 (CB1) and Z′=0.34±0.1 (CB2) and was suitable for both high content screening and profiling applications (Thermo scientific cannabinoid CB1 and CB2 redistribution assay specifications).
Before each experiment, the culture medium was changed to assay buffer [F12 culture medium containing 1 μmol/L Hoechst 33342 (Invitrogen, Oregon, USA)] and incubated at 37 °C for 20 min before different concentrations (10 nmol/L, 100 nmol/L, 1 μmol/L, and 10 μmol/L) of SR141716A or MJ08 combined with 1 μmol/L WIN 55,212-2 [the maximally active concentration on the EGFP-CB_U2OS cells (EGFP, enhanced green fluorescent protein)] was added. After further incubation at 37 °C for 2 h, the cells were imaged on the IN Cell Analyzer 1000 (20×objective), and the pictures were analyzed with the Granularity Analysis Module of IN Cell. DMSO (0.1%) was used as the vehicle control. The inhibition ratio of a test compound was expressed as percent inhibition of the internalization induced by the reference agonist WIN 55,212–2. The corresponding IC50 values were calculated from the inhibition ratios. The results were obtained from three independent experiments performed in triplicate.
Hippocampal neurons and Fluo-3/AM Ca2+ imaging
Intracellular Ca2+ assays were conducted in hippocampal neurons as previously described14. After being washed with HBS solution (130 mmol/L NaCl, 5.4 mmol/L KCl, 1.8 mmol/L CaCl2, 1 mmol/L MgCl2, 10 mmol/L HEPEs, and 25 mmol/L D-glucose, pH 7.4), the cells were incubated for 60 min with 10 μmol/L fluorescent Ca2+ indicator, fluoro-3 acetoxymethyl ester (Fluo-3/AM), and then pluronic acid F-127 (Cambridge Bioscience, Cambridge, UK) was added. Subsequently, the cells were washed again three times with HBS and challenged with 0.1% DMSO (vehicle control), or SR141716A or MJ08 at different concentrations (10 nmol/L, 100 nmol/L, 1 μmol/L, or 10 μmol/L). An application of 1 μmol/L WIN 55,212-2 was administered 1 min later. Fluorescence was monitored and imaged with the IN Cell Analyzer 1000 (GE Healthcare, NJ, USA) at 3 s intervals, and then analyzed with the Object Intensity Analysis Module of IN Cell. Background levels of fluorescence were subtracted at the beginning of the experiments. The time courses of [Ca2+]i change were plotted by recording the relative fluorescence intensity per cell vs time.
Intracellular cAMP assays
Stable Chinese hamster ovary (CHO) cells expressing the human cannabinoid CB1 and CB2 (CHO-hCB1 and CHO-hCB2, respectively) receptors were established in our previous work14. Functional antagonism of the cannabinoid CB1 receptor agonist response was measured by incubating the recombinant cannabinoid CHO cells with various concentrations of test ligands and 200 μmol/L 3-isobutyl-1-methylxanthine (IBMX, phosphodiesterase inhibitor) in the assay buffer at room temperature for 30 min. The intrinsic inverse agonism was tested in the presence of 1 μmol/L forskolin in CHO- hCB1 and CHO-hCB2 cells as above. Intracellular cAMP was assayed with the LANCE cAMP 384 kit (AD0262, PerkinElmer, CA, USA) according to the manufacturer's specifications. Briefly, cells were harvested with versene, washed with Hank's Balanced Salt Solutions (HBSS) and re-suspended in stimulation buffer at a concentration of 1.7×106/mL. Six μL of the cell suspension (containing the Alexa-labeled antibodies) were added into one well of white OptiPlate-384, and then 6 μL of different compound dilutions was added. After incubation for 30 min at room temperature, 12 μL of detection mix was added and further incubated for 60 min. The fluorescence was read on EnVision Multilabel Plate Readers (PerkinElmer, CA, USA) with 475 nm excitation and 665 nm emission. The amounts of cAMP produced in the stimulated cells were determined according to the cAMP standard curves. In the inverse agonism assay, 10 μmol/L MJ08-enhanced, forskolin-stimulated cAMP production was used to define 100% efficacy, and the correspondent IC50 values were calculated from the curve.
Tissue preparations and contraction studies
Male Kun-ming mice (25–30 g) and guinea-pigs (350–400 g) from Laboratory Animal Center of Pharmaceutical University of Shenyang, China, were humanely killed by decapitation following CO2 asphyxiation. The vas deferens and ileum were excised according to the method in the literature15, 16, 17 and placed in Krebs' physiological salt solution [pH 7.4, composition (mmol/L): NaCl 119, KCl 4.69, KH2PO4 1.18, glucose 11, NaHCO3 25, CaCl2 2.5, EDTA 0.026], gassed with 95% O2/5% CO2 and maintained at 37 °C. Each vas deferens or ileum was mounted in a 30-mL organ bath and connected to an isometric transducer (RM6240CD, Chengdu, China). The vas deferens was subsequently equilibrated for 30 min and stimulated with trains of 10 pulses of 40 V for 0.5-ms duration at intervals of 50 ms. Contraction data were registered on a polygraph recorder before and after incubation with 10−7 mol/L SR14716A, 10−7 mol/L MJ08 or the vehicle (0.1% DMSO) for 30 min. The cannabinoid agonist WIN 55,212-2 was then added at 30-min intervals to construct an inhibitory cumulative concentration-response curve. The inhibition rate of the tested compounds was calculated with the following equation: (An−A0)/A0×100%, where A0 and An denote the twitch amplitude of the tested compounds before and after the administration of different concentrations of WIN 55,212-2, respectively. The pA2 values were determined using the method of Arunlakshan and Schild, ie, pA2=log (E′/E−1)−logB, where E′ is the ED50 of the agonist under the presence of the antagonist, E is the ED50 of the agonist in the absence of the antagonist and B is the concentration of the antagonist.
Meanwhile, the specific effects of the test compounds on the contraction of the vas deferens smooth muscle and guinea-pig ileum were also observed. After equilibration for 30 min, the vas deferens was stimulated as described above, and a recording of the contraction amplitude was begun before administration of SR141716A or MJ08 for 30 min at ten-fold increments using 30-min intervals to construct a cumulative concentration-response curve. For the ileum, contraction data were recorded for 2 min before and after treatments, and cumulative concentration-response curves were generated.
Animals and treatment
Animals were obtained from Laboratory Animal Center of Beijing Institute of Pharmacology and Toxicology, unless otherwise stated. All animal experiments were performed strictly in accordance with the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health and were approved by the Institutional Animal Care and Use Committee of the Beijing Institute of Pharmacology and Toxicology. Male Wistar rats (220–240 g) and their neonates (1 d) were used for radioligand competitive binding studies and primary cultures of hippocampus cells, respectively.
Male C57BL/6J mice (6 weeks old), maintained under controlled illumination (12/12-h light/dark cycle) and temperature (22±1 °C), were fed a high-fat diet (45% fat, 18% protein, 37% carbohydrate) for 16 weeks to obtain a DIO mouse model. Age-matched lean mice were used as normal controls. The DIO mice were randomly divided into three groups based on their initial body weights. SR141716A (10 mg·kg−1·d−1), MJ08 (10 mg·kg−1·d−1) or the vehicle (1% DMSO) were administered by gavage once daily for 40 d. Individual body weight and cage food consumption were measured every day. At the end of the experimental period, the mice were fasted overnight, and blood samples were collected for the assessment of serum glucose, triglycerides (TG) and total cholesterol (TC) levels as previously described18.
Statistical analysis
All results are expressed as the mean±SD. For multiple comparisons, the statistical analysis was performed using one-way ANOVA followed by Tukey's multiple comparison tests with SPSS 11.5. P<0.05 was considered to be statistically significant.
Results
Selective interaction of MJ08 with the cannabinoid CB1 receptor at the molecular level
Figure 2 showed that [3H]-SR141716A can specifically bind to the cannabinoid CB1 receptor of rat brain membranes, and such interaction can be replaced by unlabeled SR141716A or MJ08 in a concentration-dependent manner. However, it is noted that the competitive binding inhibition curves of SR141716A or MJ08 are different in slope and shape. SR141716A exhibited a sharply competitive effect from 10−11 to 10−9 mol/L; nevertheless, MJ08 gradually inhibited [3H]-SR141716A binding from 10−14 to 10−4 mol/L. The concentration-response curves gave Ki and IC50 values of 25.4 and 99.9 nmol/L, respectively, for MJ08, and 22.9 and 99.3 pmol/L, respectively, for SR141716A. In contrast, both SR141716A and MJ08 showed very low affinity to the CB2 receptor expressed in rat spleen preparations; even at a higher concentration (about 34% inhibition at 10 μmol/L for both compounds, n=6), they could not compete with the binding of [3H]-WIN 55,212-2 to the CB2 receptor. However, the cannabinoid CB1/CB2 receptor agonist CP55,940 could antagonize this effect under the same conditions, with more than 90% inhibition to the CB2 receptor at 100 nmol/L (data not shown). These results indicate that MJ08 is a selective cannabinoid CB1 (not CB2) ligand but that it has relatively lower affinity than SR141716A at an in vitro molecular level.
The competitive inhibition of [3H]-SR141716A binding to the CB1 receptor by MJ08 and SR141716A. The specific binding rate of 2.4 nmol/L [3H]-SR141716A was defined as 1; other values of [3H]-SR141716A binding under different concentrations of SR141716A or MJ08 were relative to that. Values are the mean±SD.
MJ08 antagonized the activation of the cannabinoid CB1 receptor at the cellular level
As a Gi/s-coupled G-protein-coupled receptor (GPCR), the cannabinoid receptor is rapidly internalized following agonist binding and receptor activation19. Recombinant U2OS cells stably express human cannabinoid CB1 or CB2 receptors fused to the N-terminus of EGFP. The cannabinoid CB1 or CB2 receptor internalization assay is available for the screening of agonists or antagonists of the cannabinoid CB1 and CB2 receptors. Figure 3A shows that 1 μmol/L CB1/CB2 receptor agonist WIN 55,212-2 markedly induced the internalization of the membrane-localized CB1-EGFP fusion protein to the endosomes; the agonistic potency was 2.59 times that of the vehicle control. However, when co-administered with MJ08, it dose-dependently antagonized the internalization of the CB1-EGFP fusion protein, and the IC50 calculated from the concentration-response curve was 30.23±6.41 nmol/L, which was comparable to the value of SR141716A (32.16±6.72 nmol/L) in the same experiment (Figure 3B). However, both SR141716A and MJ08 exhibited weak antagonism towards the cannabinoid CB2 receptor activation and internalization induced by WIN 55,212-2 in EGFP-CB2_U2OS cells, with only approximately 25% to 35% inhibition by 10 μmol/L of MJ08 or SR141716A (data not shown). Therefore, MJ08 is macroscopically demonstrated to be equally potent and selective as a CB1 receptor antagonist as SR141716A in the cellular assay.
Representative images of EGFP-CB1_U2OS cells treated with the vehicle or different compounds (A) and the concentration-response curve of MJ08 and SR141716A (B). Arrows indicate WIN 55,212-2-induced CB1 receptor internalization detected by the IN Cell Analyzer. The results were obtained from three independent experiments performed in triplicate: WIN, WIN 55,212-2 1 μmol/L; WIN+SR, WIN 55,212-2 1 μmol/L+SR141716A 100 nmol/L; WIN+MJ, WIN 55,212-2 1 μmol/L+MJ08 100 nmol/L.
MJ08 antagonized the elevation and oscillation of [Ca2+]i induced by the cannabinoid CB1 receptor agonist
[Ca2+]i was measured in hippocampal neurons using the fluorescent dye Fluo3/AM as an indicator. It had been shown that cannabinoid CB1, rather than the CB2 receptor, is predominantly expressed in hippocampal tissue, and cannabinoid CB1 receptor activation increases [Ca2+]i20. In cultured rat hippocampal cells, 1 μmol/L CB1/CB2 receptor agonist WIN 55,212-2 significantly increased [Ca2+]i (Figure 4); the [Ca2+]i signal showed an initial rise, slow decay, and sustained elevated phase with oscillations. SR141716A and MJ08 both (10 nmol/L to 10 μmol/L) blocked the activation of the cannabinoid CB1 receptor by WIN 55,212-2 and the following induced elevation and oscillations of intracellular Ca2+ (Figure 4B). This result indicates that MJ08 may antagonize the second messenger molecules of cannabinoid CB1 receptor activation.
Intracellular free Ca2+ [Ca2+]i measured by Ca2+ indicators in hippocampal cells. (A) Representative micrographs showing intracellular [Ca2+]i in hippocampal cells. (B) The dynamic course of different concentrations of SR141716A (SR) or MJ08 (MJ) antagonizing WIN 55,212-2-induced elevation and pulse oscillation of intracellular [Ca2+]i.
Antagonism on intracellular cAMP and inverse agonism of MJ08
The effect of MJ08 on the agonist-mediated decrease of cAMP level in CHO cells expressing human cannabinoid CB1 receptor was examined. Like SR141716A, MJ08 (0.1 and 1 μmol/L) also significantly and dose-dependently reversed the WIN 55,212-2-induced inhibition of forskolin-stimulated cAMP accumulation, and intracellular cAMP contents at higher doses even exceeded that induced by forskolin alone; this suggests that MJ08 may also possess the inverse agonism property (Figure 5A). Neutral antagonists and inverse agonists can be well differentiated by the intracellular cAMP assay when the agonist is absent. Therefore, to further verify its functional inverse agonism, MJ08 was tested by the cAMP assays in both CHO-hCB1 and CHO-hCB2 cells. Figure 5B showed that 1 nmol/L of MJ08 can further increase cAMP levels in CHO-hCB1 cells in the presence of 1 μmol/L forskolin, and the four-fold increase of the Emax (maximal effect) was obtained at 10 μmol/L with the EC50 of 78.6 nmol/L. However, an antagonizing effect of SR141716A was observed at 1 nmol/L under the same conditions. Inverse agonism was displayed above 10 nmol/L, and the Emax value was significantly lower than that of MJ08 (P<0.05), which corresponds to that of MJ08 at 1 μmol/L. The EC50 in this assay was 159.2 nmol/L, about two-fold that of MJ08. However, MJ08 and SR141716A did not influence intracellular cAMP in CHO-hCB2 cells, even at 10 μmol/L. These data indicate that MJ08 possesses more potent intrinsic inverse agonistic activity to CB1 receptors than SR141716A in the absence of the receptor agonist.
Effect of MJ08 on 1 μmol/L WIN 55,212-2 induced inhibition of cAMP accumulation stimulated by 0.1 μmol/L forskolin (A) and inverse agonism property of MJ08 in CHO-hCB1 cells (B). The data were derived from a cell-based assay measuring the intracellular cAMP level with the LANCE cAMP kits. Fos (F), forskolin; WIN (W), WIN 55,212-2; values are the mean±SD. cP<0.01 versus vehicle; fP<0.01 versus forskolin; hP<0.05, iP<0.01 versus F+W.
The effects of MJ08 on the contraction of guinea pig ileum and mouse vas deferens smooth muscle
At concentrations of 10−6 and 10−5 mol/L, SR141716A markedly increased the contraction intensity of guinea pig ileum smooth muscle, but its potency tended to decrease in a time-dependent manner (Figure 6A). The contraction frequency was only significantly increased at 10−5 mol/L at 60 and 120 s after the administration (Figure 6C). MJ08 demonstrated a similar promotion effect. It remarkably increased the contraction force and frequency. However, a more significant effect was observed on frequency, which was strikingly enhanced by MJ08 and without attenuation over time, even at 10−9 mol/L at 60 s (Figure 6B, 6D).
Effect of MJ08 and SR141716A on the contractions of the guinea pig ileum measured 2 min after compound administration. (A) and (B) SR141716A and MJ08 promoted the contraction amplitude. (C) and (D) SR141716A and MJ08 promoted the contraction frequency. Values are the mean±SD (n=6). bP<0.05, cP<0.01, versus vehicle.
The electrically-stimulated vas deferens bioassay was reported to be a preferable approach for the determination of the antagonist potency17. Without pretreatment with the antagonist, the cannabinoid CB1/CB2 receptor agonist WIN 55,212-2 elicited a concentration-dependent inhibition of the twitches of mouse vas deferens (IC50=0.44 nmol/L), and a nearly completed inhibition appeared at 10−6 mol/L (Figure 7A and B). At 10−7 mol/L, both SR141716A and MJ08 significantly antagonized the inhibitory effect of WIN 55,212-2 (P<0.01 for both) and induced dextral displacements of the agonist's dose-responsive curve with IC50 values of 0.206 and 3.31 μmol/L, respectively (Figure 7A). The competitive interaction between the antagonist and agonist signified that SR141716A and MJ08 were competitive antagonists of WIN 55,212–2. The calculated pA2 values for SR141716A and MJ08 were 9.47±0.73 and 10.29±1.05, respectively, indicating that the antagonistic potency of MJ08 was comparable to that of SR141716A. However, when the concentration of WIN 55,212-2 increased to 3 μmol/L, SR141716A (0.1 μmol/L) nearly lost its antagonism, whereas MJ08 (0.1 μmol/L) still preserved the contract ability of the muscle (Figure 7B). Furthermore, MJ08 and SR141716A both had trends towards promoting the electrically-evoked twitches of the mouse vas deferens even at a concentration of 1 nmol/L in absence of the agonist, although without apparent dose-response relationships (data not shown). These results indicate that MJ08 is not only a selective and competitive CB1 receptor antagonist but also a cannabinoid CB1 receptor inverse agonist with equal or more potency than SR141716A.
Effect of MJ08 and SR141716A on electrically-evoked twitches of the mouse vas deferens measured 30 min after drug administration. (A) The antagonistic effect on inhibiting the contraction induced by WIN 55,212–2. 10−7 mol/L SR141716A or MJ08 were added to the bath solutions 30 min before the agonist. (B) Representative records of mouse vas deferens' contraction. Values are the mean±SD (n=5–6).
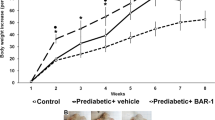
Effect of MJ08 in DIO mice
Adverse effects on animal behavior or obvious signs of toxicity were not observed at any point in the experiment for any treatment group. The body weight of DIO mice was significantly higher than that of normal mice (32.02±0.83 g vs 24.3±0.29 g, P<0.01) at the beginning of the experiment. Sequential monitoring showed that both SR141716A and MJ08 decreased the body weight of the DIO mice throughout the experiment. On average, the body weight of MJ08-treated mice was relatively lower than that of SR141716A-treated mice during the first 25 d of treatment (Figure 8A). The impact of food intake was similar between the two testing compounds, which was reduced only in the first 10 d of administration and then relapsed to the consumption amount of the model group (Figure 8B). Meanwhile, both SR141716A and MJ08 dramatically decreased the hypertriglyceridemia (P<0.05) and the intra-abdominal adipose tissue (P<0.05) in DIO mice (Table 1). However, different from SR141716A, MJ08 also markedly lowered serum TC levels (P<0.05). Unexpectedly, the fasting blood glucose of the DIO mice was significantly increased by MJ08 after 35 d of treatment (P<0.01), yet it was decreased by SR141716A. However, the increased fasting blood glucose soon recovered to normal once MJ08 was withdrawn (the FBG were 5.04±1.09 mmol/L and 4.57±0.91 mmol/L at 5 and 10 d after discontinuation, respectively).
Effects of MJ08 on body weight, food intake and white adipose weight in DIO mice. (A) Body weight change, which was calculated for individual mouse and then averaged. (B) Food intake, which was calculated every day and then averaged. (C) Epididymal fat weight and (D) Perirenal fat weight index. SR, SR141716A. Values are the mean±SD of 10–12 animals per group. cP<0.01 versus normal; eP<0.05, fP<0.01 versus model.
Discussion
As a new chemical entity targeting the cannabinoid CB1 receptor, the pharmacological properties of MJ08 were evaluated in various in vitro and in vivo experimental systems in the present study. MJ08 exhibited selective and potent antagonism to the cannabinoid CB1 receptor. Although in vitro competitive binding analysis revealed that its affinity was lower than that of SR141716A at the molecular level, the cellular cannabinoid receptor activation and transposition assay, [Ca2+]i and cAMP measurements in mammalian cells functionally demonstrated the equivalent efficiency of MJ08 in selectively antagonizing the cannabinoid CB1 receptor compared with SR141716A. Furthermore, more potent or equivalent cannabinoid CB1 receptor inverse agonistic effects of MJ08 relative to SR141716A were revealed by directly increasing intracellular cAMP and promoting the contraction of guinea pig ileum and mouse vas deferens smooth muscles in isolated tissues at in vitro and ex vivo tests. Additionally, the results from DIO mice further confirmed its oral bioactivity and in vivo potency.
Receptor competitive binding analysis is a classical method for the evaluation of binding characteristics of ligands. Rat cerebellum and spleen (CB1 and CB2 receptor-rich tissues, respectively) membrane preparations were used here to analyze the receptor binding activity and characteristics of MJ08. The radioligand displacement curves showed that, similar to the well-known cannabinoid CB1 receptor selective antagonist SR141716A, MJ08 dose dependently displaced [3H]-SR141716A binding to rat cerebellum membranes, and its selectivity to the CB1 receptor against the CB2 receptor was more than 100-fold. However, the binding affinity of MJ08 to the CB1 receptor was about 500–1000 times less potent than that of SR141716A. It was noted that the slope of the displacement curve was steeper for SR141716A than MJ08, SR141716A exhibited a sharp competitive effect from 10−11 to 10−9 mol/L, but MJ08 gradually inhibited [3H]-SR141716A's binding from 10−14 to 10−4 mol/L. This result indicates that the binding mode of MJ08 is somewhat different from that of SR141716A. MJ08 showed more potent affinity to the CB1 receptor at a lower concentration in the molecular test.
Recently, functional assays of receptor activation in living cells were widely used in screening and in the evaluation of novel ligands for receptors. Compared with molecular-level assays, living cell assays reflect both receptor binding and the functional activity of a ligand. In this study, the CB1/CB2 redistribution assay (commercial EGFP-CB1/CB2_U2OS cell model, specially designed for screening of agonists or antagonists of cannabinoid CB1/CB2 receptor with High Content Assay) was used. Both MJ08 and SR141716A antagonized the internalization of the membrane-located CB1-EGFP fusion protein induced by the agonist (WIN 55,212-2) without significant impact to WIN 55,212-2-induced internalization of the membrane-located CB2-EGFP fusion protein; this signified that they selectively antagonized the cannabinoid CB1 receptor activation in the cellular model. Moreover, in contrast to the receptor binding test at the molecular level, MJ08 displayed an equivalent antagonistic effect to SR141716A in the living cell assay suggesting that MJ08 may be more suitable for binding to CB1 receptor in living cells.
Intracellular Ca2+ and adenylyl cyclase are considered to be important signaling molecules of cannabinoid CB1 receptors20, 21, 22. To confirm the functional antagonistic activities of MJ08 toward the cannabinoid CB1 receptor, the effects of MJ08 on cannabinoid CB1 receptor agonist-induced responses, including intracellular Ca2+ ([Ca2+]i) and cAMP content, were observed in hippocampal neurons (abundance of CB1 receptor) and CHO-hCB1 cells, respectively. It has been documented that the cannabinoid CB1/CB2 receptor agonist WIN 55,212-2 increases intracellular Ca2+ via CB1 coupling to Gq/11 G proteins20. In our experiment, similar to SR141716A and other reported antagonists23, 24, the increase of [Ca2+]i induced by WIN 55,212-2 was absent in hippocampal neurons after the incorporation of MJ08 (from 10−8 to 10−5 mol/L) with comparable efficiency to SR141716A. Additionally, as CB-coupled Gi/o proteins, cAMP is the key molecule in reflecting cannabinoid CB1 receptor activation or antagonism. Our results revealed that MJ08 significantly reversed WIN 55,212-2-induced inhibition of forskolin-stimulated cyclic AMP accumulation in a dose-dependent manner in CHO-hCB1 cells. Taken together, the [Ca2+]i and cAMP assays demonstrated that MJ08 acts as a cannabinoid CB1 receptor antagonist of second messenger signaling in mammalian cells with similar efficacy to SR141716A. Additionally, both SR141716A and MJ08 significantly antagonized the inhibition by WIN 55,212-2 of the contraction of mouse vas deferens smooth muscle with electrical stimulation. The relatively higher pA2 value of MJ08 than SR141716A in this assay indicates its stronger or comparable antagonism. Therefore, the above results suggest that MJ08 is a potent and highly selective cannabinoid CB1 receptor antagonist.
On the other hand, MJ08 also displayed inverse agonist properties, ie, inhibiting CB1 receptor activity in the absence of an agonist, which includes directly increasing cAMP accumulation in CHO-hCB1 cells and promoting contractions of isolated preparations of guinea pig ileum and mouse vas deferens. In CHO-hCB1 cells, MJ08 not only enhanced cAMP accumulation in the presence of forskolin (its efficacy was about 5 to 10 times of SR141716A) but also markedly evoked the increase of intracellular cAMP in the absence of forskolin at higher concentrations. The efficacy of 1 μmol/L of MJ08 also corresponds to the efficacy of 10 μmol/L of SR141716A (data not shown). This result indicates that MJ08 is a more potent inverse agonist of the cannabinoid CB1 receptor than SR141716A. SR141716A has been shown to enhance the contraction force of guinea pig ileum smooth muscle in isolated guinea pig ileum tests, but we found that it displayed a time-dependent decreasing trend, with the maximum effect at 30 s. The contraction frequency was increased 1.16 times by 10−5 mol/L SR141716A at 60 s, whereas MJ08 significantly enhanced both the contraction force and frequency under the same conditions without attenuation with time. The contraction frequency was significantly increased by MJ08 even at 10−9 mol/L at 60 s and reached to 1.24 times with 10−5 mol/L MJ08. In the isolated mouse vas deferens experiment, similar to known inverse agonists, SR141716A or and MJ08 also both promoted the electrically-evoked contractions of the mouse vas deferens at concentrations ranging from 10−10 to 10−6 mol/L, although the contraction amplitude was only slightly increased. This phenomenon corresponded with the point that the inverse agonist exhibited greater potency in producing opposing effects induced by the cannabinoid CB1 receptor agonists9. As MJ08 did not interact directly with the muscarinic receptor or adrenergic receptor α (data not shown), the mechanisms by which MJ08 promotes muscle contraction and the electrically-evoked contractions of the mouse vas deferens are likely to be cannabinoid CB1 receptor mediated rather than through non-specific interactions with other receptors. Therefore, MJ08 is a selective antagonist and inverse agonist of the cannabinoid CB1 receptor.
Previously, an increasing body of evidence has demonstrated the roles of the endogenous cannabinoid system (ECs), including CB1 receptor, endocannabinoids, and related metabolic enzymes, in the regulation of food consumption and body weight in animals and humans25, 26. Hyperphagic effects are closely related to the hyperactivity of the ECs, and thus the endocannabinoid system had been a valuable therapeutic target for obesity27, 28. Correspondingly, the cannabinoid CB1 receptor antagonist had been shown to attenuate food intake and increase body energy expenditure in DIO mice and genetic obese animals26, 29, 30. Thus, in the present study, high-fat diet-induced obese mice were used to evaluate the in vivo pharmacodynamic effects of MJ08. Compared with SR141716A, chronic treatment with MJ08 displayed a higher efficacy in inducing weight loss (although without statistical difference), correcting dyslipidemia, and in lowering retroperitoneal adipose tissue in DIO mice. This effect suggests that MJ08 is an orally active cannabinoid CB1 receptor antagonist. Additionally, a significant increase in FBG in DIO mice by MJ08 was surprisingly found after 40 d of treatment; however, the FBG values returned to normal soon after compound withdrawal. Similarly, during the preparation of our manuscript, another CB1 receptor inverse agonist AM251 was also reported to increase the serum glucose level in 24-h fasted obese rats, but the author attributed it to heavy insulin resistance produced by hypercaloric diets31. However, this conclusion seems inappropriate because the serum insulin and glucose levels of the obese rats were both lower than that of the standard diet rats; the levels of the other two hormones (adiponectin and leptin) relating to glucose homeostasis were also comparable to the non-obese rats in their study31. Here, we considered two reasons may be responsible for this FBG increasing effect of a cannabinoid CB1 receptor antagonist/inverse agonist MJ08: first, it may be related to the activation of the sympathoadrenal system and the release of noradrenaline, which had been recently demonstrated in the diet-induced obese rats by Molhoj et al32; and secondly, MJ08 itself markedly increased intracellular cAMP, which may have promoted gluconeogenesis and/or glycogenolysis via increasing phosphorylation of phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphate (G6P), respectively. Therefore, the more potent inverse agonistic characteristic of MJ08 may be partially related to this FBG increasing effect, although the detailed mechanisms still need further study. However, if this is a category response of some CB1 receptor inverse agonists can't be completely excluded.
Additionally, it was also observed that the bioactivities of MJ08 became more potent as the experimental system advanced from the in vitro molecular level to the cellular level and then to the in vivo experiments; a significant enhancement was particularly seen between the molecular and cellular systems. First, we think that the incomplete, identical binding modes of MJ08 and SR141716A and the minute conformational change of the cannabinoid CB1 receptor in cell membrane preparations and living cells may be responsible for the phenomenon. When considering the cannabinoid CB1 receptor to be a well-defined but dynamic receptor protein, changes in the receptor steric conformation under different circumstances will likely affect its response to exogenous ligands. Secondly, the complex pharmacological regulations depend on the particular profile of the used ligand; the minute difference in structure of MJ08 may be key because the compound's conformation or conformational freedom is crucial for the receptor's affinity, selectivity, and efficacy33. Different small-molecule antagonists and inverse agonists bind in very different modes into the funnel of the main ligand-binding pocket GPCRs. In fact, MJ08 has a different amide in the 3 site of the pyrazole compared with SR141716A; when calculated with ChemOffice 2008, the LogP of MJ08 (7.04) is higher than that of SR141716A (6.28). This indicates that SR141716A is more hydrophilic than MJ08 and may thus display higher affinity at the in vitro molecular level, which is also confirmed by their different behaviors in the thin-layer chromatography assay. Certainly, the involved mechanisms need to be studied in further detail.
In conclusion, MJ08 is a structurally novel, potent and selective cannabinoid CB1 receptor antagonist with many specialized pharmacologic effects on different experimental systems. It exhibits potent inverse agonism and in vivo bioactivity. MJ08 may be used as a novel pharmacological tool to characterize the versatile nature and complexity of the cannabinoid signaling pathway.
Author contribution
Wei CHEN analyzed the data, wrote the manuscript and performed the experiments; Cheng XU analyzed the data and performed the experiments; Li-li WANG and Song LI designed the research and revised the paper; Hong-ying LIU, Long LONG, Wei ZHANG, Zhi-bing ZHENG, and Yun-de XIE performed the experiments.
Abbreviations
CHO, Chinese hamster ovary; DMSO, dimethyl sulphoxide; CP55,940, {5-(1,1-dimethylheptyl)-2-[5-hydroxy-2-(3-hydroxypropyl) cyclohexyl] phenol}; WIN 55,212-2, {[2, 3-Dihydro-5-methyl-3-[(morpholinyl)methyl]pyrrolo[1,2,3-de]-1,4-benzoxazinyl]-(1-naphthalenyl)methanone}; SR141716A, [N-Piperidino-5-(4-chlorophenyl)-1-(2, 4-dichlorophenyl)-4-methylpyrazole-3-carboxamide].
References
Xie S, Furjanic MA, Ferrara JJ, McAndrew NR, Ardino EL, Ngondara A, et al. The endocannabinoid system and rimonabant: a new drug with a novel mechanism of action involving cannabinoid CB1 receptor antagonism — or inverse agonism — as potential obesity treatment and other therapeutic use. J Clin Pharm Ther 2007; 32: 209–31.
Janero DR, Makriyannis A . Cannabinoid receptor antagonists: pharmacological opportunities, clinical experience, and translational prognosis. Expert Opin Emerg Drugs 2009; 14: 43–65.
Pertwee RG . Emerging strategies for exploiting cannabinoid receptor agonists as medicines. Br J Pharmacol 2009; 156: 397–411.
Di Marzo V, Szallasi A . Rimonabant in rats with a metabolic syndrome: good news after the depression. Br J Pharmacol 2008; 154: 915–7.
Scheen AJ, Paquot N . Use of cannabinoid CB1 receptor antagonists for the treatment of metabolic disorders. Best Pract Res Clin Endocrinol Metab 2009; 23: 103–16.
Nisoli E, Carruba MO . Emerging aspects of pharmacotherapy for obesity and metabolic syndrome. Pharmacol Res 2004; 50: 453–69.
Lee HK, Choi EB, Pak CS . The current status and future perspectives of studies of cannabinoid receptor 1 antagonists as anti-obesity agents. Curr Top Med Chem 2009; 9: 482–503.
Receveur JM, Murray A, Linget JM, Norregaard PK, Cooper M, Bjurling E, et al. Conversion of 4-cyanomethyl-pyrazole-3-carboxamides into CB1 antagonists with lowered propensity to pass the blood-brain-barrier. Bioorg Med Chem Lett 2010; 20: 453–7.
Pertwee RG . Inverse agonism and neutral antagonism at cannabinoid CB1 receptors. Life Sci 2005; 76: 1307–24.
Fong TM, Heymsfield SB . Cannabinoid-1 receptor inverse agonists: current understanding of mechanism of action and unanswered questions. Int J Obes (Lond) 2009; 33: 947–55.
Rinaldi-Carmona M, Barth F, Heaulme M, Shire D, Calandra B, Congy C, et al. SR141716A, a potent and selective antagonist of the brain cannabinoid receptor. FEBS Lett 1994; 350: 240–4.
Shearman LP, Stribling DS, Camacho RE, Rosko KM, Wang JY, Tong S, et al. Characterization of a novel and selective cannabinoid CB1 receptor inverse agonist, Imidazole 24b, in rodents. Eur J Pharmacol 2008; 579: 215–24.
Sink KS, McLaughlin PJ, Wood JA, Brown C, Fan P, Vemuri VK, et al. The novel cannabinoid CB1 receptor neutral antagonist AM4113 suppresses food intake and food-reinforced behavior but does not induce signs of nausea in rats. Neuropsychopharmacology 2008; 33: 946–55.
Chen W, Tang H, Liu H, Long L, Gong Z, Zheng J, et al. Novel selective antagonist of the cannabinoid CB1 receptor, MJ15, with prominent anti-obesity effect in rodent models. Eur J Pharmacol 2010; 637: 178–85.
Jagerovic N, Hernandez-Folgado L, Alkorta I, Goya P, Navarro M, Serrano A, et al. Discovery of 5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-3-hexyl-1h-1,2,4-triazole, a novel in vivo cannabinoid antagonist containing a 1,2,4-triazole motif. J Med Chem 2004; 47: 2939–42.
Pertwee RG, Joe-Adigwe G, Hawksworth GM . Further evidence for the presence of cannabinoid CB1 receptors in mouse vas deferens. Eur J Pharmacol 1996; 296: 169–72.
Christopoulos A, Coles P, Lay L, Lew MJ, Angus JA . Pharmacological analysis of cannabinoid receptor activity in the rat vas deferens. Br J Pharmacol 2001; 132: 1281–91.
Chen W, Zhou XB, Liu HY, Xu C, Wang LL, Li S . P633H, a novel dual agonist at peroxisome proliferator-activated receptors alpha and gamma, with different anti-diabetic effects in db/db and KK-Ay mice. Br J Pharmacol 2009; 157: 724–35.
Hsieh C, Brown S, Derleth C, Mackie K . Internalization and recycling of the CB1 cannabinoid receptor. J Neurochem 1999; 73: 493–501.
Lauckner JE, Hille B, Mackie K . The cannabinoid agonist WIN55,212-2 increases intracellular calcium via CB1 receptor coupling to Gq/11 G proteins. Proc Natl Acad Sci U S A 2005; 102: 19144–9.
Wang H, Dey SK, Maccarrone M . Jekyll and hyde: two faces of cannabinoid signaling in male and female fertility. Endocr Rev 2006; 27: 427–48.
Bosier B, Muccioli GG, Hermans E, Lambert DM . Functionally selective cannabinoid receptor signalling: therapeutic implications and opportunities. Biochem Pharmacol 2010; 80: 1–12.
Drysdale AJ, Ryan D, Pertwee RG, Platt B . Cannabidiol-induced intracellular Ca2+ elevations in hippocampal cells. Neuropharmacology 2006; 50: 621–31.
Sugiura T, Kodaka T, Kondo S, Tonegawa T, Nakane S, Kishimoto S, et al. 2-arachidonoylglycerol, a putative endogenous cannabinoid receptor ligand, induces rapid, transient elevation of intracellular free Ca2+ in neuroblastoma X glioma hybrid NG108-15 cells. Biochem Biophys Res Commun 1996; 229: 58–64.
Di Marzo V, Capasso R, Matias I, Aviello G, Petrosino S, Borrelli F, et al. The role of endocannabinoids in the regulation of gastric emptying: alterations in mice fed a high-fat diet. Br J Pharmacol 2008; 153: 1272–80.
Hildebrandt AL, Kelly-Sullivan DM, Black SC . Antiobesity effects of chronic cannabinoid CB1 receptor antagonist treatment in diet-induced obese mice. Eur J Pharmacol 2003; 462: 125–32.
Di Marzo V . The endocannabinoid system: its general strategy of action, tools for its pharmacological manipulation and potential therapeutic exploitation. Pharmacol Res 2009; 60: 77–84.
Di Marzo V, Matias I . Endocannabinoid control of food intake and energy balance. Nat Neurosci 2005; 8: 585–9.
Griffith DA, Hadcock JR, Black SC, Iredale PA, Carpino PA, DaSilva-Jardine P, et al. Discovery of 1-[9-(4-chlorophenyl)-8-(2-chlorophenyl)-9H-purin-6-yl]-4-ethylaminopiperi dine-4-carboxylic acid amide hydrochloride (CP-945,598), a novel, potent, and selective cannabinoid type 1 receptor antagonist. J Med Chem 2009; 52: 234–7.
Di Marzo V, Goparaju SK, Wang L, Liu J, Batkai S, Jarai Z, et al. Leptin-regulated endocannabinoids are involved in maintaining food intake. Nature 2001; 410: 822–5.
Rivera P, Romero-Zerbo Y, Pavon FJ, Serrano A, Lopez-Avalos MD, Cifuentes M, et al. Obesity-dependent cannabinoid modulation of proliferation in adult neurogenic regions. Eur J Neurosci 2011; 33: 1577–86.
Molhoj S, Hansen HS, Schweiger M, Zimmermann R, Johansen T, Malmlof K . Effect of the cannabinoid receptor-1 antagonist rimonabant on lipolysis in rats. Eur J Pharmacol 2010; 646: 38–45.
Thomas BF, Zhang Y, Brackeen M, Page KM, Mascarella SW, Seltzman HH . Conformational characteristics of the interaction of SR141716A with the CB1 cannabinoid receptor as determined through the use of conformationally constrained analogs. AAPS J 2006; 8: E665–71.
Acknowledgements
We gratefully acknowledge Prof Hua LI for her critical reading of the manuscript. This work was funded by Chinese National Hi-tech Research and Development Grants '863' (No 2003AA235010), the National Key Technologies R&D Program for New Drug of China (No 2009ZX09301-002) and the National Science and Technology Major Project of the Ministry of Science and Technology of China (No 2009ZX09501-031).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, W., Xu, C., Liu, Hy. et al. Novel selective cannabinoid CB1 receptor antagonist MJ08 with potent in vivo bioactivity and inverse agonistic effects. Acta Pharmacol Sin 32, 1148–1158 (2011). https://doi.org/10.1038/aps.2011.80
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2011.80