Abstract
Aim:
The present study investigated the effect of adenosine on Na+-K+ pumps in acutely isolated guinea pig (Cavia sp.) ventricular myocytes.
Methods:
The whole-cell, patch-clamp technique was used to record the Na+-K+ pump current (Ip) in acutely isolated guinea pig ventricular myocytes.
Results:
Adenosine inhibited the high DHO-affinity pump current (Ih) in a concentration-dependent manner, which was blocked by the selective adenosine A1 receptor antagonist DPCPX and the general protein kinase C (PKC) antagonists staurosporine, GF 109203X or the specific δ isoform antagonist rottlerin. In addition, the inhibitory action of adenosine was mimicked by a selective A1 receptor agonist CCPA and a specific activator peptide of PKC-δ, PP114. In contrast, the selective A2A receptor agonist CGS21680 and A3 receptor agonist Cl-IB-MECA did not affect Ih. Application of the selective A2A receptor antagonist SCH58261 and A3 receptor antagonist MRS1191 also failed to block the effect of adenosine. Furthermore, H89, a selective protein kinase A (PKA) antagonist, did not exert any effect on adenosine-induced Ih inhibition.
Conclusion:
The present study provides the electrophysiological evidence that adenosine can induce significant inhibition of Ih via adenosine A1 receptors and the PKC-δ isoform.
Similar content being viewed by others
Introduction
The Na+-K+ pump is a ubiquitous plasma membrane-bound enzyme that transports three Na+ for every two K+ into the cell by hydrolyzing ATP. Functional Na+-K+ pumps contain a catalytic α-subunit and a glycosylated β-subunit. The α-subunit alone binds Na+, K+, ATP, and cardiac glycosides. At present, four isoforms of the α-subunit (α1–α4) have been identified, and each has a unique tissue distribution1, 2. In guinea pig (Cavia sp.) ventricular myocytes, only the α1- and α2-isoforms, which correspond to the low- and high-affinity isoforms for cardiac glycosides, respectively, are expressed3, 4.
The Na+-K+ pump is subject to regulation by a variety of hormones or transmitters, including catecholamines, aldosterone, insulin, angiotensin, thyroid hormone and adenosine5, 6, 7, 8, 9. For instance, Alzamora et al5 demonstrated that aldosterone has a non-genomic effect on the Na+-K+ pump of vascular tissue, which is mediated by PKC activation. In patch-clamped guinea pig ventricular myocytes, Gao et al4 showed that the high DHO-affinity pump current (Ih) is regulated by α-adrenergic agonists via a PKC-dependent pathway, whereas the low DHO-affinity pump current (Il) is regulated by β-adrenergic agonists via a PKA-dependent pathway.
Adenosine, a purine nucleoside, is widely distributed in all tissues and body fluids. It is well known that adenosine exerts its cardiovascular effects by interacting with four types of G-protein coupled receptors (A1R, A2AR, A2BR, A3R)10. Considering that the regulatory effect of adenosine is a receptor-mediated process that involves the activation of PKA and PKC10, 11, 12, one would expect to find a potential regulatory effect of adenosine on the Na+-K+ pump. Indeed, several recent studies have been carried out to address this issue. However, these studies have yielded disparate results. Caruso-Neves et al6 demonstrated that in the Malpighian tubule cells of the blood-sucking bug Rhodnius prolixus, adenosine inhibited the Na+-K+ pump through interaction with the A1R. Krumschnabel et al13 have also reported adenosine A1R mediated Na+-K+ pump inhibition in the hepatocytes of goldfish (Carassius auratus) and trout (Oncorhynchus mykiss). These findings together suggest that the A1R may play a role in adenosine-induced Na+-K+ pump inhibition. In contrast, Darlington et al14 found an ultra-filtrate in plasma from mammalian species (dog, rat, calf) that could stimulate the Na+-K+ pump activity. They identified the stimulator to be adenosine and suggested that the effect of adenosine on the Na+-K+ pump was independent of adenosine receptors.
Given the lack of uniformity of these observations described above, the present study was designed to ascertain the effects of adenosine on the Na+-K+ pump in guinea pig ventricular myocytes and to further clarify the potential underlying mechanisms involved.
Materials and methods
Preparation of single ventricular myocytes
Adult guinea pigs (250–350 g) were purchased from Hebei Medical University Laboratorial Animal Center (Shijiazhuang, China). Single ventricular myocytes were enzymatically isolated as described in Gao et al15 with minor modifications. Briefly, hearts from anesthetized (sodium pentobarbitone, 120 mg/kg, ip) guinea pigs were excised quickly and perfused retrogradely through the aorta (about 8 mL/min) with oxygenated Ca2+-free Tyrode's solution (mmol/L): 137.7 NaCl, 2.3 NaOH, 5.4 KCl, 1 MgCl2, 5 Hepes, and 10 glucose (pH adjusted to 7.4 with NaOH) at 37 °C. After the perfusate was free of blood, the solution was changed to Ca2+-free Tyrode's solution containing 12 mg/mL collagenase (Serva, Heidelberg, Germany) for 10 min. Digested ventricles were thereafter cut into small species and agitated mechanically in high-K+ Kraft-Brühe (KB) solution to obtain single ventricular myocytes. The composition of the KB solution was (mmol/L): 83 KCl, 30 K2HPO4, 5 MgSO4, 2 KOH, 5 sodium pyruvic acid, 5 β-OH-butyric acid, 5 creatine, 20 taurine, 10 glucose, 0.5 EGTA, 5 Hepes, and 5 Na2-ATP (pH adjusted to 7.2 with KOH). The dissociated cells were then kept in KB solution at room temperature for at least 1 h before the experiment.
Electrophysiology
Cells were placed in the 0.3 mL superfusion chamber mounted on the stage of an inverted microscope (Nikon TE2000-S), allowed to attach to its glass bottom, and then superfused with the extracellular solution containing (mmol/L): 137.7 NaCl, 2.3 NaOH, 5.4 KCl, 1 MgCl2, 5 Hepes, 10 glucose, 2 BaCl2 and 1 CdCl2 (pH adjusted to 7.4 with NaOH). The chamber was perfused at a rate of about 2 mL/min and the solution exchange was complete within 2 min. The holding current was recorded using a whole-cell, patch-clamp technique and amplified using an Axopatch 700B amplifier (Axon Instruments). The sampling rate was 200 ms/point, and the data were low-pass filtered at 2 Hz. Patch electrodes were pulled with a Flaming/Brown micropipette puller (Sutter Instruments) and fire-polished to a final resistance of 1–3 MΩ when filled with the standard pipette solution, which contained (mmol/L) 50 sodium aspartic acid, 20 potassium aspartic acid, 30 CsOH, 20 TEACl, 5 MgSO4, 5 Hepes, 11 EGTA, 10 glucose, 5 Na2-ATP, 1 CaCl2 (pH adjusted to 7.2 with CsOH). Solutions were designed to minimize all other components of membrane current (K+ currents were blocked by replacing pipette K+ with Cs+ and TEA+ and adding Ba2+ to the extracellular solution; Ca2+ channel and Na+-Ca2+ exchanger currents were inhibited by including 1 mmol/L CdCl2 in the extracellular solution). Under these conditions, Ip was defined as the difference in currents before and after the addition of DHO, a specific and reversible inhibitor of the Na+-K+ pump. We voltage-clamped the myocytes to 0 mV, a saturating voltage for the Na+-K+ pump. For each experiment, both control and test Ip were obtained from the same cell to avoid cell-to-cell variability. For measurement of the voltage dependence of Ip, a voltage-ramp protocol going from +20 to −100 mV in a 4-s period was used in some experiments. This protocol was applied to each myocyte at least three times: (1) under control conditions, (2) during the adenosine effect on Ip and (3) after the Na+-K+ pump was blocked with DHO. The Ip values were obtained by digital subtraction of the membrane current in the presence of DHO from that in its absence at each test potential. All recordings were carried out at room temperature (22–25 °C) and data acquisition was achieved using pClamp 9.0 software.
Drugs
The drugs used in these studies and their abbreviations include CCPA, DPCPX, CGS-21680, Cl-IB-MECA, staurosporine (St), H89, adenosine (Ado), GF 109203X, MRS1191, dihydroouabain (DHO), Gö-6976, rottlerin, PP114, and SCH58261. All chemical reagents were purchased from Sigma Chemical Co (St Louis, MO, USA). Adenosine and DHO were dissolved in deionized water, and all other chemicals were dissolved in dimethylsulfoxide (DMSO) to prepare stock solutions that were stored at −20 °C. The final concentration of DMSO never exceeded 0.1%, which produced no detectable effect on Ip.
Data analysis and statistics
The data were analyzed with Clampfit 9.0 (Axon Instruments) and Origin 7.0 (Originlab Corporation) software. All values are presented as means±SEM. Statistical analysis of differences between two groups was carried out using Student's paired t-test. Two-way ANOVA was performed to determine significance between the voltage dependence curves. A value of P<0.05 was considered statistically significant.
Results
Adenosine specifically inhibits Ih in guinea pig ventricular myocytes
Il (α1-isoform related Ip) and Ih (α2-isoform related Ip) are distinguishable by their different sensitivities to cardiac glycosides, with 5 μmol/L DHO blocking Ih and 1 mmol/L DHO blocking Il3, 16. Experiments were carried out to determine the effects of adenosine on each of these two isoforms.
First, we examined the effect of adenosine on Ih. Figure 1A illustrates that a physiological concentration of adenosine (1 nmol/L)17, 18 decreased Ih from 16.1±0.3 pA (Ih (Con)) to 9.9±0.7 pA (Ih (Ado)) by 39% (n=8, P<0.05, upper panel). The decrease in Ip was not due to pump “rundown” because the adenosine effect was reversible upon washout (lower panel of Figure 1A). Figure 1B shows that adenosine inhibited Ih in a concentration-dependent manner from 1×10−11 to 1×10−5 mol/L (8% to 47%). Adenosine (1×10−8 mol/L) caused maximal inhibition. No significant effect was observed at concentrations of adenosine below 1×10−11 mol/L. The mean data from five to seven cells are shown in Figure 1C, where the percentage inhibition of Ih is plotted against the concentration of adenosine.
Adenosine inhibits Ih in guinea pig ventricular myocytes. (A) Upper panel: a typical trace showing the effect of 1 nmol/L adenosine on Ih. The lower and upper horizontal lines indicate the application of 5 μmol/L DHO and an adenosine-containing solution, respectively. The vertical bar illustrates the measured Ih amplitude. Lower panel: a typical trace showing that the adenosine effects on Ih were not due to pump “run-down”. (B) Representative traces of the effect of adenosine (1×10−11−1×10−5 mol/L) on Ih. (C) The percentage inhibition of Ih was plotted for each concentration of adenosine used. The error bars indicate means±SEM.
Next, we investigated the effect of adenosine on Il. The entire experiment was performed in the presence of 5 μmol/L DHO to block Ih, and Il was measured following the application of 1 mmol/L DHO. Figure 2A shows that adenosine did not change Il significantly [113.8±0.9 pA for Il (Ado), P>0.05 vs 115.4±0.7 pA for Il (Con), n=7]. In addition, increasing adenosine to 10 μmol/L had no effect on Il [91.2±0.8 pA for Il (Ado), P>0.05 vs 94.4±0.9 pA for Il (Con), n=10, Figure 2B]. These results indicate that the inhibitory effect of adenosine on the Na+-K+ pump current is specifically mediated via the Na+-K+ pump α2-isoform, so our subsequent studies were focused primarily on the effect of adenosine on Ih.
The adenosine-induced inhibition of Ih is voltage independent
Because Ip in guinea pig ventricular myocytes is voltage dependent16, we went further to examine the effect of adenosine on the Ih–Vm relationship. Figure 3A shows the voltage-ramp protocol applied to the myocytes. The relationships were normalized to the Ih recorded at 0 mV to facilitate comparison of their slopes, which are summarized in Figure 3B. The normalized Ih was generally lower in the presence of adenosine than that in its absence. The difference between these slopes was not statistically significant (n=6, P>0.05; two-way ANOVA). Thus, adenosine-induced Ih inhibition is voltage independent.
Inhibition of Ih by adenosine is mediated by A1 receptors
All four adenosine receptor subtypes are expressed in guinea pig ventricular myocytes, among which A1R is considered predominant19, 20. Thus, we tested whether adenosine inhibition of Ih was mediated by A1R. Figure 4A indicates that DPCPX (10 nmol/L), a selective A1R antagonist, had no effect on Ih by itself (upper panel), but completely abolished adenosine-induced Ih inhibition [7.8±0.5 pA for Ih (Ado), P<0.05 vs 14.7±0.3 pA for Ih (Con), and 14.1±0.6 pA for Ih (Ado+DPCPX), P>0.05 vs 14.7±0.3 pA for Ih (Con), n=8, lower panel]. In addition, CCPA (10 nmol/L), a selective agonist for A1R, produced a marked inhibition of Ih [7.8± 0.4 pA for Ih (CCPA), P<0.05 vs 15.7±0.3 pA for Ih (Con), n=9, Figure 4B]. In addition, the CCPA effect was absent in the presence of DPCPX (data not shown). These results strongly suggest that the effect of adenosine was the result of stimulation of the adenosine A1R.
Adenosine-induced inhibition of Ih is mediated by adenosine A1R, but not by A2AR or A3R. (A) Upper panel: a typical trace showing the effect of the A1R selective antagonist DPCPX (10 nmol/L) alone on Ih. Lower panel: a typical trace in the left panel showing the effect of adenosine on Ih in the presence and absence of DPCPX (10 nmol/L). The right panel shows a summary of the results. (B) A typical trace in the left panel showing the effect of the A1R selective agonist CCPA (10 nmol/L) on Ih. The right panel shows a summary of the results. (C, D) Typical traces in the left panels showing the effects of the A2AR and A3R selective agonists CGS21680 (0.2 μmol/L) and Cl-IB-MECA (0.5 μmol/L), respectively, on Ih. The right panels show summaries of the results. (E) A typical trace in the left panel showing the effect of adenosine on Ih in the presence and absence of the A2AR and A3R selective antagonists SCH58261 and MRS1191 (0.1 μmol/L each). The right panel shows a summary of the results. The error bars indicate means±SEM. bP<0.05 vs controls.
To investigate the possible participation of other adenosine receptor subtypes, the A2AR and A3R selective agonists CGS21680 and Cl-IB-MECA, respectively, were tested. As shown in Figure 4C, CGS21680 (0.2 μmol/L) had no significant effect on Ih [16.0±0.4 pA for Ih (CGS21680), P>0.05 vs 16.2±0.7 pA for Ih (Con), n=9]. Similarly, Cl-IB-MECA (0.5 μmol/L) had no effect on Ih [18.2±0.5 pA for Ih (Cl-IB-MECA), P>0.05 vs 18.5±0.6 pA for Ih (Con), n=9, Figure 4D]. We also observed that perfusion of adenosine, together with SCH58261 and MRS1191 (0.1 μmol/L each), the A2AR and A3R selective antagonists, respectively, did not alter the adenosine effect on Ih [11.8±0.6 pA for Ih (Ado), P<0.05 vs 22.1±0.5 pA for Ih (Con), and 10.3±0.8 pA for Ih (Ado+SCH58261+MRS1191), P<0.05 vs 22.1±0.5 pA for Ih (Con), n=9] (Figure 4E). It is, therefore, highly unlikely that A2AR and A3R are involved in adenosine-induced inhibition of Ih.
The activation of PKC-δ inhibits Ih
PKC is stimulated by A1R activation in ventricular myocytes11, 21. Therefore, we examined the effect of adenosine in the presence of staurosporine, a well-characterized PKC inhibitor. Perfusion of 1.5 μmol/L staurosporine alone did not modify Ih (data not shown) but completely abolished adenosine-induced Ih. inhibition [10.5±0.6 pA for Ih (Ado), P<0.05 vs 19.8±0.5 pA for Ih (Con), and 18.8±0.9 pA for Ih (Ado+St), P>0.05 vs 19.8±0.5 pA for Ih (Con), n=10, upper panel of Figure 5A]. Similar results were also obtained with GF 109203X, a highly specific PKC inhibitor. Adenosine did not inhibit Ih in the presence of 1 μmol/L GF 109203X [11.9±0.6 pA for Ih (Ado), P<0.05 vs 22.4±0.8 pA for Ih (Con), and 20.3±0.9 pA for Ih (Ado+GF 109203X), P>0.05 vs 22.4±0.8 pA for Ih (Con), n=8, lower panel of Figure 5A]. This reinforces the view that adenosine inhibits Ih through a PKC-dependent mechanism.
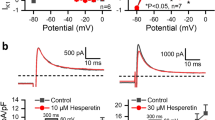
PKC-δ is primarily involved in the inhibitory effect of adenosine on Ih, whereas PKA is not involved. (A) Typical traces in the left panels showing the effects of adenosine on Ih in the presence and absence of the general PKC antagonists St (1.5 μmol/L, upper panel) or GF 109203X (1 μmol/L, lower panel). The right panels show summaries of the results. (B) Upper panel: a typical trace in the left panel showing the effect of adenosine on Ih in the presence and absence of the PKC-α and β inhibitor Gö-6976 (100 nmol/L). The right panel shows a summary of the results. Middle panel: a typical trace in the left panel showing the effect of adenosine on Ih in the presence and absence of the PKC-δ inhibitor rottlerin (10 μmol/L). The right panel shows a summary of the results. Lower panel: a typical trace in the left panel showing the effect of the PKC-δ activator PP114 (200 nmol/L) on Ih. The right panel shows a summary of the results. (C) A typical trace in the left panel showing the effect of adenosine on Ih in the presence and absence of the PKA antagonist H89 (1 μmol/L). The right panel shows a summary of the results. The error bars indicate means±SEM. bP<0.05 vs controls.
Because adult cardiomyocytes express multiple PKC isoforms22, we asked which one might be involved. We initially explored the role of the classical PKC isoforms (PKC-α and β) using the inhibitor Gö-6976. The upper panel of Figure 5B shows that adenosine still inhibited Ih in the presence of 100 nmol/L Gö-6976 [14.5±0.6 pA for Ih (Ado), P<0.05 vs 27.4±0.8 pA for Ih (Con), and 12.8±0.9 pA for Ih (Ado+Gö-6976), P<0.05 vs 27.4±0.8 pA for Ih (Con), n=8]. This indicates that classical PKC isoforms are not involved. Given the prominent role of PKC-δ during A1R activation by adenosine23, 24, we next examined the effect of rottlerin, a specific PKC-δ inhibitor, on the adenosine effect. Inhibition of PKC-δ with 10 μmol/L rottlerin completely abolished the effect of adenosine [12.9±0.6 pA for Ih (Ado), P<0.05 vs 24.4±0.8 pA for Ih (Con), and 22.3±0.8 pA for Ih (Ado+rottlerin), P>0.05 vs 24.4±0.8 pA for Ih (Con), n=8, middle panel of Figure 5B], indicating that PKC-δ is required for the adenosine effect on Ih. To confirm this, a specific activator peptide of PKC-δ, PP114, was used. Similar to adenosine, PP114 (200 nmol/L) caused a marked decrease in Ih [10.8±0.7 pA for Ih (PP114), P<0.05 vs 22.7±0.6 pA for Ih (Con), n=9, lower panel of Figure 5B]. The PP114 effect was also blocked by GF 109203X or rottlerin (data not shown). Taken together, these results indicate that PKC-δ plays a crucial role in the inhibition of Ih by adenosine.
To exclude the possible involvement of PKA in the adenosine-mediated Ih inhibition, the effect of adenosine was examined in the presence of H89, an inhibitor of PKA. Figure 5C shows that inhibition of PKA with 1 μmol/L H89 failed to abolish the effect of adenosine on Ih [11.0±0.6 pA for Ih (Ado), P<0.05 vs 20.7±0.4 pA for Ih (Con), and 10.9±0.8 pA for Ih (Ado+H89), P<0.05 vs 20.7±0.4 pA for Ih (Con), n=8]. Thus, PKA appears not to mediate Ih inhibition by adenosine.
Discussion
Numerous studies over the years have highlighted the isoform-specific modulation of Na+-K+ pumps by transmitters or kinases in many types of cells4, 25, 26. In this study, we found that the α2-isoform Na+-K+ pumps are specifically inhibited by adenosine. This implies a link among a specific adenosine receptor, its associated kinases, and inhibition of Ih in ventricular myocytes. In light of this, the goal of this study was to identify potential mechanisms by which adenosine exerts its effects on Ih.
We first examined which type of adenosine receptor is involved in this phenomenon. Considering that the adenosine concentration we used is close to that described for the high-affinity A1R (0.5–100 nmol/L)27, we speculate that the inhibitory effects of adenosine on the Na+-K+ pump are most likely mediated via the A1R. Indeed, using selective AR agonists and antagonists, we have demonstrated a specific role for A1R in adenosine-mediated Ih inhibition, whereas A2AR and A3R are not involved, in accordance with earlier studies using R prolixus and C auratus6, 13. There are two possible explanations for the above results. First, the A2AR is coupled to the cAMP-PKA pathway28, 29, which is targeted to the α1-isoform of the Na+-K+ pump4. Hence, A2AR activation could not lead to any change in Ih. A second possibility that may be pertinent to our results is the absence of functional A2AR or A3R proteins in cardiac myocytes10, 30. These two lines of evidence completely rule out the involvement of A2AR and A3R in the present study.
We next examined the possible mechanism(s) underlying Ih inhibition by A1R stimulation. Binding of adenosine to A1R inhibits adenyl cyclase and stimulates PKC via activation of the pertussis toxin sensitive G proteins Gi and/or Go28, 29. Using selective antagonists for PKC and PKA, we observed that the adenosine A1R triggers the PKC pathway to inhibit Ih, but the cAMP-PKA pathway is not involved. Specifically, this inhibition is predominantly mediated by the novel PKC-δ isoform. Our results are consistent with those of Gao et al4, who demonstrated that Ih was specifically regulated by PKC. However, in their study, Ih was increased by α-adrenoceptor stimulation via the PKC pathway, which is not congruent with our result showing a PKC-δ-mediated decrease in Ih. The most likely explanation for this discrepancy is the stimulation of different PKC isoforms by α-adrenoceptor activation. Indeed, we observed that α-adrenoceptor activation increases Ih in a PKC-β dependent manner using the inhibitor LY333531, which substantiates our results (data not shown). Taken together, these observations strongly suggest that adenosine-induced Ih inhibition is mediated by the PKC-δ isoform. The exact mechanisms for PKC-δ-mediated inhibition of Ih require further study, however, it most likely involves a phosphorylation-dependent process. In this case, PKC-δ may directly phosphorylate the pump protein to induce conformational changes, thus decreasing the turnover rate of each pump1, 31. In addition, the recent observation that phospholemman (FXYD1) associates with the cardiac Na+-K+ pump32 offers another subunit that may confer sensitivity to PKC-δ.
In conclusion, the major findings are that adenosine inhibits Ih via activation of A1R and PKC-δ. This finding may have implications for our understanding of the antiarrhythmic effect of adenosine when used clinically. The inhibition of Na+-K+ pump prolongs action potential duration and myocardial refractoriness, which is involved in the mechanisms of two other widely used antiarrhythmic agents, bretylium and amiodarone33, 34. Thus, it is tempting to speculate that the antiarrhythmic effects of adenosine are in part caused by Na+-K+ pump inhibition.
Author contribution
Yong-li WANG and Zhe ZHANG designed research; Zhe ZHANG and Hui-cai GUO performed research; Zhe ZHANG and Li-nan ZHANG analyzed data; Zhe ZHANG and Yong-li WANG wrote the paper.
References
Blanco G, Mercer RW . Isozymes of the Na-K-ATPase: heterogeneity in structure, diversity in function. Am J Physiol 1998; 275: F633–50.
Lopina OD . Na+, K+-ATPase: structure, mechanism, and regulation. Membr Cell Biol 2000; 13: 721–44.
Gao J, Mathias RT, Cohen IS, Baldo GJ . Two functionally different Na/K pumps in cardiac ventricular myocytes. J Gen Physiol 1995; 106: 995–1030.
Gao J, Wymore R, Wymore RT, Wang Y, McKinnon D, Dixon JE, et al. Isoform-specific regulation of the sodium pump by alpha- and beta-adrenergic agonists in the guinea-pig ventricle. J Physiol 1999; 516 (Pt 2): 377–83.
Alzamora R, Marusic E, Gonzalez M, Michea L . Nongenomic effect of aldosterone on Na+,K+-adenosine triphosphatase in arterial vessels. Endocrinology 2003; 144: 1266–72.
Caruso-Neves C, Monteiro SO, de Oliveira CF, Filho CC, Lopes AG . Adenosine modulates the Na+/K+ ATPase activity in malpighian tubules isolated from Rhodnius prolixus. Arch Insect Biochem Physiol 2000; 43: 72–7.
Hakam AC, Hussain T . Angiotensin II AT2 receptors inhibit proximal tubular Na+-K+-ATPase activity via a NO/cGMP-dependent pathway. Am J Physiol Renal Physiol 2006; 290: F1430–6.
Hansen PS, Buhagiar KA, Gray DF, Rasmussen HH . Voltage-dependent stimulation of the Na+-K+ pump by insulin in rabbit cardiac myocytes. Am J Physiol Cell Physiol 2000; 278: C546–53.
Sharabani-Yosef O, Nir U, Sampson SR . Thyroid hormone up-regulates Na+/K+ pump alpha2 mRNA but not alpha2 protein isoform in cultured skeletal muscle. Biochim Biophys Acta 2002; 1573: 183–8.
Peart JN, Headrick JP . Adenosinergic cardioprotection: multiple receptors, multiple pathways. Pharmacol Ther 2007; 114: 208–21.
Miura T, Liu Y, Kita H, Ogawa T, Shimamoto K . Roles of mitochondrial ATP-sensitive K channels and PKC in anti-infarct tolerance afforded by adenosine A1 receptor activation. J Am Coll Cardiol 2000; 35: 238–45.
Son YK, Park WS, Ko JH, Han J, Kim N, Earm YE . Protein kinase A-dependent activation of inward rectifier potassium channels by adenosine in rabbit coronary smooth muscle cells. Biochem Biophys Res Commun 2005; 337: 1145–52.
Krumschnabel G, Biasi C, Wieser W . Action of adenosine on energetics, protein synthesis and K+ homeostasis in teleost hepatocytes. J Exp Biol 2000; 203: 2657–65.
Darlington DN, Gann DS . Adenosine stimulates NA/K ATPase and prolongs survival in hemorrhagic shock. J Trauma 2005; 58: 1–6.
Gao J, Mathias RT, Cohen IS, Baldo GJ . Isoprenaline, Ca2+ and the Na+-K+ pump in guinea-pig ventricular myocytes. J Physiol 1992; 449: 689–704.
Gadsby DC, Nakao M . Steady-state current-voltage relationship of the Na/K pump in guinea pig ventricular myocytes. J Gen Physiol 1989; 94: 511–37.
Deussen A, Stappert M, Schafer S, Kelm M . Quantification of extracellular and intracellular adenosine production: understanding the transmembranous concentration gradient. Circulation 1999; 99: 2041–7.
Gorman MW, Wangler RD, Bassingthwaighte JB, Mohrman DE, Wang CY, Sparks HV . Interstitial adenosine concentration during norepinephrine infusion in isolated guinea pig hearts. Am J Physiol 1991; 261: H901–9.
Cook MA, Karmazyn M . Cardioprotective actions of adenosine and adenosine analogs. Exs 1996; 76: 325–44.
Thomas GP, Sims SM, Cook MA, Karmazyn M . Hydrogen peroxide-induced stimulation of L-type calcium current in guinea pig ventricular myocytes and its inhibition by adenosine A1 receptor activation. J Pharmacol Exp Ther 1998; 286: 1208–14.
Parsons M, Young L, Lee JE, Jacobson KA, Liang BT . Distinct cardioprotective effects of adenosine mediated by differential coupling of receptor subtypes to phospholipases C and D. FASEB J 2000; 14: 1423–31.
Mackay K, Mochly-Rosen D . Localization, anchoring, and functions of protein kinase C isozymes in the heart. J Mol Cell Cardiol 2001; 33: 1301–7.
Henry P, Demolombe S, Puceat M, Escande D . Adenosine A1 stimulation activates delta-protein kinase C in rat ventricular myocytes. Circ Res 1996; 78: 161–5.
Kudo M, Wang Y, Xu M, Ayub A, Ashraf M . Adenosine A1 receptor mediates late preconditioning via activation of PKC-delta signaling pathway. Am J Physiol Heart Circ Physiol 2002; 283: H296–301.
Brodsky JL . Insulin activation of brain Na+-K+-ATPase is mediated by alpha 2-form of enzyme. Am J Physiol 1990; 258: C812–7.
Gertsberg I, Brodsky I, Priel Z, Danilenko M . Na+-K+-ATPase in frog esophagus mucociliary cell membranes: inhibition by protein kinase C activation. Am J Physiol 1997; 273: C1842–8.
Fredholm BB, Abbracchio MP, Burnstock G, Daly JW, Harden TK, Jacobson KA, et al. Nomenclature and classification of purinoceptors. Pharmacol Rev 1994; 46: 143–56.
Headrick JP, Hack B, Ashton KJ . Acute adenosinergic cardioprotection in ischemic-reperfused hearts. Am J Physiol Heart Circ Physiol 2003; 285: H1797–818.
Mubagwa K, Flameng W . Adenosine, adenosine receptors and myocardial protection: an updated overview. Cardiovasc Res 2001; 52: 25–39.
Kilpatrick EL, Narayan P, Mentzer RM Jr, Lasley RD . Cardiac myocyte adenosine A2a receptor activation fails to alter cAMP or contractility: role of receptor localization. Am J Physiol Heart Circ Physiol 2002; 282: H1035–40.
Gao J, Wymore RS, Wang Y, Gaudette GR, Krukenkamp IB, Cohen IS, et al. Isoform-specific stimulation of cardiac Na/K pumps by nanomolar concentrations of glycosides. J Gen Physiol 2002; 119: 297–312.
Crambert G, Fuzesi M, Garty H, Karlish S, Geering K . Phospholemman (FXYD1) associates with Na, K-ATPase and regulates its transport properties. Proc Natl Acad Sci USA 2002; 99: 11476–81.
Gatto C, Barkulis CT, Schneider WR, Holden JP, Arnett KL, Milanick MA . Inhibition of the Na,K-ATPase by the antiarrhythmic drug, Bretylium. Ann N Y Acad Sci 2003; 986: 620–2.
Gray DF, Mihailidou AS, Hansen PS, Buhagiar KA, Bewick NL, Rasmussen HH, et al. Amiodarone inhibits the Na+-K+ pump in rabbit cardiac myocytes after acute and chronic treatment. J Pharmacol Exp Ther 1998; 284: 75–82.
Acknowledgements
This project was supported by the Natural Science Foundation of Hebei Province (No 30200030).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Z., Guo, Hc., Zhang, Ln. et al. Isoform-specific regulation of the Na+-K+ pump by adenosine in guinea pig ventricular myocytes. Acta Pharmacol Sin 30, 404–412 (2009). https://doi.org/10.1038/aps.2009.26
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.26