Abstract
Social and medical issues regarding prenatal diagnosis in Luxembourg are addressed. The organisation and the overall impact of amniocentesis on aneuploid births are described. Legal aspects are discussed as are future developments.
Similar content being viewed by others
Introduction
The population of the Grand Duchy of Luxembourg falls just short of 400,000 inhabitants with roughly 5,000 births per year. Until 1994, the Social Security did not provide reimbursement of either amniocentesis (AC) or fetal karyotyping. This seriously hampered prenatal diagnosis (PND) and was a major reason why the National Health Laboratory, providing chromosomal analysis since the late sixties, started offering fetal karyotypes as late as 1989 on the few amniocenteses performed locally. By now, more than 95% of the reimbursed prenatal chromosome analyses are done at this single site.
Due to stipulations of the national pregnancy surveillance programme, five medical examinations by a gynaecologist are mandatory for prenatal allocations, thus virtually excluding general practitioners from prenatal care. This programme includes three ultrasounds, one for each trimester.
Organisation
Fetal karyotyping is carried out by the National Health Laboratory for all pregnancies qualifying for PND reimbursed by the Social Security. It also centralises all chromosomal analyses for malformations diagnosed at birth and later in life. For molecular analysis, the vast majority of samples are transferred to university facilities mostly in France or Belgium.
All gynaecologists are entitled to sample amniotic fluid, but de facto 67% of all AC are performed by 9 practitioners and close to 20% by 1 among them. There is a definite trend to refer AC to a few performers.
The triple test, on a paying basis, is done in a single hospital laboratory or at the University of Liège (Prof. Koulischer).
Genetic counselling is provided biweekly at the Centre Hospitalier de Luxembourg. Counselling after a positive finding is given at the Department of Cytogenetics.
Sources of Information
There is no national registry for congenital abnormalities, genetic disorders or PND in Luxembourg. From 1980 to 1989, Luxembourg contributed data to the EUROCAT registry for congenital anomalies and genetic diseases.
The National Health Laboratory keeps files on prenatal and neonatal karyotyping carried out at its site. The latter are comprehensive figures. Demographic data are kindly provided by the National Statistics Office (STATEC).
Impact of PND
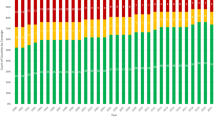
Demographic data in Luxembourg, as elsewhere in Europe, show a definite trend to later birth giving in the 1990s compared to the preceding decade (fig. 1). As a result, more children are born to mothers aged over 35 years, from 6.4% in 1980 to 12.1% in 1995 (fig. 2).
Prenatal screening for common aneuploidies, like Down’s syndrome and trisomies 18 and 13, was delayed in Luxembourg due to the non-reimbursement of both fetal karyotyping and the triple test.
Starting in 1989, the National Health Laboratory offered free fetal karyotyping for pregnant women over 35, thus giving even socially disadvantaged mothers-to-be free access to prenatal screening for Down’s syndrome. The Social Security started reimbursing AC and fetal karyotypes, for women over 35 or presenting a specific risk factor, in 1994. The triple test is only available on a paying basis.
The possible impact of the local screening policy on Down’s syndrome at birth, in women aged over 35 is done by comparing official birth data with neonatal karyotype results.
While the prevalence of Down’s syndrome in women under 35 years remains unchanged at a median of 0.9 ± 0.4 for 1,000 births, it decreased from 12/1,000 in 1986 to 0/1,000 in the last 3 years, following a steady downward trend beginning in 1988 (fig. 3).
Figures for trisomies 13 and 18 are too small for analysis. Nonetheless, no live-birth was observed for these aneuploidies in the last 4 years while from 1 to 3 were expected. In the same period, fetal karyotyping detected 1 trisomy 18. Fetal karyotyping for pregnancies in women over 35 years achieved a dramatic reduction of trisomic births in the considered age class. No similar evolution is observed in younger women in spite of the fact that at least 25% undergo serum testing.
Other trisomies detected prenatally from 1992 to 1995: 47,XXX (1), 47+18 (1), 46,XXY (2), 45,XO (2), 69,XXY (1). No data are available for non-chromosomal congenital anomalies.
Available Diagnostic Procedures
Ultrasound screening is used by all attending gynaecologists. As no level 3 ultrasound is available in the country, a regional arrangement with nearby Metz (France) covers this need.
The Social Security does not pay for serum marker screening. It is offered in one private hospital laboratory on a paying basis or handed over to the Liège University, depending on the gynaecologist’s choice.
α-Fetoprotein (AFP) screening is widely available and used.
AC is offered in all 6 obstetric centres of the country.
Fetal chromosome analysis is performed at the National Health Laboratory for the following indications: maternal age over 35 years or balanced chromosomal rearrangement in parents, aneuploidy in collaterals, chromosomal disease in close family, abnormalities detected by ultrasound and elevated relative risk according to serum markers.
Choriocentesis and cordocentesis are referred to foreign university centres. Professional guidelines are lacking for both gynaecologists and cytogenetists.
Current Methods in Use for PND
Level 1 ultrasound screening is widely used.
Fetal cell sampling is performed nearly exclusively by AC; choriocentesis is an exceptional procedure. Chordocentesis is offered as a back-up method whenever a second chromosomal analysis is considered.
All amniotic fluids are routinely analysed for AFP and on request for AChE. Conventional banding methods are used for fetal karyotyping. Fluorescence in situ hybridization (FISH) is considered whenever structural rearrangements or microdeletions have to be characterised.
Areas under Development
FISH on interphase nuclei is under development. A comprehensive policy for serum marker screening in women under 35 and a screening programme for cystic fibrosis in affected families is currently being discussed.
Funding Arrangements for PND
As of January 1994, the Social Security pays for the following procedures: ultrasound limited to three for normal pregnancies, AFP determination, fetal karyotype for given indications except after triple test karyotype, and for all procedures referred to a foreign country, namely choriocentesis, cordocentesis, level 2 and 3 ultrasound and molecular biology, screening for relevant feto-maternal infectious agents. The triple test is not reimbursed as such, whereas the three markers taken individually are.
Current Legislation Surrounding PND
Termination of Pregnancy
According to a law passed November 15, 1975, termination of pregnancy is legal during the first 12 weeks of pregnancy: if the pregnancy may endanger the physical or psychic health of the mother, if a serious risk exists for the fetus to present a serious disease, malformations or important psychic alterations, if the pregnancy may be considered as consecutive to a rape.
The woman is requested to consult with a gynaecologist to be informed about potential risks and must give a written consent.
After week 12, two qualified physicians have to certify that a ‘very serious risk’ to the health or the life of the pregnant woman or her child exists. No time limit for termination is given by the law. The Social Security is obliged to cover medical expenses of termination.
Pre-implantation Diagnosis
No legal text covers this issue.
Problems to Face and Future Developments
Luxembourg lacks professional guidelines for all parties engaged in PND. Medically assisted procreation evolves in an absolute legal vacuum. The politically and economically responsible parties are very slow to agree on a comprehensive strategy for prenatal screenings.
Genetic counselling is embryonic at best. No parents’ associations for genetically damaged children are available for informing parents-to-be about upcoming problems while rising a severely handicapped child or about the joy to do so.
The size and the relative stability of the population call for a national surveillance strategy for chromosomal and Mendelian diseases and malformations.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Schneider, F.C. Prenatal Diagnosis in Luxembourg. Eur J Hum Genet 5 (Suppl 1), 48–50 (1997). https://doi.org/10.1007/BF03405961
Issue Date:
DOI: https://doi.org/10.1007/BF03405961