Abstract
Objective:
Previous reports suggest a benefit of fluconazole prophylaxis in extremely low birth weight (ELBW) infants <1000 g. Our aim was to evaluate if limiting fluconazole prophylaxis to targeted highest risk infants effectively prevents invasive fungal infections, has no undesired side effects and limits unnecessary drug exposure.
Study Design:
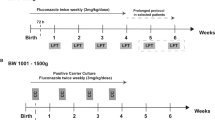
This nonrandomized retrospective pre-post intervention study compared two groups of infants: (1) Infants <26 weeks gestation and/or <750 g birth weight, requiring central vascular access and admitted to the Monroe Carell Jr Children's Hospital at Vanderbilt neonatal intensive care unit (NICU) prior to 5 days of age, who received fluconazole prophylaxis and (2) a matched control group from the year prior to prophylaxis. This target population was selected for fluconazole prophylaxis based on prior infection control data from our institution and a number needed to treat of <15 to prevent one episode of fungemia. Following implementation and integration through the institution's computerized physician order entry (CPOE) system, provider adherence to the protocol was assessed during the prophylaxis period.
Result:
A total of 86 patients were included in the study, 44 in the no-prophylaxis group and 42 in the prophylaxis group. In the targeted prophylaxis group, no invasive fungal infections were observed as compared to nine infants with invasive infections in the no-prophylaxis group (P=0.004). No significant adverse effects were recorded. Targeting the highest risk infants reduced the number of infants <1000 g requiring prophylaxis from 80 to 42 (48% reduction) with no preventable infection missed. Provider compliance was 91% following implementation of this protocol through the CPOE system using a standardized order set.
Conclusion:
Targeting the highest risk infants for fluconazole prophylaxis through CPOE can effectively prevent invasive fungal infections and limit drug exposure with no unwanted side effects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 2002; 110: 285–291.
Feja KN, Wu F, Roberts K, Loughrey M, Nesin M, Larson E et al. Risk factors for candidemia in critically ill infants: a matched case-control study. J Pediatr 2005; 147: 156–161.
Saiman L, Ludington E, Pfaller M, Rangel-Frausto S, Wiblin RT, Dawson J et al. Risk factors for candidemia in Neonatal Intensive Care Unit patients. The National Epidemiology of Mycosis Survey Study Group. Pediatr Infect Dis J 2000; 19: 319–324.
Benjamin Jr DK, Ross K, McKinney Jr RE, Benjamin DK, Auten R, Fisher RG . When to suspect fungal infection in neonates: a clinical comparison of Candida albicans and Candida parapsilosis fungemia with coagulase-negative staphylococcal bacteremia. Pediatrics 2000; 106: 712–718.
Baley JE, Kliegman RM, Boxerbaum B, Fanaroff AA . Fungal colonization in the very low birth weight infant. Pediatrics 1986; 78: 225–232.
Saiman L, Ludington E, Dawson JD, Patterson JE, Rangel-Frausto S, Wiblin RT et al. Risk factors for Candida species colonization of neonatal intensive care unit patients. Pediatr Infect Dis J 2001; 20: 1119–1124.
Kaufman D, Kaufman D, Boyle R, Hazen KC, Patrie JT, Robinson M et al. Fluconazole prophylaxis against fungal colonization and infection in preterm infants. N Engl J Med 2001; 345: 1660–1666.
Smith PB, Morgan J, Benjamin JD, Fridkin SK, Sanza LT, Harrison LH et al. Excess costs of hospital care associated with neonatal candidemia. Pediatr Infect Dis J 2007; 26: 197–200.
Kaufman D, Boyle R, Hazen KC, Patrie JT, Robinson M, Grossman LB . Twice weekly fluconazole prophylaxis for prevention of invasive Candida infection in high-risk infants of <1000 grams birth weight. J Pediatr 2005; 147: 172–179.
Healy CM, Baker CJ, Zaccaria E, Campbell JR . Impact of fluconazole prophylaxis on incidence and outcome of invasive candidiasis in a neonatal intensive care unit. J Pediatr 2005; 147: 166–171.
Bertini G, Perugi S, Dani C, Filippi L, Pratesi S, Rubaltelli FF . Fluconazole prophylaxis prevents invasive fungal infection in high-risk, very low birth weight infants. J Pediatr 2005; 147: 162–165.
Manzoni P, Arisio R, Mostert M, Leonessa M, Farina D, Latino MA et al. Prophylactic fluconazole is effective in preventing fungal colonization and fungal systemic infections in preterm neonates: a single-center, 6-year, retrospective cohort study. Pediatrics 2006; 117: e22–e32.
McCrossan BA, McHenry E, O'Neil F, Ong G, Sweet DG . Selective fluconazole prophylaxis in high risk babies to reduce invasive fungal infection. Arch Dis Child Fetal Neonatal Ed 2007; 92: F454–F458.
Uko S, Soghier LM, Vega M, Marsh J, Reinersman GT, Herring L et al. Targeted short-term fluconazole prophylaxis among very low birth weight and extremely low birth weight infants. Pediatrics 2006; 117: 1243–1252.
Manzoni P, Stolfi I, Pugni L, Decembrino L, Magnani C, Vetrano G et al. A multicenter, randomized trial of prophylactic fluconazole in preterm neonates. N Engl J Med 2007; 356: 2483–2495.
Aghai ZH, Mudduluru M, Nakhla TA, Amendolia B, Longo D, Kemble N et al. Fluconazole prophylaxis in extremely low birth weight infants: association with cholestasis. J Perinatol 2006; 26: 550–555.
McGuire W, Clerihew L, Austin N . Prophylactic intravenous antifungal agents to prevent mortality and morbidity in very low birth weight infants. Cochrane Database Syst Rev 2004; (1): CD003850.
Martinez Sesmero JM, Farfan Sedano FJ, Molina Garcia T, Brussi MM, Sanchez-Rubio Ferrandez J, Diez Fernandez R et al. Fungal chemoprophylaxis with fluconazole in preterm infants. Pharm World Sci 2005; 27: 475–477.
Alangaden G, Chandrasekar PH, Bailey E, Khaliq Y . Antifungal prophylaxis with low-dose fluconazole during bone marrow transplantation. The Bone Marrow Transplantation Team. Bone Marrow Transplant 1994; 14: 919–924.
Playford EG, Webster AC, Sorell TC, Craig JC . Antifungal agents for preventing fungal infections in solid organ transplant recipients. Cochrane Database Syst Rev 2004; (3): CD004291.
Burwell LA, Kaufman D, Blakely J, Stoll BJ, Fridkin SK . Antifungal prophylaxis to prevent neonatal candidiasis: a survey of perinatal physician practices. Pediatrics 2006; 118: e1019–e1026.
Long SS, Stevenson DK . Reducing Candida infections during neonatal intensive care: management choices, infection control, and fluconazole prophylaxis. J Pediatr 2005; 147: 135–141.
Fanaroff AA . Fluconazole for the prevention of fungal infections: get ready, get set, caution. Pediatrics 2006; 117: 214–215.
Fridkin SK, Kaufman D, Edwards JR, Shetty S, Horan T . Changing incidence of Candida bloodstream infections among NICU patients in the United States: 1995–2004. Pediatrics 2006; 117: 1680–1687.
Rangel-Frausto MS, Wiblin T, Blumberg HM, Saiman L, Patterson J, Rinaldi M et al. National epidemiology of mycoses survey (NEMIS): variations in rates of bloodstream infections due to Candida species in seven surgical intensive care units and six neonatal intensive care units. Clin Infect Dis 1999; 29: 253–258.
Lin MY, Carmeli Y, Zumsteg J, Flores EL, Tolentino J, Sreeramoju P et al. Prior antimicrobial therapy and risk for hospital-acquired Candida glabrata and Candida krusei fungemia: a case-case-control study. Antimicrob Agents Chemother 2005; 49: 4555–4560.
Novelli V, Holzel H . Safety and tolerability of fluconazole in children. Antimicrob Agents Chemother 1999; 43: 1955–1960.
Acknowledgements
We thank Steven Steele, RN, for his assistance in data retrieval for this study. We thank Russell Waitman, PhD and the Vanderbilt WizOrder Team for their continued CPOE support as well as William Walsh, MD and Judy Aschner, MD, for review of the manuscript and helpful discussions. This study has been acknowledged by the Vanderbilt Infection Prevention (VIP) award to one of the authors (JHW).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weitkamp, JH., Ozdas, A., LaFleur, B. et al. Fluconazole prophylaxis for prevention of invasive fungal infections in targeted highest risk preterm infants limits drug exposure. J Perinatol 28, 405–411 (2008). https://doi.org/10.1038/sj.jp.7211914
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211914
Keywords
This article is cited by
-
Updates in the Pharmacologic Prophylaxis and Treatment of Invasive Candidiasis in the Pediatric and Neonatal Intensive Care Units
Current Treatment Options in Infectious Diseases (2022)
-
Meningitis, urinary tract, and bloodstream infections in very low birth weight infants enrolled in a heart rate characteristics monitoring trial
Pediatric Research (2020)
-
Prevention of Invasive Candidiasis in Premature Neonates: Administering Fluconazole or Not?
Current Fungal Infection Reports (2018)
-
Fluconazole prophylaxis is associated with a decreased rate of coagulase-negative Staphylococcal infections in a subset of extremely low birth weight neonates
Medical Microbiology and Immunology (2014)
-
Safety of fluconazole in paediatrics: a systematic review
European Journal of Clinical Pharmacology (2013)