Abstract
Objective
To determine rates of late-onset infection (LOI) during postnatal days 3–7 among preterm infants, based on antibiotic exposure during days 0–2.
Study design
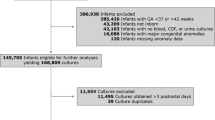
Retrospective cohort study of infants born <1500 grams and ≤30 weeks gestation, 2005–2018. We analyzed the incidence and microbiology of LOI at days 3–7 based on antibiotic exposure during postnatal days 0–2.
Results
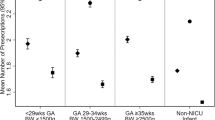
The cohort included 88,574 infants, of whom 85% were antibiotic-exposed. Fewer antibiotic-exposed compared to unexposed infants developed LOI (1.5% vs. 2.1%; adjusted hazard ratio, 0.28, 95% CI 0.24–0.33). Among antibiotic-exposed compared to unexposed infants, Gram-negative (38% vs. 28%, p = 0.002) and fungal (11% vs. 1%, p < 0.001) species were more commonly isolated, and gram-positive organisms (49% vs. 70%, p < 0.001) were less commonly isolated.
Conclusions
We observed low overall rates of LOI at days 3–7 after birth, but antibiotic exposure from birth was associated with lower rates, and with differing microbiology, compared to no exposure.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The dataset analyzed during the current study derives from the Pediatrix Medical Group database and is not publicly available.
References
Stoll BJ, Puopolo KM, Hansen NI, Sánchez PJ, Bell EF, Carlo WA, et al. Early-onset neonatal sepsis 2015 to 2017, the rise of Escherichia coli, and the need for novel prevention strategies. JAMA Pediatr. 2020;174:e200593.
Flannery DD, Edwards EM, Puopolo KM, Horbar JD. Early-onset sepsis among very preterm infants. Pediatrics. 2021;148:2021052456.
Flannery DD, Ross RK, Mukhopadhyay S, Tribble AC, Puopolo KM, Gerber JS. Temporal trends and center variation in early antibiotic use among premature infants. JAMA Netw Open. 2018;1:e180164.
Kuppala VS, Meinzen-Derr J, Morrow AL, Schibler KR. Prolonged initial empirical antibiotic treatment is associated with adverse outcomes in premature infants. J Pediatr. 2011;159:720–5.
Cantey JB, Huffman LW, Subramanian A, Marshall AS, Ballard AR, Lefevre C, et al. Antibiotic exposure and risk for death or bronchopulmonary dysplasia in very low birth weight infants. J Pediatr. 2017;181:289–93.e1.
Ting JY, Roberts A, Sherlock R, Ojah C, Cieslak Z, Dunn M, et al. Duration of initial empirical antibiotic therapy and outcomes in very low birth weight infants. Pediatrics. 2019;143:e20182286.
Letouzey M, Lorthe E, Marchand-Martin L, Kayem G, Charlier C, Butin M, et al. Early antibiotic exposure and adverse outcomes in very preterm infants at low risk of early-onset sepsis: the EPIPAGE-2 cohort study. J Pediatr. 2022;243:91–8.e4.
Cotten CM, Taylor S, Stoll B, Goldberg RN, Hansen NI, Sanchez PJ, et al. Prolonged duration of initial empirical antibiotic treatment is associated with increased rates of necrotizing enterocolitis and death for extremely low birth weight infants. Pediatrics. 2009;123:58–66.
Gasparrini AJ, Crofts TS, Gibson MK, Tarr PI, Warner BB, Dantas G. Antibiotic perturbation of the preterm infant gut microbiome and resistome. Gut Microbes. 2016;7:443–9.
Ramirez CB, Cantey JB. Antibiotic resistance in the neonatal intensive care unit. Neoreviews. 2019;20:e135–44.
Patel SJ, Oshodi A, Prasad P, Delamora P, Larson E, Zaoutis T, et al. Antibiotic use in neonatal intensive care units and adherence with centers for disease control and prevention 12 step campaign to prevent antimicrobial resistance. Pediatr Infect Dis J. 2009;28:1047–51.
Garber SJ, Dhudasia MB, Flannery DD, Passarella MR, Puopolo KM, Mukhopadhyay S. Delivery-based criteria for empiric antibiotic administration among preterm infants. J Perinatol. 2021;41:255–62.
Puopolo KM, Benitz WE, Zaoutis TE. Management of neonates born at ≤34 6/7 weeks’ gestation with suspected or proven early-onset bacterial sepsis. Pediatrics. 2018;142:e20182896.
Puopolo KM, Mukhopadhyay S, Hansen NI, Cotten CM, Stoll BJ, Sanchez PJ, et al. Identification of extremely premature infants at low risk for early-onset sepsis. Pediatrics. 2017;140:e20170925.
Flannery DD, Mukhopadhyay S, Morales KH, Dhudasia MB, Passarella M, Gerber JS, et al. Delivery characteristics and the risk of early-onset neonatal sepsis. Pediatrics. 2022;149:e2021052900.
Mukhopadhyay S, Puopolo KM. Clinical and microbiologic characteristics of early-onset sepsis among very low birth weight infants: opportunities for antibiotic stewardship. Pediatr Infect Dis J. 2017;36:477–81.
Spitzer AR, Ellsbury D, Clark RH. The Pediatrix BabySteps® Data Warehouse—a unique national resource for improving outcomes for neonates. Indian J Pediatr. 2015;82:71–9.
Clark RH, Gordon P, Walker WM, Laughon M, Smith PB, Spitzer AR. Characteristics of patients who die of necrotizing enterocolitis. J Perinatol. 2012;32:199–204.
Attridge JT, Clark R, Walker MW, Gordon PV. New insights into spontaneous intestinal perforation using a national data set: (2) two populations of patients with perforations. J Perinatol. 2006;26:185–8.
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS. New intrauterine growth curves based on United States data. Pediatrics. 2010;125:e214–24.
Vidavalur R, Hussain N. Interstate practice variation and factors associated with antibiotic use for suspected neonatal sepsis in the United States. Am J Perinatol. 2023. https://doi.org/10.1055/a-2061-8620.
Boghossian NS, Geraci M, Lorch SA, Phibbs CS, Edwards EM, Horbar JD. Racial and ethnic differences over time in outcomes of infants born less than 30 weeks’ gestation. Pediatrics. 2019;144:e20191106.
Le J, Greenberg RG, Benjamin DK, Yoo YJ, Zimmerman KO, Cohen-Wolkowiez M, et al. Prolonged post-discontinuation antibiotic exposure in very low birth weight neonates at risk for early-onset sepsis. J Pediatr Infect Dis Soc. 2021;10:615–21.
Mukhopadhyay S, Briker SM, Flannery DD, Dhudasia MB, Coggins SA, Woodford E, et al. Time to positivity of blood cultures in neonatal late-onset bacteraemia. Arch Dis Child Fetal Neonatal Ed. 2022;107:583–8.
Scheer CS, Fuchs C, Gründling M, Vollmer M, Bast J, Bohnert JA, et al. Impact of antibiotic administration on blood culture positivity at the beginning of sepsis: a prospective clinical cohort study. Clin Microbiol Infect. 2019;25:326–31.
Gibson MK, Crofts TS, Dantas G. Antibiotics and the developing infant gut microbiota and resistome. Curr Opin Microbiol. 2015;27:51–6.
Mukhopadhyay S, Lee J-J, Hartman E, Woodford E, Dhudasia MB, Mattei LM, et al. Preterm infants at low risk for early-onset sepsis differ in early fecal microbiome assembly. Gut Microbes. 2022;14:2154091.
Cotten CM, McDonald S, Stoll B, Goldberg RN, Poole K, Benjamin DK. The association of third-generation cephalosporin use and invasive candidiasis in extremely low birth-weight infants. Pediatrics. 2006;118:717–22.
Yu Y, Du L, Yuan T, Zheng J, Chen A, Chen L, et al. Risk factors and clinical analysis for invasive fungal infection in neonatal intensive care unit patients. Am J Perinatol. 2013;30:589–94.
Benjamin DK, Stoll BJ, Gantz MG, Walsh MC, Sánchez PJ, Das A, et al. Neonatal candidiasis: epidemiology, risk factors, and clinical judgment. Pediatrics. 2010;126:e865.
Ficara M, Pietrella E, Spada C, Della Casa Muttini E, Lucaccioni L, Iughetti L, et al. Changes of intestinal microbiota in early life. J Matern Fetal Neonatal Med. 2020;33:1036–43.
Gibson MK, Wang B, Ahmadi S, Burnham C-AD, Tarr PI, Warner BB, et al. Developmental dynamics of the preterm infant gut microbiota and antibiotic resistome. Nat Microbiol. 2016;1:16024.
Greenwood C, Morrow AL, Lagomarcino AJ, Altaye M, Taft DH, Yu Z, et al. Early empiric antibiotic use in preterm infants is associated with lower bacterial diversity and higher relative abundance of Enterobacter. J Pediatr. 2014;165:23–9.
Zhu D, Xiao S, Yu J, Ai Q, He Y, Cheng C, et al. Effects of one-week empirical antibiotic therapy on the early development of gut microbiota and metabolites in preterm infants. Sci Rep. 2017;7:8025.
Polin RA, Papile LA, Baley JE, Benitz W, Carlo WA, Cummings J, et al. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics. 2012;129:1006–15.
Greenberg RG, Chowdhury D, Hansen NI, Smith PB, Stoll BJ, Sánchez PJ, et al. Prolonged duration of early antibiotic therapy in extremely premature infants. Pediatr Res. 2019;85:994–1000.
Funding
SAC reports receiving research funding from the National Heart, Lung and Blood Institute of the National Institutes of Health (T32HL007891). KMP reports receiving research funding from the National Institutes of Health, from two contracts with the Centers for Disease Control and Prevention, and from the Children’s Hospital of Philadelphia. ML reports receiving support from the National Heart, Lung and Blood Institute of the National Institutes of Health (K24HL143283). RGG has received support from industry for research services (https://dcri.org/about-us/conflict-of-interest/).
Author information
Authors and Affiliations
Contributions
Concept and design: SAC, ZW, DKB, ML, SM, RGG and KMP. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: SAC. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: ZW and DKB. Administrative, technical, or material support: DKB and RHC. Study supervision: DKB, ML, RGG and KMP.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Coggins, S.A., Willis, Z., Benjamin, D.K. et al. Early antibiotic exposure in very-low birth weight infants and infection risk at 3–7 days after birth. J Perinatol 43, 1158–1165 (2023). https://doi.org/10.1038/s41372-023-01737-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01737-x