Abstract
Background:
Prolonged use of parenteral nutrition (PN) in neonates can lead to parenteral nutrition-associated liver disease (PNALD), manifested by elevated direct bilirubin concentrations, and in some cases progressing to hepatic failure. When new potential means of preventing PNALD in the neonatal intensive care unit (NICU), such as Omegaven usage, are tested in clinical trials, the studies should enroll neonates at a very high risk of developing PNALD. However, it is not always clear, in the first days of life, which neonates are most likely to develop PNALD. Therefore, preparatory to devising studies of prophylaxis against PNALD, we conducted an evaluation of all NICU patients who received PN for ⩾14 day, assessing their likelihood of developing PNALD.
Methods:
We performed an historic cohort analysis of all neonates in the Intermountain Healthcare system, receiving PN for 14 days or more during their stay, with dates of birth between 1 January, 2002 and 30 June, 2006.
Results:
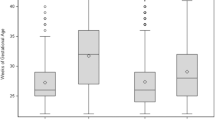
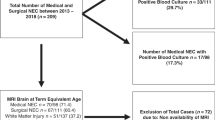
During the 4½-year period, 9861 neonates were cared for in the Intermountain Healthcare NICUs. Of these, 9547 (96.8%) survived for at least 28 days, and of these 6543 (68.5%) received PN. Twenty-one percent (1366 patients) of those receiving PN, received it for ⩾14 days. PNALD was ascertained in this group by a direct bilirubin ⩾2.0 mg/dl. Neonates receiving PN for 14–28 days had a 14% incidence of PNALD, those receiving PN for 29–56 days had a 43% incidence, those receiving PN for 57–100 days had a 72% incidence and those receiving PN for >100 days had a 85% incidence. Groups of patients identifiable on the first day of life as having the highest risk of developing PNALD were birth weight <500 g (odds ratio (OR), 30.7), birth weight 500–749 g (OR, 13.1), gastrochisis (OR, 20.3) and jejunal atresia (OR, 24.0). Among 357 patients who developed PNALD, the highest direct bilirubin concentrations correlated with the highest serum alkaline phosphatase and transaminase concentrations. Deaths after 28 days were much more common in those with the highest direct bilirubin and transaminase concentrations (P<0.0001).
Conclusions:
In the first days of life, certain NICU patients can be identified as being at very high risk for developing PNALD. These are patients <750 g birth weight, those with gastrochisis and those with jejunal atresia. We speculate that these groups would be reasonable subjects for including in a PNALD prophylaxis trial, testing new preventative strategies such as Omegaven usage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Abbreviations
- NICU:
-
neonatal intensive care unit
- PN:
-
parenteral nutrition
- PNALD:
-
parenteral nutrition-associated liver disease.
References
Thureen PJ, Hay Jr WW . Early aggressive nutrition in preterm infants. Semin Neonatol 2001; 6: 403–415.
Ziegler EE, Thureen PJ, Carlson SJ . Aggressive nutrition of the very low birthweight infant. Clin Perinatol 2002; 29: 225–244.
Teitlebaum DH . Parenteral nutrition-associated cholestasis. Curr Opin Pediatr 1997; 9: 270–275.
Kelly DA . Intestinal failure-associated liver disease: what do we know today? Gastroenterology 2006; 130 (2 Suppl 1): S70–S77.
Heubi JE, Wiechmann DA, Creutzinger V, Setchell KD, Squires Jr R, Couser R et al. Tauroursodeoxycholic acid (TUDCA) in the prevention of total parenteral nutrition-associated liver disease. J Pediatr 2002; 141: 237–242.
Teitelbaum DH, Tracy Jr TF, Aouthmany MM, Llanso A, Brown MB, Yu S et al. Use of cholecystokinin–octapeptide for the prevention of parenteral nutrition-associated cholestasis. Pediatrics 2005; 115: 1332–1340.
Tietelbaum DH, Han-Markey T, Drongowski RA, Coran AG, Bayar G, Geiger JD et al. Use of cholecystokinin to prevent the development of parenteral nutrition-associated cholestasis. JPEN J Parenter Enteral Nutr 1997; 21: 100–103.
Spencer AU, Yu S, Tracy TF, Aouthmany MM, Llanos A, Brown MB et al. Parenteral nutrition-associated cholestasis in neonates: multivariate analysis of the potential protective effect of taurine. JPEN J Parenter Enteral Nutr 2005; 29: 337–343.
Gleghorn EE, Merritt RJ, Subramanian N, Ramos A . Phenobarbital does not prevent total parenteral nutrition-associated cholestasis in noninfected neonates. JPEN J Parenter Enteral Nutr 1986; 10: 282–283.
Blaszyk K, Wild PJ, Olivera A, Kelly DG, Burgart LJ . Hepatic copper in patients receiving long-term total parenteral nutrition. J Clin Gastroenterol 2005; 39: 318–320.
Yip YY, Lim AK, Tan KL . A multivariate analysis of factors predictive of parenteral nutrition-related cholestasis (TPN cholestasis) in VLBW infants. J Singapore Paediatr Soc 1990; 32: 144–148.
Van Aerde JE, Duerksen DR, Gramlich L, Meddings JB, Chan G, Thomson AB et al. Intravenous fish oil emulsion attenuates total parenteral nutrition-induced cholestasis in newborn piglets. Pediatr Res 1999; 45: 202–208.
Alwayn IP, Gura K, Nose V, Zausche B, Javid P, Garza J et al. Omega-3 fatty acid supplementation prevents hepatic steatosis in a murine model of nonalcoholic fatty liver disease. Pediatr Res 2005; 57: 445–452.
Gura KM, Duggan CP, Collier SB, Jennings RW, Folkman J, Bistrian BR et al. Reversal of parenteral nutrition-associated liver disease in two infants with short bowel syndrome using parenteral fish oil: implications for future management. Pediatrics 2006; 118: e197–e201.
Gura KM, Parsons SK, Bechard LJ, Henderson T, Dorsey M et al. Use of a fish oil-based lipid emulsion to treat essential fatty acid deficiency in a soy allergic patient receiving parenteral nutrition. Clin Nutr 2005; 24: 839–847.
Marcus AD . A doctor's push for drug pits him against its maker. T Wall Street J 2006; 248: 1–15.
Mullick FG, Moran CA, Ishak KG . Total parenteral nutrition: a histopathologic analysis of the liver changes in 20 children. Mod Pathol 1994; 7: 190–194.
Zambrano E, El-Hennawy M, Ehrenkranz RA, Zelterman D, Reyes-Mugica M . Total parenteral nutrition induced liver pathology: an autopsy series of 24 newborn cases. Pediatr Dev Pathol 2004; 5: 425–432.
Kobuta A, Yonekura T, Oyanagi H, Kawahara H, Yagi M et al. Total parenteral nutrition-associated intrahepatic cholestasis in infants: 25 years' experience. J Pediatr Surg 2000; 35: 1049–1051.
Wales PW, de Sliva N, Kim JH, Lecce I, Sandhu A, Moore AM . Neonatal short bowel syndrome: a cohort study. J Pediatr Surg 2005; 40: 755–762.
Weinberger B, Watorek K, Strauss R, Witz G, Hiatt M, Hegyi T . Association of lipid peroxidation with hepatocellular injury in preterm infants. Crit Care 2002; 6: 521–525.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Christensen, R., Henry, E., Wiedmeier, S. et al. Identifying patients, on the first day of life, at high-risk of developing parenteral nutrition-associated liver disease. J Perinatol 27, 284–290 (2007). https://doi.org/10.1038/sj.jp.7211686
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211686
Keywords
This article is cited by
-
Cholestasis is associated with a higher rate of complications in both medical and surgical necrotizing enterocolitis
Journal of Perinatology (2024)
-
Targeted LC-MS/MS profiling of bile acids reveals primary/secondary bile acid ratio as a novel biomarker for necrotizing enterocolitis
Analytical and Bioanalytical Chemistry (2024)
-
Effects of mixed oil emulsion on short-term clinical outcomes in premature infants: A prospective, multicenter, randomized controlled trial
European Journal of Clinical Nutrition (2023)
-
Fish oil-containing lipid emulsions prevention on parenteral nutrition-associated cholestasis in very low birth weight infants: a meta-analysis
World Journal of Pediatrics (2022)
-
Partially hydrolyzed guar gum alleviates hepatic steatosis and alters specific gut microbiota in a murine liver injury model
Pediatric Surgery International (2022)