Abstract
OBJECTIVE:The use of continuous positive airway pressure (CPAP) in the treatment of a variety of neonatal respiratory conditions is associated with improvement in arterial oxygen saturation, decreased long-term morbidity, and an overall improvement in infant survival. We reasoned that CPAP might change diaphragm length by increasing end-expiratory lung volume (EEV), but the extent to which this occurs has not been assessed. This study was designed to evaluate (1) the extent to which CPAP shortens the diaphragm and (2) the relationship of diaphragm thickness and excursion with arterial oxygen saturation in spontaneously breathing preterm infants.
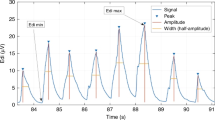
STUDY DESIGN:Ultrasonographically (7.5 MHz transducer), diaphragm thickness and diaphragm excursion were measured in 12 stable preterm infants [birth weight 1120±225 g (mean±SD); study weight 1187±400 g; gestational age 29±1 week; postnatal age 10±8 days, six males and six females] at three levels of CPAP [1–3, 4–6, and 7–9 cm H2O (low, medium, and high, respectively)]. Heart rate, respiratory rate, and arterial oxygen saturation were simultaneously recorded.
RESULTS:We found that diaphragm thickness and arterial oxygen saturation increased, and diaphragm excursion decreased significantly at higher levels of CPAP (p<0.05). The shortening of the diaphragm at the high levels of CPAP, calculated from the increase in diaphragm thickness, was 36% at EEV and 31% at end-inspiratory volume.
CONCLUSION:We conclude that the improvement in arterial oxygen saturation with CPAP occurred despite the presence of a shorter and a less mobile diaphragm, and that other physiological and mechanical alterations accompanying the application of CPAP offset its negative effects on diaphragm function. We speculate that with excessive CPAP, however, diaphragm dysfunction along with the previously described adverse hemodynamic effects may outweigh its benefits on oxygenation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Gregory G, Kitterman J, Phibbs R, Tooley W, Hamilton W Treatment of idiopathic respiratory distress syndrome with continuous positive airway pressure N Engl J Med 1971 284 1333–40
Avery ME, Tooley WH, Keller JB, et al Is chronic lung disease in low-birth-weight infants preventable? A survey of eight centers Pediatrics 1987 79 26–30
Bancalari E, Sinclair JC Mechanical ventilation In: Sinclair JC, Bracken MB, editors Effective Care of the Newborn Infant New York: Oxford University Press 1992 p. 200–20
LundstrØm KE, Griesen G Early treatment with nasal CPAP Acta Pediatr 1993 82 856–7
Hansen O, Hady-Abdel H, Petersen S, Greisen G Nasal continuous positive airway pressure Prenatal Neonat Med 1996 1 80–91
Verder H, Robertson B, Greisen G, et al Surfactant therapy and nasal continuous positive airway pressure for newborns with respiratory distress syndrome N Engl J Med 1994 331 1051–5
Klausner JF, Lee AY, Hutchison AA Decreased imposed work with a nasal continuous positive airway pressure device Pediatr Pulmonol 1996 22 188–94
Gergory GA Continuous airway pressure In: Thibeault DW, Gregory GA, editors Neonatal Pulmonary Care 2nd ed East Norwalk: Appleton-Century-Crofts 1986 p. 349–66
Kattwinkel J, Fleming D, Cha C, et al A device for administration of continuous positive airway pressure by the nasal route Pediatrics 1973 52 131–4
Field D, Vyas H, Milner AD, Hopkin IE Continuous positive airway pressure via a single nasal catheter in preterm infants Early Hum Dev 1985 11 275–80
Moa G, Nilsson K Nasal continuous positive airway pressure: experience with a new technical approach Acta Paediatr 1993 82 210–11
Miller MJ, DiFiore JM, Strohl KP, Martin RJ Effects of nasal CPAP on supraglottic and total pulmonary resistance in preterm infants J Appl Physiol 1990 68 141–6
Kattwinkel J, Nearman HS, Fanaroff A, Katona PG, Klaus MH Apnea of prematurity: comparative therapeutic effects of cutaneous stimulation and nasal CPAP J Pediatr 1975 86 588–92
Miller MJ, Carlo WA, Martin RJ Continuous positive airway pressure selectively reduces obstructive apnea in preterm infants J Pediatr 1985 106 91–4
Cotton R Pathophysiology of hyaline membrane disease (excluding surfactant) In: Polin R, Fox W, editors Fetal and Neonatal Physiology Philadelphia: WB Saunders 1998 p. 1165–74
Cohn DB, Benditt JO, Eveloff SE, McCool FD Diaphragm thickening during inspiration J Appl Physiol 1997 83 (1) 291–6
Rehan VK, Nakashima JM, Gutman A, Rubin LP, McCool FD Effects of the supine and prone position of diaphragm thickness in healthy infants Arch Dis Child 2000 83 234–8
Gabriel M, Albani M, Schulte FJ Apneic spells and sleep states in preterm infants Pediatrics 1976 57 142–7
Yu VYH, Rolfe P Effect of continuous positive airway pressure breathing on cardiorespiratory function in infants with respiratory distress syndrome Acta Pediatr Scand 1977 66 59–64
Wung J-T Respiratory management for low-birth-weight infants Crit Care Med 1993 21 S364–5
Laing IA, Teele RL, Stark AR Diaphragmatic movement in newborn infants JPediatr 1988 112 638–43
Rehan V, Laipraset J, Wallach M, Rubin L, McCool, FD Diaphragm dimensions in the healthy preterm infant Pediatrics 2001 (in press)
Rehan V, McCool FD Diaphragm dimensions in the healthy term infant [Abstract] Pediatr Res 1999 45 A1868
Mortola JP Dynamics of breathing in newborn mammals Physiol Rev 1987 67 187–243
Hagan R, Bryan AC, Bryan MH, Gulston G Neonatal chest wall afferents and regulation of respiration J Appl Physiol 1977 42 362–7
Locke R, Greenspan JS, Shaffer TH, Rubenstein SD, Wolfson MR Effect of nasal CPAP on thoraco-abdominal motion in neonates with respiratory insufficiency Pediatr Pulmonol 1991 11 259–64
Martin RJ, Nearman HS, Katona PG, Klaus MH The effect of a low continuous positive airway pressure on the reflex control of respiration in preterm infants J Pediatr 1977 90 976–81
Heldt GP, McIlroy MB Distortion of chest wall and work of diaphragm in preterm infants J Appl Physiol 1987 62 164–9
Boriek AM, Wilson TA, Rodarte JR Displacements and strains in the costal diaphragm of the dog Chest 1994 76 223–9
Margulies SS, Farkas GA, Rodarte JR Effects of body position and lung volume on in situ operating length of canine diaphragm J Appl Physiol 1990 69 1702–8
Hubmayr RD, Litchy WJ, Gay PC, Nelson SB Transdiaphragmatic twitch pressure: effects of lung volume and chest wall shape Am Rev Respir Dis 1988 139 647–52
McCool FD, Tzelepis GE, Leith DE, Hoppin FG Jr Oxygen cost of breathing during fatiguing inspiratory resistive loads J Appl Physiol 1989 66 2045–55
Author information
Authors and Affiliations
APPENDIX
APPENDIX
Calculation of diaphragm length (ldi) from diaphragm thickness (tdi):

where m, t, p, and l represent diaphragm mass, thickness, perimeter, and length, respectively. Assuming m and p are constant:

Therefore, change in diaphragm length from low and high CPAP can be obtained as follows:

Rights and permissions
About this article
Cite this article
Rehan, V., Laiprasert, J., Nakashima, J. et al. Effects of Continuous Positive Airway Pressure on Diaphragm Dimensions in Preterm Infants. J Perinatol 21, 521–524 (2001). https://doi.org/10.1038/sj.jp.7210587
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7210587
This article is cited by
-
Ultrasound evaluation of diaphragm kinetics after minimally invasive surfactant administration
Journal of Ultrasound (2023)
-
The increase in diaphragm thickness in preterm infants is related to birth weight: a pilot study
European Journal of Pediatrics (2023)
-
How to improve CPAP failure prediction in preterm infants with RDS: a pilot study
European Journal of Pediatrics (2021)
-
Sonographic evaluation of diaphragmatic thickness and excursion as a predictor for successful extubation in mechanically ventilated preterm infants
European Journal of Pediatrics (2021)