Abstract
OBJECTIVES: The bleeding time is a measurement of platelet and capillary interaction following a small standardized cutaneous incision. In adults, anemia causes a prolongation of the bleeding time, and we hypothesized that the same would be true in very low birth weight (VLBW) infants during their first week of life.
STUDY DESIGN: Template bleeding times, using the Surgicutt Newborn device, were performed on 20 VLBW weight infants ≤7 days old, before, and again following a clinically ordered erythrocyte transfusion.
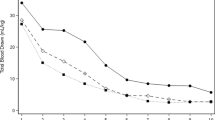
RESULTS: Neonates who had pretransfusion hematocrits ≤0.28 l/l had longer bleeding times, which fell 164±25 seconds (mean±SD; p<0.0001) following transfusion. Patients with pretransfusion hematocrits >0.28 l/l had no significant reduction in bleeding time following transfusion.
CONCLUSIONS: In VLBW infants, during their first week of life (the time when their risk of intraventricular hemorrhage is greatest), a low hematocrit is associated with a significant prolongation in the bleeding time.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Harker LA, Slichter SJ The bleeding time as a screening test for evaluation of platelet function N Eng J Med 1972 287 155–8
Khuri SF, Wolfe JA, Josa M, et al Hematologic changes during and after cardiopulmonary bypass and their relationship to the bleeding time and nonsurgical blood loss J Thorac Cardiovasc Surg 1992 104 94–107
Fernandez F, Goudable C, Sie P, et al Low haematocrit and prolonged bleeding time in uraemic patients: effect of red cell transfusions Br J Haematol 1985 59 139–48
Vigano G, Benigni A, Mendogni D, et al Recombinant human erythropoietin to correct uremic bleeding Am J Kidney Dis 1991 18 44–9
Cadroy Y, Hanson SR Effects of red blood cell concentration on hemostasis and thrombus formation in a primate model Blood 1990 75 2185–93
Crowley JP, Metzger JB, Valeri CR The volume of blood shed during the bleeding time correlates with the peripheral venous hematocrit Am J Clin Pathol 1997 108 579–84
Anand A, Feffer SE Hematocrit and bleeding time: an update South Med J 1994 87 299–301
Shulman I The anemia of prematurity J Pediatr 1959 54 663–72
Oski FA, Naiman JL Anemia in the neonatal period In: Oski FA, Naiman JL, editors. Hematologic Problems in the Newborn. Philadelphia: W.B. Saunders; 1982 p. 56–86
Strauss RG Blood banking and transfusion issues in perinatal medicine In: Christensen RD, editor. Hematologic Problems of the Neonate Philadelphia: W.B. Saunders 1999 p. 405–25
Andrew M, Paes B, Bowker J, Vegh P Evaluation of an automated bleeding time device in the newborn Am J Hematol 1990 35 275–7
Ment LR, Duncan CC, Ehrenkranz RA Intraventricular hemorrhage of the preterm neonate Semin Perinatol 1987 11 132–41
Duke WW The relation of blood platelets to hemorrhagic diseases JAMA 1910 60 1185–92
George TN, Johnson KJ, Bates JN, Segar JL The effect of inhaled nitric oxide therapy on bleeding time and platelet aggregation in neonates J Pediatr 1998 132 731–4
Andrew M, Castle V, Mitchell L, Paes B Modified bleeding time in the infant Am J Hematol 1989 30 190–1
Corazza MS, Davis RF, Merritt TA, Bejar R, Cventic W Prolonged bleeding time in preterm infants receiving indomethacin for patent ductus arteriosus J Pediatr 1984 105 292–6
Moia M, Mannucci PM, Vizzotto L, et al Improvement in the haemostatic defect of uraemia after treatment with recombinant human erythropoietin Lancet 1987 2 1226–9
Acknowledgements
We thank Pamela Connolly, RN, Ann Cothran, RN, and Jessica Wong, of the Clinical Research Center for their assistance in these studies.
Author information
Authors and Affiliations
Additional information
This study was supported by grants HL44951, HL61798, and RR00083 from the National Institutes of Health, by a grant from the Children's Miracle Network Telethon, and by a fellowship training grant from the American Heart Association.
Rights and permissions
About this article
Cite this article
Sola, M., del Vecchio, A., Edwards, T. et al. The Relationship Between Hematocrit and Bleeding Time in Very Low Birth Weight Infants During the First Week of Life. J Perinatol 21, 368–371 (2001). https://doi.org/10.1038/sj.jp.7210546
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7210546
This article is cited by
-
Ibuprofen lysine administration to neonates with a patent ductus arteriosus: effect on platelet plug formation assessed by in vivo and in vitro measurements
Journal of Perinatology (2009)
-
Template bleeding times of 240 neonates born at 24 to 41 weeks gestation
Journal of Perinatology (2008)