Abstract
Purpose
Despite the importance of a healthy endothelial layer in anterior segment surgery, the possible influence of corneal parameters on endothelial cell density (ECD) has largely been ignored in the young adult eye. This study investigated the possible associations between corneal tomographic parameters and ECD values in young adults.
Methods
Subjects aged 21–30 years, with normal corneas were recruited. Mean ECD, mean cell area (MCA), coefficient of variation for cell area (COVA), and proportion of hexagonal cells were derived by in vivoconfocal microscopy. The Orbscan II system was used to measure corneal parameters including: thickness, horizontal corneal diameter, corneal curvature, anterior and posterior elevation, and eccentricity.
Results
Sixty-two subjects (42 female, 20 male) were included (mean age 25±3 years). Overall mean ECD was 3169±309 cells/mm2 with no differences between genders. Mean percentage of hexagonality was 53±5%, male subjects (55%) had a higher percentage of hexagonal cells than female subjects (51%) (P=0.02). Central corneal thickness (CCT) was 529±43 μm. Central ECD was significantly correlated with CCT (Pearson's r=0.26, P=0.04). However, horizontal corneal diameter (r=0.19, P=0.14), anterior corneal curvature (r=−0.07, P=0.6), and posterior corneal curvature (r=−0.07, P=0.6) were not correlated with ECD or percentage of hexagonality. There was no statistically significant association between anterior chamber depth (3.6±0.3 mm) and ECD (r=0.15, P=0.3).
Conclusion
Corneal thickness is related to ECD in normal young adult eye, with lower ECD values identified in thinner corneas; however, corneal diameter and corneal curvature do not have a significant correlation with ECD.
Similar content being viewed by others
Introduction
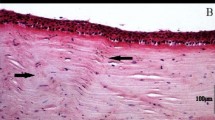
The corneal endothelium consists of a single layer of cuboidal and hexagonal cells, which line the posterior corneal surface.1, 2 The cornea is supplied with a relatively fixed population of endothelial cells (3500–4000 cells/mm2) at birth1 and although mitosis can occur in young endothelial cells, it is infrequent in the adult, thus injured cells are not replaced. It is well established that there is a gradual decrease in endothelial cell density (ECD) and a corresponding increase in polymegathism and pleomorphism with advancing age.1, 3, 4, 5, 6, 7, 8, 9 Clinically, the assessment of ECD and morphology can provide valuable information in relation to the functional reserve of the corneal endothelium.
Surprisingly, there have been few reports in the literature of the possible impact or association of corneal parameters on ECD in the normal eye. Our research group10 has previously reported on the effects of corneal parameters on the assessment of ECD in the elderly eye, concluding that in an older population, thinner and/or steeper corneas and longer axial lengths were strongly correlated with lower central ECD values. No significant correlation between horizontal corneal diameter and ECD was identified in this population. In contrast, in a study involving children (age range 5–15 years), a significant independent correlation was identified between increasing horizontal corneal diameter and lower central ECD values.11 A significant correlation between thinner corneas and lower ECD values has also been reported in children.12 However, despite the growing interest in intraocular refractive surgery procedures in young adults, there have been no previous reports that have specifically assessed the relationship between corneal tomographic parameters on ECD in normal young adults.
The aim of this study was to investigate the possible impact of corneal thickness, anterior and posterior corneal curvature, and horizontal corneal diameter on the measurement of ECD values in healthy young adults in their third decade—age range 21–30 years.
Methods
Subjects
Following an explanation of the purpose of the study, and written informed consent, 62 normal, healthy subjects were recruited into the study group. Only the right eye of each subject was included in assessment and analysis. Subject inclusion/exclusion criteria were defined as: no current or past ocular disease/trauma, freedom from ocular symptoms, no history of contact lens wear, no systemic diseases that may affect the cornea, and no abnormality on slit lamp biomicroscopic or computerized topography assessment. The study observed the tenets of the declaration of Helsinki, and ethical approval for this study was obtained from the Auckland Ethics Committee.
Assessment
The Orbscan II combined Placido and slit-scanning corneal tomography system (Orbscan, Bausch and Lomb, Salt Lake City, UT, USA) was used to measure corneal thickness, anterior elevation, posterior elevation, corneal eccentricity, horizontal corneal diameter, and anterior chamber depth. Before measurement, the subject's head/eye was carefully aligned with the instrument and a head strap was placed around the back of the head. The subject was advised to keep both eyes open and fixate on the internal target. By viewing the real-time image of the eye on the monitor, the examiner aligned the two fixation markers reflected by the instrument on the corneal surface before performing the scan. One Orbscan scan was acquired and saved per cornea and the central corneal pachymetry (thickness), horizontal corneal diameter, anterior corneal curvature (equivalent to the spherical radius of curvature using the least square method of determining the best fit sphere), and the eccentricity of the anterior and posterior surfaces was recorded.
For central corneal pachymetry, the pachymetry map option was selected and the data from the central measuring ring with a 1-mm sample zone diameter was noted. All pachymetry values were quoted using the standard acoustic correction factor (0.92).13
In vivo confocal microscopy of the cornea was performed using slit-scanning technology (Confoscan 2, Fortune Technologies America, Greensboro, NC, USA). The subject was asked to fixate on a target and the examination was performed with a × 40 non-applanating, immersion lens that covers an area of approximately 0.1 mm2. A drop of Viscotears (Carbomer 940 2 mg/g, CIBA Vision, Castle Hill, NSW, Australia) on the objective lens served as an immersion and contact substance. For all examinations, a standard setting of four passes was used, with a scanning range of between 700 and 800 μm (throughout the z-axis). One examination was performed on the centre of each cornea and up to 300 images were obtained for each examination.
Based on the best visibility of endothelial cells, three representative frames from each scan were chosen for analysis. Three frames per subject were analysed to reduce the effect of within person variation of the measurements. All captured images were analysed using the NAVIS (Nidek Advanced Vision Information System) proprietary software (Figure 1). The chosen frame size or region of interest (ROI) was 0.035 mm2. Using manually adjusted automated cell counts, the values for ECD, mean cell area, coefficient of variation for area and length, and percentage of hexagonal cells within each of the three frames were recorded and the mean values for each cornea were calculated. NAVIS identifies polygonal representations of the cells by using proprietary image-processing routines and contains an internal calibration for magnification. For manual correction, the polygons were superimposed over the image of the endothelial cells, and the user was allowed to add, delete, and move the polygon's apices based on visual inspection.14
Statistical analysis
Statistical analysis was performed in consultation with a medical statistician from the Epidemiology Department of the University of Auckland. The SPSS v 12 for Windows (Statistical Product and Service Solutions, Inc., Chicago, IL, USA) software package programme was used. Descriptive statistics (mean, standard deviation, median, and range) were calculated for each set of data. Differences between data sample means were determined by Student's t-test and one-way analysis of variance. Pearson's correlation coefficients were calculated to analyse the relationship between the parameters. A probability level of 0.05 or less was considered statistically significant.
Results
Subjects
Sixty-two normal subjects, 42 female and 20 male, all in their third decade with mean age 25±2.7 years (range 21–30) who met the inclusion/exclusion criteria were recruited into the study group. Sixty-two right eyes of these 62 subjects were included in the analyses. All results are expressed as mean±standard deviation.
Endothelial cell density
A mean of 135±17 cells were counted per image (range 94–169 cells) and approximately 10% of cells required manual adjustment of their borders.
The mean ECD for all subjects was 3169±309 cells/mm2 (range 2450–3802 cells/mm2). There was no significant gender-related difference in ECD (mean ECD in female subjects 3159±313 cells/mm2, mean ECD in male subjects 3187±308 cells/mm2, P=0.75). The ECD characteristics overall and for each gender are presented in Table 1. The analysis of each cornea included between 94 and 169 clearly visible cells per frame (mean 134±16 cells).
Analysis of the percentage of hexagonality provides a measure of cellular pleomorphism. The mean percentage of hexagonality overall was 53±5% with the range 43–68%. Male subjects (55%) had a significantly higher proportion of hexagonal cells compared to female subjects (51%) (P=0.02).
A negative and statistically significant correlation was identified between the proportion of hexagonal cells and the coefficient of variation for cell area (COVA) (r=−0.7, P<0.01) and COVL (r=−0.9, P<0.01), indicating a strong association between loss of hexagonal cell shape and variation in cell size.
Intra-class correlation (ICC) is the proportion of the variance that comes from between subjects; therefore, the closer ICC is to 1, the greater is the similarity of measures within a subject. ICC for endothelial parameters were as follows: ECD=0.88, mean cell area=0.89, COVA=0.70, COVL=0.67, and the percentage of hexagonal cells=0.78. Intra-subject variation was therefore small compared to inter-subject variation.
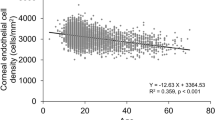
Corneal thickness
The mean central corneal thickness (CCT) was 529±43 μm (range 429–627 μm). There was no significant difference in CCT between male subjects (mean 530±50 μm) and female subjects (mean 529±30 μm) (P=0.9). When the mean central ECD values were compared with CCT values, a statistically significant correlation was identified (Pearson's r=0.26, P=0.04) (Figure 2). This indicates that lower ECD values were measured in thinner corneas. Although there was a clear trend for mean CCT to be negatively correlated with the proportion of hexagonal cells (indicating thinner corneas have a higher proportion of hexagonal cells), this trend did not reach statistical significance (r=−0.24, P=0.06).
Horizontal corneal diameter
The mean horizontal corneal diameter (HCD) for the entire study group was 11.7±0.4 mm and the range was 10.8–13.0 mm. There was no statistically significant difference in mean HCD between male subjects (mean 11.6±0.3 mm) and female subjects (mean 11.8±0.4 mm) (P=0.2). No statistically significant correlation between mean HCD and central ECD was identified (Pearson's r=0.19, P=0.14) (Figure 3). Analysis of the percentage of hexagonality and HCD revealed no significant relationship (r=−0.09, P=0.45).
Corneal curvature
The mean anterior corneal curvature (best-fit sphere) for the entire study group was 7.9±0.2 mm) and the range was 7.5–8.7 mm. The mean anterior eccentricity was 0.52, indicating that the mean anterior surface for all corneas assessed had the shape of a prolate ellipse (flattening peripherally). No statistically significant difference in mean anterior curvature between male subjects and female subjects was identified (P=0.6). There was no statistically significant correlation identified between mean anterior corneal curvature and central ECD (Pearson's r=−0.07, P=0.6).
The mean posterior corneal curvature was 6.5±0.2 mm and the range was 6.0–7.9 mm. The mean posterior eccentricity was 0.50, indicating the mean posterior surface had a prolate shape. No statistically significant difference in posterior corneal curvature between male subjects and female subjects was identified (P=0.6). There was no statistically significant correlation between mean posterior corneal curvature and central ECD (r=−0.07, P=0.6) (Figure 4).
Anterior chamber depth
The overall mean anterior chamber depth (ACD) was 3.6±0.3 mm and the range was 3.0–4.9 mm. No statistically significant difference in mean ACD between male subjects (mean 3.7±0.4 mm) and female subjects (mean 3.5±0.2 mm) was identified (P=0.05). There was no statistically significant correlation identified between mean ACD and central ECD in this study (r=0.15, P=0.3). A summary of the Pearson's correlation coefficients for all corneal parameters and endothelial values is presented in Table 2.
Discussion
The mean value for ECDin this current study (3169 cells/mm2) was in concordance with that previously reported in the literature for young adults (range 2680–3700 cells/mm2).15, 16, 17, 18, 19, 20 When compared with mean ECD values reported for children (3400–4300 cells/mm2) and for elderly eyes (2324–3175 cells/mm2), a clear trend of decreasing mean ECD with advancing age is observed.9, 10, 11, 15, 17, 21, 22, 23, 24, 25 Consistent with the majority of other published reports, there was no significant difference in mean ECD based on gender in this study.5, 9, 16, 17, 26, 27
With regards to the reliability and repeatability of the NAVIS endothelial analysis system, automated endothelial analysis often fails to correctly identify endothelial cell borders.14, 28 However, Kitzman et al14 have demonstrated that after manual correction of cell borders detected by the NAVIS automated software, the endothelial density, coefficient of variation of cell area, and percentage of hexagonal cells were not different from those determined by the Corners method. They therefore concluded that if the ConfoScan and its proprietary programme are used to determine cell density, investigators must manually correct cell boundaries on the images. Doughty et al15 reported that at least 75 cells should be counted per image for an acceptable level of inter-subject variance. Isager et al29 have reported that the magnification of the specular microscope decreases slightly with decreasing CCT. In the current study, the potential effect of magnification on ECD was accounted for by the NAVIS software, which contains an internal calibration for magnification.14
CCT measurement in this study (529 μm) was slightly less than that reported by Sanchis-Gimeno et al30 (554±16 μm), who studied the corneal thickness of 1000 young (range 20–30 years) emmetropic subjects using a similar Orbscan II slit-scanning corneal topography system. Comparison of CCT with other published reports is limited due to differences in measurement technique. Although the accuracy, precision, and repeatability of the Orbscan system has been accepted for use in research, it is recognized that it overestimates CCT compared to the more commonly used technique of ultrasound pachymetry.10, 31, 32 The current study has taken this into account by applying the standard acoustic correction factor.13 The repeatability of Orbscan pachymetry has been demonstrated to be approximately 2 μm33 to 5 μm.34
Similar to the observations of previous reports, we identified no significant difference in CCT based on gender in this study.35, 36, 37 The relationship between CCT and age has been extensively studied—although the majority of authors report a gradual decrease in CCT with advancing age after infancy,38, 39, 40, 41, 42 in contrast, others have reported no change or an increase in CCT with advancing age.36, 43
The relationship between significant endothelial dysfunction and increased corneal thickness is well established,3, 44, 45, 46 and recognized causes of increased corneal thickness include anterior segment disease and previous intraocular surgery.23, 42, 47, 48 However, the relationship between corneal thickness and ECD in the normal eye throughout life has yet to be fully established, with few reports in the literature investigating a possible relationship.
Studies investigating the influence of corneal thickness on ECD in the elderly eye have reported conflicting results. Muller et al10 in a study of pre-operative cataract surgery patients (mean age 75±11 years) identified a significant correlation between central ECD and central, superior, and temporal corneal thickness. Counter-intuitively, the authors demonstrated that in an older population, lower ECD values were associated with thinner corneas. In contrast, Ventura et al23 failed to identify a correlation between corneal thickness and ECD either pre-operatively or post-operatively in a study of elderly patients (mean age 71±15 years) undergoing cataract surgery. In the sole study, investigating the relationship between corneal thickness and ECD in children, Muller et al12 reported a significant correlation between thinner corneas and lower central ECD values in children with a mean age of 10±3 years. Interestingly, the results of the current study suggest that a similar relationship between central ECD and CCT, as highlighted in children and older adults by Muller et al,10, 12 may also exist in normal, healthy, young adult corneas.
Chang et al16 studied the corneas of young myopic adults (mean age 22±4 years). They identified that longer axial length was associated with flatter corneal curvature, decreased corneal thickness, and decreased ECD. However, they identified no direct correlation between corneal thickness and corneal curvature with ECD. To the authors' knowledge, currently there are no other published reports investigating the relationship between corneal thickness and ECD in young adults.
The mean HCD in the current study was identical to that reported by Rüfer et al49 in their study of 390 normal subjects using the Orbscan II scanning topography system (11.7±0.4 mm). Similarly, no significant difference based on gender was identified in either study.49 Several studies have investigated the change in corneal diameter with age. The majority of investigators have reported that corneal diameter reaches adult size by the end of the third year of life, with no significant age-related increase in corneal diameter thereafter.11, 50, 51, 52 However, a few investigators have suggested that corneal diameter may continue to change into late childhood.53, 54 This possibility is important because previous reports have identified that corneal diameter has an important effect on ECD in children, with a significant independent negative correlation between HCD and central ECD.11, 55, 56 The enlarged posterior corneal surface associated with an increased corneal diameter may require spreading of the fixed population of endothelial cells to cover the greater surface area, therefore resulting in a corresponding decrease in ECD. An increase in corneal diameter during infancy or early childhood may, therefore, be a factor in the recognized decrease in ECD that occurs during this time. However, the effect of HCD on central ECD in the elderly eye was studied by Muller et al,11 with no significant correlation identified. Similarly, in the current study, no significant relationship between HCD and central ECD was identified for normal young adults. This suggests that the effect of corneal diameter on the measurement of ECD in the normal eye may be limited to infants and children only.
The effect of corneal curvature on the measurement of ECD is yet to be fully established. A significant correlation between steeper corneas and lower ECD values has previously been recognized in the elderly eye,10 but the authors cautioned that there may be an artifactual element to this result, as the true optical effects of increased corneal curvature on the measurement of endothelial cell area by specular or in vivo confocal microscopy has yet to be elucidated. In this current study, no significant correlation between either anterior or posterior corneal curvature and ECD was identified. This is in concordance with the findings of Chang et al14 who identified no significant relationship between corneal curvature and ECD in myopic young adults. No studies appear to have specifically reported on the influence of corneal curvature on the measurement of ECD in infants or children.
Interestingly, Moezzi et al57 demonstrated that contact lens-induced corneal swelling flattens the posterior surface of the cornea. This raises the question of how ECD is affected by acutely induced changes in corneal curvature. Theoretically, any change in ECD would be expected to be minimal because the area of corneal endothelium imaged by the in vivo confocal microscope (0.087 mm2) is small relative to the diameter and curvature of the cornea.
In addition to the measurement of ECD, the percentage of hexagonality (percentage of six-sided cells) can also be used as an indicator of the health of the corneal endothelium. The mean percentage of hexagonality in this current study (53±5%) was less than that identified in two recently published reports that analysed mean percentage of hexagonality for the same age range as this study (both 61±7%).17, 58 Percentage of hexagonality of the corneal endothelium has been reported to gradually decrease with advancing age.4, 8, 17, 58 There was no correlation between percentage of hexagonality and ECD in this study. However, a significant correlation was identified between decreasing percentage of hexagonality and increased variation in cell area. A correlation between increasing percentage of hexagonality and decreasing corneal thickness was identified in this study, but the correlation marginally failed to reach statistical significance (P=0.057). Percentage of hexagonality was not related to the other corneal parameters assessed or to ACD.
The current study suggests that corneal thickness may be related to the measurement of ECD in the normal young adults, with lower ECD values associated with thinner corneas. The results of this study are therefore in concordance with earlier studies involving children and the elderly, which have demonstrated a significant correlation between corneal thickness and ECD. Corneal thickness decreases gradually with age and this may contribute to the apparent decline in ECD recognized with advancing age in the normal eye. The effect of corneal diameter on ECD appears to be limited to children, with no correlation between these parameters identified in the current study. This was in concordance with a previous study involving elderly eyes. The current study suggests that, at least for young adults, corneal curvature and ACD do not have an effect on the measurement of ECD.
By establishing the relationship between corneal parameters and ECD in healthy young adults, this study provides useful baseline data for future studies of the impact of diseases known to affect the cornea (eg diabetes mellitus), intraocular surgery (an increasingly popular option for refractive correction in this age group), and corneal refractive surgery. In the latter case, it is particularly important to take into account the effects of altered corneal curvature on endothelial image magnification and the questionable accuracy of Orbscan CCT measurements post-operatively.
The reasons behind the relationships reported here also merit further investigation in the form of structure–function correlation. For example, Doughty et al59 demonstrated that dynamic changes in CCT in young contact lens-wearing subjects are significantly correlated with apparent changes in ECD.
References
Shaw E, Rao G, Arthur E . The functional reserve of the corneal endothelium. Trans Am Acad Ophthalmol Otolaryngol 1978; 85: 640.
Kuwabara T . Current concepts in anatomy an histology of the cornea. Contact lens Intraoc Lens Med J 1978; 4: 101.
Waring III G, Bourne W, Edelhauser H, Kenyon KR . The corneal endothelium. Normal and pathologic structure and function. Ophthalmology 1982; 89: 531–590.
Bourne M, Kaufman H . Specular microscopy of human corneal endothelium in vivo. Am J Ophthalmol 1976; 81: 319–323.
Yee R, Matsuda M, Schultz R, Edelhauser HF . Changes in the normal corneal endothelial cellular pattern as a function of age. Curr Eye Res 1985; 4: 671–678.
Sturrock G, Sherrard E, Rice N . Specular microscopy of the corneal endothelium. Br J Ophthalmol 1978; 62: 809–814.
Cheng H, Jacobs P, McPherson K, Noble MJ . Precision of cell density and endothelial cell loss with age. Arch Ophthalmol 1985; 103: 1478–1481.
Laing R, Sandstrom M, Berrospi A, Leibowitz HM . Changes in the corneal endothelium as a function of age. Exp Eye Res 1976; 22: 587–594.
Laule A, Cable M, Hoffman C, Hanna C . Endothelial cell population changes of human cornea during life. Arch Ophthalmol 1978; 96: 2031–2035.
Muller A, Craig J, Grupcheva C, McGhee C . The effects of corneal parameters on the assessment of endothelial cell density in the elderly eye. Br J Ophthalmol 2004; 88: 325–330.
Muller A, Doughty M . Assessment of corneal endothelial cell density in growing children and its relationship to horizontal corneal diameter. Optom Vis Sci 2002; 79: 762–770.
Muller A . Assessment of eye growth related changes in the corneal endothelium of children and young teenagers. Glasgow Caledonian University PhD Thesis, 2000.
Fakhry MA, Artola A, Belda JI, Ayala MJ, Alio JL . Comparison of corneal pachymetry using ultrasound and Orbscan II. J Cataract Refract Surg 2002; 28 (2): 248–252.
Kitzmann AS, Winter EJ, Nau CB, McLaren JW, Hodge DO, Bourne WM . Comparison of corneal endothelial cell images from a noncontact specular microscope and a scanning confocal microscope. Cornea 2005; 24 (8): 980–984.
Doughty M, Muller A, Zaman M . Assessment of the reliability of human corneal endothelial cell density estimates using a noncontact specular microscope. Cornea 2000; 19: 148–158.
Chang SW, Tsai IL, Hu FR, Lin LL, Shih YF . The cornea in young myopic eyes. Br J Ophthalmol 2001; 85: 916–920.
Rao S, Sen P, Fogla R, Gangadharan S, Padmanabhan P, Badrinath SS . Corneal endothelial cell density and morphology in normal Indian eyes. Cornea 2000; 19: 820–823.
Bigar F . Specular microscopy of the corneal endothelium: optical solutions and clinical results. Dev Ophthalmol 1982; 6: 1–94.
Wilson R, Roper-Hall M . Effect of age on the endothelial cell count in the normal eye. Br J Ophthalmol 1982; 66: 513–515.
Doughty M . Prevalence of ‘non hexagonal’ cells in the corneal endothelium of young Caucasian adults, and their inter-relationships. Ophthalmic Physiol Opt 1998; 18: 415–422.
Snellingen T, Rao G, Shrestha J, Huq F, Cheng H . Quantitative and morphological characteristics of the human corneal endothelium in relation to age, gender, and ethnicity in cataract populations of South Asia. Cornea 2001; 20: 55–58.
Johnston R, Hasany S, Rootman D . Endothelial cell analysis of corneas from donor eyes with an intraocular lens: a comparative study. Cornea 1997; 16: 531–533.
Ventura A, Walti R, Bohnke M . Corneal thickness and endothelial density before and after cataract surgery. Br J Ophthalmol 2001; 85: 18–20.
Azen SP, Smith RE, Burg KA, Reinig J . Variation in central and vertical corneal endothelial cell density in normal subjects. Acta Ophthalmol 1981; 59: 94–99.
Price N, Barbour D . Corneal endothelial cell density in twins. Br J Ophthalmol 1981; 65: 812–814.
Matsuda M, Yee R, Edelhauser H . Comparison of the corneal endothelium in an American and a Japanese population. Arch Ophthalmol 1985; 103: 68–70.
Inoue K, Kimura C, Amano S, Oshika T, Tsuru T . Corneal endothelial changes twenty years after penetrating keratoplasty. Jap J Ophthalmol 2002; 46: 189–192.
Klais CM, Buhren J, Kohnen T . Comparison of endothelial cell count using confocal and contact specular microscopy. Ophthalmologica 2003; 217 (2): 99–103.
Isager P, Hjortdal JO, Ehlers N . Magnification changes in specular microscopy after corneal refractive surgery. Acta Ophthalmol Scand 1999; 77 (4): 391–393.
Sanchis-Gimeno JA, Lleo-Perez A, Alonso L, Rahhal MS . Anatomic study of the corneal thickness of young emmetropic studies. Cornea 2004; 23: 669–673.
Marsich M, Bullimore M . The repeatability of corneal thickness measures. Cornea 2000; 19: 792–795.
Chakrabarti HS, Craig JP, Brahma A, Malik TY, McGhee CN . Comparison of corneal thickness measurements using ultrasound and Orbscan slit scanning topography in normal and post-LASIK eyes. J Cataract Refract Surg 2001; 27: 1823–1828.
Lattimore Jr MR, Kaupp S, Schallhorn S, Lewis IV R . Orbscan pachymetry: implications of a repeated measures and diurnal variation analysis. Ophthalmology 1999; 106 (5): 977–981.
Grupcheva CN, Riley AF, Craig JP, Malik TY, McGhee CN . Analyzing small-incision cataract surgery by Orbscan II fourth-dimensional pachymetry mapping. J Cataract Refract Surg 2002; 28 (12): 2153–2158.
Price F, Koller D, Price M . Central corneal pachymetry in patients undergoing laser in situ keratomileusis. Ophthalmology 1999; 106: 2216–2220.
Cosar C, Sener A . Orbscan corneal topography system in evaluating anterior structures of the human eye. Cornea 2003; 22: 118–121.
Bron AM, Creuzot-Garcher C, Goudeau-Boutillon S, d'Athis P . Falsely elevated IOP due to increased corneal thickness. Graefes Arch Clin Exp Ophthalmol 1999; 237: 220–224.
Korey M, Gieser D, Kass MA, Waltman SR, Gordon M, Becker B . Central endothelial cell density and central corneal thickness in ocular hypertension and primary open angle glaucoma. Am J Ophthalmol 1982; 94: 610–616.
Olsen T . Light scattering from human cornea. Invest Ophthal Vis Sci 1982; 23: 66–81.
Herse P, Yao W . Variation of corneal thickness with age in young New Zealanders. Acta Ophthalmol 1993; 71: 360–364.
Lam A, Douthwaite W . The corneal thickness profile in Hong Kong Chinese. Cornea 1998; 17: 384–388.
Olsen T . Corneal thickness and endothelial damage after intercapsular cataract extraction. Acta Ophthalmol 1980; 58: 424–433.
Rapuano C, Fishbaugh J, Strike D . Nine point corneal thickness measurements and keratometry readings in normal corneas using ultrasound pachymetry. Insight 1993; 18: 16–22.
Jalbert I, Stapleton F, Papas E, Sweeney DF, Coroneo M . In vivo confocal microscopy of the human cornea. Br J Ophthalmol 2003; 87: 225–236.
O'Neal M, Polse K . In vivo assessment of mechanism controlling corneal hydration. Invest Ophthalmol Vis Sci 1985; 26: 849–856.
Cheng H, Bates AK, Wood L, McPherson K . Positive correlation of corneal thickness and endothelial cell loss. Serial measurements after cataract surgery. Arch Ophthalmol 1988; 106: 920–922.
Burns R, Bourne W, Brubaker R . Endothelial function in patients with corneal guttata. Invest Ophthalmol Vis Sci 1981; 20: 77–85.
Erickson P, Doughty MJ, Comstock TL, Cullen AP . Endothelial cell density and contact lens induced corneal swelling. Cornea 1998; 17: 152–157.
Rufer F, Schroder A, Erb C . White to white corneal diameter: normal values in healthy humans obtained with Orbscan II Topography System. Cornea 2005; 24: 259–261.
Hymes C . The postnatal growth of the cornea and palpebral fissure and the projection of the eyeball in early life. J Comp Neurol 1929; 48: 415–440.
Sorsby A, Benjamin B, Sheridan M . Refraction and Its Components During the Growth of the Eye from the Age of Three. Her Majesty's Stationary Office: London, 1961.
Peter R . Uber die Korneagrosse und ihre Vererbung. von Graefes Arch Ophthalmol 1924; 115: 29–48.
Bao S . Measurement of horizontal corneal diameter in 717 preschool children. Chung Hua Yen Ko Tsa Chih 1981; 17: 286–288.
Bruckner R, Batschelet E, Hugenschmidt F . The basal longitudinal study on aging: ophthalmo–gerontological research results. Doc Ophthalmol 1986; 64: 235–310.
Muller A, Doughty M, Wright L . Reassessment of the corneal endothelial cell organisation in children. Br J Ophthalmology 2000; 84: 692–696.
Muller A, Doughty M, Watson L . A retrospective pilot study to assess the impact of strabismus surgery on the corneal endothelium in children. Ophthalmic Physiol Opt 2002; 22: 38–45.
Moezzi AM, Fonn D, Simpson TL, Sorbara L . Contact lens-induced corneal swelling and surface changes measured with the Orbscan II corneal topographer. Optom Vis Sci 2004; 81 (3): 189–193.
Padilla D, Sibayan S, Gonzales C . Corneal endothelial cell density and morphology in normal Filipino eyes. Cornea 2004; 23: 129–135.
Doughty MJ, Aakre BM, Ystenaes AE, Svarverud E . Short-term adaptation of the human corneal endothelium to continuous wear of silicone hydrogel (lotrafilcon A) contact lenses after daily hydrogel lens wear. Optom Vis Sci 2005; 82 (6): 473–480.
Acknowledgements
We would like to acknowledge Elizabeth Robinson from the Epidemiology Department of the University of Auckland for her help with statistical analysis in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patel, H., Patel, D. & McGhee, C. Identifying relationships between tomography-derived corneal thickness, curvature, and diameter and in vivo confocal microscopic assessment of the endothelium in healthy corneas of young adults. Eye 23, 270–278 (2009). https://doi.org/10.1038/sj.eye.6703091
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703091