Abstract
Purpose
To determine population-based normative CCT data for elderly white subjects, with and without diabetes, and to explore the relationship between CCT and IOP and HRT2 measurements in such subjects with normal visual fields.
Methods
All eligible subjects were consecutive in a population screened for eye disease. CCT was measured by ultrasound pachymetry, and the optic disc was morphometrically defined using Heidelberg retinal tomography (HRT2). Inclusion criteria were: (1) normal visual field on suprathreshold testing and (2) corrected logMAR acuity of at least 0.3 in both eyes. Subjects with significant corneal pathology, previous corneal surgery, or known history of glaucoma or treatment for raised intraocular pressure were excluded. One eye was randomly selected from each subject for analysis.
Results
In all, 983 eyes of 983 subjects were included with 690 HRT images deemed acceptable for the analysis. The mean age (414 men and 569 women) was 73.3 years (minimum 65 years). Mean (SD) CCT was 544.1 (36.5) μm, with a normally distributed range of 429–633 μm. There was no significant difference in CCT between men and women (mean CCT 546.1 and 542.7 μm, respectively, P=0.15, Student's t-test), though CCT was correlated weakly and negatively with age (Pearson's r=−0.063, P=0.047). Diabetic patients (n=103) had a greater mean CCT than non-diabetic patients (551.9 and 543.0 μm respectively, P=0.02). No significant correlation was found between any global optic disc parameter and CCT in the 690 eyes analysed.
Conclusion
Elderly white eyes with normal fields have CCTs that are normally distributed, with those from diabetic persons having greater CCTs. No clear evidence of a relationship between CCT and HRT2 optic disc parameters used in glaucoma diagnosis was found.
Similar content being viewed by others
Introduction
Thin central corneal thickness (CCT) has been shown to be a powerful risk factor for the progression of ocular hypertension (OHT) and preperimetric glaucomatous optic neuropathy to primary open-angle glaucoma (POAG).1, 2 Patients with a CCT of ⩽555 μm in the ocular hypertension treatment study (OHTS) had a three-fold increase in the risk of glaucoma development compared with those having CCT of ⩾588 μm.3 In addition, thinner CCT is associated with more severe glaucoma progression, both at first presentation to the ophthalmologist,4 and during follow-up.5 However, the mechanism by which CCT is related to glaucoma risk remains, as yet, unclear.
It is generally accepted that an indirect relationship between CCT and glaucoma risk operates via its relationship with intraocular pressure (IOP). CCT is positively related to IOP with thinner corneas requiring less force than expected to achieve applanation by Goldmann applanation tonometry. Thus, true IOP, and therefore glaucoma risk, may be underestimated in these eyes. This may explain the findings that mean CCT is thinner in patients with normal tension glaucoma compared with those having POAG,6, 7 and thicker in patients with OHT.8, 9 These findings are replicated among different racial groups.10
In addition, in a multivariate analysis of baseline factors predicting the conversion of OHT into POAG within OHTS, CCT was retained as a risk factor independent of its relationship with IOP.3 Speculative proposals on the mechanism of this IOP-independent interaction reflect the nature of the cornea as an extension of the sclera. They include an association with altered trabecular meshwork function and a relationship with optic nerve head morphometry, perhaps via the quality of lamina cribrosa support. One study found that at the time of referral of OHT and POAG patients, CCT correlated positively with optic nerve head rim area.11 Two other studies demonstrated the relationships between CCT and neuroretinal tissue measurements in OHT patients12 and normal subjects.13 However, none of these studies were population based and so are prone to unpredictable sources of bias.
This study presents data obtained from subjects screened by the Bridlington Eye Assessment Project (BEAP)14 effectively, a screening programme for ocular disease in elderly white subjects. The aim of the current study was to determine population-based normative CCT data for elderly white subjects both with and without diabetes, and to explore the relationship between CCT and IOP and HRT2 measurements in such subjects with normal visual fields.
Methods
Subjects: the Bridlington Eye Assessment Project
The methodology of BEAP has been previously described.14 Briefly, the project is a screening exercise for eye disease in patients over 65 years of age. Approximately 6500 such subjects registered with the general practitioners in the town of Bridlington, England were systematically invited to attend an extensive eye examination performed by one of four optometrists trained specifically for the project. Patients registered blind or partially sighted, bed-bound or suffering dementia, and those moving into or out of the area during the study were excluded.
A relevant standardized medical history was obtained (eg, diabetes, stroke, hypertension) together with the patient's drug and family history. Distance and reading spectacle requirements were recorded in addition to any history of amblyopia, ocular surgery, or any other ocular disease. Specifically, any history of glaucoma was noted.
Patients then underwent a comprehensive eye examination, logMAR visual acuity testing (Bailey Lovie #4 Chart, National Vision Research Institute of Australia) and automated suprathreshold visual field testing with the Henson Pro 5000 perimeter (Tinsley Instruments, Croydon, UK). A single stimulus, suprathreshold central 26-point test was employed. This was automatically extended to a 68-point test if a defect was detected. Intraocular pressure (IOP) was measured by a calibrated Goldmann tonometer and CCT measurement was performed by ultrasound pachymetry (Tomey SP-3000 Pachymeter, Tomey Corporation, Nagoya, Japan). The pachymeter probe operates at a frequency of 20 MHz with a resolution of 1 μm. Each scan comprises 10 individual measurements with the mean measurement being recorded in micrometres (μm). After instillation of tropicamide 1% into both eyes, systematic slit-lamp biomicroscopy was performed and Heidelberg retina tomograph II images (HRT2, Software Version 2.1, Heidelberg Engineering GmbH, Dossenheim, Germany) were obtained.
Bridlington Eye Assessment Project saw its first patient on 5 November 2002 and had seen 2434 patients (58% acceptance rate) when this study commenced. Patients were invited in ascending numerical order of postcode. An informed written consent was obtained from all participants and a Local Ethics Committee approved all methodology. All methods adhered to the tenets of the Declaration of Helsinki guidelines for research in human subjects.
Patient selection
Normal individuals were selected for this study from the BEAP database, with one eye chosen at random from each subject. Normality was defined with the following criteria applied to both eyes: (1) normal visual field determined by suprathreshold automated examination and (2) corrected logMAR acuity of at least 0.3 (Snellen equivalent 6/12). Exclusion criteria were: (1) significant corneal pathology that might influence corneal thickness, such as corneal ulcers or scars, endothelial guttata, or keratic precipitates (2) previous corneal surgery (3) known history of glaucoma or intraocular pressure-lowering-treatment and (4) incomplete data relating to the above criteria.
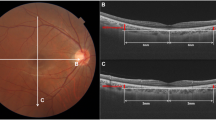
Confocal scanning laser ophthalmoscope assessment
Patients were imaged with HRT2, with the scanner's focus being adjusted according to the patient's refraction, and to obtain the best image. One mean topographic image was acquired per eye. Much of the acquisition process using HRT2 is automated. If the machine stated that astigmatism was significantly impairing the image then the image was obtained through the patients' spectacles. If the image acquired was subjectively unacceptable then the process was repeated to obtain an acceptable image, although this was not possible in a minority of patients. The optic disc contour line was drawn on all images by one investigator (MJH). The HRT2 software then calculated disc area (mm2), reference height (mm) and 12 further stereometric parameters, cup area (mm2), rim area (mm2), cup/disc area ratio, rim/disc area ratio, cup volume (mm3), rim volume (mm3), mean cup depth (mm), maximum cup depth (mm), height variation contour (mm), cup shape measure, mean retinal nerve fibre layer (RNFL) thickness (mm), and RNFL cross-sectional area (mm2). Each of these parameters was expressed for the global disc, and for six individual disc sectors (temporal, temporal superior, temporal inferior, nasal, nasal superior, and nasal inferior). Images with a mean pixel height SD greater than 50 μm were excluded from further analysis. Statistical analyses were conducted using SPSS for Windows version 12.0.2 (Statistical Package for Social Sciences, SPSS Inc., Chicago, IL, USA). Two-tailed tests were used in all statistical analyses. Statistical significance was set at P<0.05.
Results
Demographics
In all, 983 eyes of 983 consecutive subjects satisfying the entry criteria were included from the 2434 people examined. All subjects were white and of European extraction; 42% were men, and 52% of eyes were right sided. The mean (SD) age of the 983 subjects was 73.3 (5.2) years (range 65.3–94.2 years). The mean age of men and women was not significantly different (73.2 and 73.3 years, respectively, P=0.67, Mann–Whitney U-test). Of the 983 subjects, 103 (10.5%) had a history of diabetes, 453 (46%) had a history of hypertension, 66 (6.7%) reported previous cerebrovascular disease, and 131 (13%) reported a family history of glaucoma.
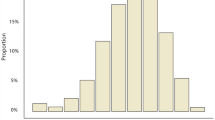
Central corneal thickness
Central corneal thickness was normally distributed in the 983 eyes (Figure 1). The mean (SD) CCT was 544.1 (36.5) μm (range 429–633 μm) and the mean CCT in right and left eyes was 544.0 and 544.3 μm, respectively (P=0.92, Student's t-test). There was no significant difference in CCT between men and women (mean CCT 546.1 and 542.7 μm, respectively, P=0.15, Student's t-test). CCT correlated negatively very weakly with age (Pearson's r=−0.063, P=0.047). Mean CCT was found to be significantly greater in those with diabetes mellitus (551.9 μm) compared with nondiabetics (543 μm; P=0.02, Student's t-test). There was no significant difference in mean CCT between those reporting systemic hypertension (542.3 μm) and normotensives (544.8 μm; P=0.29, Student's t-test), or between those with previous intraocular surgery (545.7 μm) and those without such a history (544.1 μm; P=0.76). There was no significant difference in CCT between those with and without a positive family history of glaucoma (mean CCT 543.3 and 543.7 μm, respectively, P=0.62, Student's t-test). No significant correlation was found between CCT and study number indicating no calibration drift with study duration.
Intraocular pressure
The mean (SD) IOP in the 983 eyes was 16.4. (3.0) mmHg, with a range of 8–32 mmHg. The mean IOP in men and women did not differ significantly (16.5 and 16.3 mmHg, respectively, P=0.19, Student's t-test). In addition, there was no difference in IOP between eyes, with a mean IOP of 16.3 mmHg in left eyes and 16.4 mmHg in right eyes. There was no significant difference in mean IOP between diabetic and non-diabetic patients (16.7 and 16.3 mmHg, respectively; P=0.22, Student's t-test). There was a small but significant positive correlation between CCT and measured IOP in our sample (Pearson's r=0.13, P<0.001; Figure 2). No significant correlation was found between IOP and study number indicating no calibration drift with study number.
Optic nerve head parameters
In total, 690 of the 983 eyes had acceptable HRT2 image quality for analysis. Subjects with acceptable images were on average younger than those with images of unacceptable quality (mean ages 72.6 and 75.3 years, respectively; P<0.001, Mann–Whitney U-test). Mean CCT tended to be greater in subjects with acceptable images, though of borderline statistical significance (mean CCT 544.8 and 537.3 μm, respectively; P=0.07, Student's t-test).
There was no significant correlation between any global optic nerve head parameter and CCT in this group of eyes (Table 1, Figure 3). The Spearman's rank correlation coefficients between CCT and HRT2 sectoral ONH parameters were all nonsignificant except for cup area in the temporal (rs=−0.07, P=0.05) and temporal-superior sectors (rs=−0.09, P=0.02).
Discussion
To our knowledge this is the first study to simultaneously report CCT data and objective ONH parameters (using HRT2) in an elderly white population. The elderly are an important group in the study of glaucoma since they have the greatest prevalence of the disease.15 The study group employed in this research represents a population of elderly subjects without visual field defect or a diagnosis of glaucoma. As the only entry criteria were based on visual field and visual acuity, we included subjects with IOPs outside the normal range and optic discs which might be determined as glaucomatous by some observers. Our sample of nearly 700 eyes from 700 persons analysing CCT against HRT should therefore include eyes that will be progressing towards glaucomatous field loss. The number of ONHs in the sample has been sufficient to demonstrate systematic differences in HRT2 parameters between elderly men and women in one of our previous publications,14 the former of which have twice the prevalence of the disease.15 Thus, the absence of any relationship between global HRT2 parameters and CCT in this study suggests that if a larger study found a relationship, it would likely be of little clinical significance (the finding of two statistically significant associations in the 72 sectoral analyses of CCT vs HRT2 parameters would be expected by chance in a study with large numbers such as ours and is also of no clinical significance).
Previous studies investigating the relationship between CCT and ONH have produced varying results. One study found no relationship between CCT and retinal nerve fibre layer thickness (measured by scanning laser polarimetry) in 44 eyes with normal visual fields and clinically normal optic discs.13 Additionally, investigations into the relationship between CCT and scleral characteristics found no correlation with post-mortem lamina cribrosa or scleral thickness in normal eyes,16 or with axial length in the clinic setting.17 Studies which have found a relationship between CCT and ONH parameters did so only in ocular hypertensive and glaucomatous eyes.11, 12 One of these studies found a significant relationship between CCT and ONH rim area at the time of referral of glaucoma patients but found no relationship between CCT and risk of progression during follow-up.11 In these samples, the substantial confounding effects of IOP, as measured by applanation, which may have a nonlinear relationship with CCT,18 and those of the glaucomatous process, may make isolation of the relationship between CCT and ONH difficult. Age is a further confounding factor since CCT decreases,10, 19, 20 and POAG prevalence increases, with advancing years. In addition, limitations of the CCT measurement protocol in the OHTS study3 may make the finding of a statistically independent relationship between CCT and the risk of POAG development unreliable.11 Our study adds weight to the evidence that, in the white elderly population with normal fields, lower CCT values are not associated with reduced neuro-retinal rim measurements on the HRT2, and therefore probably not an important risk factor for future glaucomatous visual field loss.
In our study with 983 eyes from 983 white persons of European extraction, CCT was normally distributed with a mean of 544.1 μm and a range of 429–633 μm, similar to the findings of the Rotterdam Study.21 Our study found that CCT was positively correlated with IOP in elderly white subjects without visual field defect. A similar relationship has been found in various populations,21, 22, 23, 24 although it was not present in the black participants of the Barbados Eye Study.25 IOP measured by Goldmann applanation tonometry should ideally be adjusted for CCT, although a simple nomogram is unlikely to be accurate in all cases due to the influence of other factors such as corneal rigidity. In addition to our study, other researchers have found a significant thinning of the central cornea with age.8, 10, 19, 20 Two studies which also only recruited older participants, failed to detect a significant relationship.21, 22, 23, 24 The changes in structural corneal biomechanics with subject age adds further complexity to the relationship between CCT and Goldmann IOP.26
The diabetic patients in our study had significantly greater CCTs than the non-diabetic patients, although only by a mean of 9 μm. Although the eyes of diabetics (all type 2) had higher IOPs (a mean of 0.4 mmHg higher) in our study, this did not reach statistical significance in contrast to the results of larger comparative studies that included types 1 and 2 diabetics.27, 28 Similar findings of an association between diabetes and thicker CCT have been found in the Barbados Eye Study,25 and in another study,29 whereas a Japanese study found no increase in CCT in type 2 diabetic patients.30
Potential sources of bias exist in our study. As BEAP did not utilise a randomised sampling procedure, we cannot be sure that the study population is representative of the whole population. However, using the Jarman Index (a measure of deprivation), those not attending did not differ from attendees during the project. The exclusion of 30% of subjects due to poor HRT2 image quality is unfortunately an inevitable consequence of a study such as this. This issue has been discussed previously,14 and represents the reduction in image quality with increasing age, and is due to a number of factors including lens clarity. However, there was no significant difference in CCT and age between those included and excluded on the grounds of HRT quality. A further potential limitation to the study is the fact that we did not measure intra- and inter-observer repeatability of CCT during BEAP. This was for logistical reasons in such a large screening exercise with much data to collect from each individual. Some studies have shown significant variability in CCT measured by ultrasound pachymetry on different occasions,31, 32, 33 although others have found a high degree of reproducibility.34, 35 Finally, we cannot be sure that those considered not to have diabetes would all be deemed negative by strict criteria as it was impractical to perform glucose tolerance tests on all subjects.
In conclusion, our study indicates that CCT is normally distributed in the white elderly population with normal visual fields, that diabetics have thicker corneas than nondiabetics within this population and that there is no significant association between CCT and optic nerve characteristics used in glaucoma diagnosis on HRT scanning. This suggests that the measurement of CCT in white elderly people with normal fields is of no value in predicting the ONH morphology as measured by the HRT2, and may be of no value in predicting future field loss from glaucoma in screening programmes.
References
Medeiros FA, Sample PA, Zangwill LM, Bowd C, Aihara M, Weinreb RN . Corneal thickness as a risk factor for visual field loss in patients with preperimetric glaucomatous optic neuropathy. Am J Ophthalmol 2003; 136 (5): 805–813.
Medeiros FA, Sample PA, Weinreb RN . Corneal thickness measurements and frequency doubling technology perimetry abnormalities in ocular hypertensive eyes. Ophthalmology 2003; 110 (10): 1903–1908.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA et al. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120 (6): 714–720; discussion 829–830.
Herndon LW, Weizer JS, Stinnett SS . Central corneal thickness as a risk factor for advanced glaucoma damage. Arch Ophthalmol 2004; 122 (1): 17–21.
Kim JW, Chen PP . Central corneal pachymetry and visual field progression in patients with open-angle glaucoma. Ophthalmology 2004; 111 (11): 2126–2132.
Ventura AC, Bohnke M, Mojon DS . Central corneal thickness measurements in patients with normal tension glaucoma, primary open angle glaucoma, pseudoexfoliation glaucoma, or ocular hypertension. Br J Ophthalmol 2001; 85 (7): 792–795.
Morad Y, Sharon E, Hefetz L, Nemet P . Corneal thickness and curvature in normal-tension glaucoma. Am J Ophthalmol 1998; 125 (2): 164–168.
Brandt JD, Beiser JA, Kass MA, Gordon MO . Central corneal thickness in the ocular hypertension treatment study (OHTS). Ophthalmology 2001; 108 (10): 1779–1788.
Wu LL, Suzuki Y, Ideta R, Araie M . Central corneal thickness of normal tension glaucoma patients in Japan. Jpn J Ophthalmol 2000; 44 (6): 643–647.
Aghaian E, Choe JE, Lin S, Stamper RL . Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African-Americans, and Japanese in a glaucoma clinic. Ophthalmology 2004; 111 (12): 2211–2219.
Jonas JB, Stroux A, Velten I, Juenemann A, Martus P, Budde WM . Central corneal thickness correlated with glaucoma damage and rate of progression. Invest Ophthalmol Vis Sci 2005; 46 (4): 1269–1274.
Henderson PA, Medeiros FA, Zangwill LM, Weinreb RN . Relationship between central corneal thickness and retinal nerve fiber layer thickness in ocular hypertensive patients. Ophthalmology 2005; 112 (2): 251–256.
Iester M, Mermoud A . Retinal nerve fiber layer and physiological central corneal thickness. J Glaucoma 2001; 10 (3): 158–162.
Vernon SA, Hawker MJ, Ainsworth G, Hillman JG, Macnab HK, Dua HS . Laser scanning tomography of the optic nerve head in a normal elderly population: the Bridlington Eye Assessment Project. Invest Ophthalmol Vis Sci 2005; 46 (8): 2823–2828.
Wolfs RC, Borger PH, Ramrattan RS, Klaver CC, Hulsman CA, Hofman A et al. Changing views on open-angle glaucoma: definitions and prevalences—the Rotterdam study. Invest Ophthalmol Vis Sci 2000; 41 (11): 3309–3321.
Jonas JB, Holbach L . Central corneal thickness and thickness of the lamina cribrosa in human eyes. Invest Ophthalmol Vis Sci 2005; 46 (4): 1275–1279.
Shimmyo M, Orloff PN . Corneal thickness and axial length. Am J Ophthalmol 2005; 139 (3): 553–554.
Kniestedt C, Lin S, Choe J, Bostrom A, Nee M, Stamper RL . Clinical comparison of contour and applanation tonometry and their relationship to pachymetry. Arch Ophthalmol 2005; 123 (11): 1532–1537.
Sanchis-Gimeno JA, Lleo-Perez A, Alonso L, Rahhal MS . Caucasian emmetropic aged subjects have reduced corneal thickness values: emmetropia, CCT and age. Int Ophthalmol 2004; 25 (4): 243–246.
Cho P, Lam C . Factors affecting the central corneal thickness of Hong Kong-Chinese. Curr Eye Res 1999; 18 (5): 368–374.
Wolfs RC, Klaver CC, Vingerling JR, Grobbee DE, Hofman A, de Jong PT . Distribution of central corneal thickness and its association with intraocular pressure: the Rotterdam study. Am J Ophthalmol 1997; 123 (6): 767–772.
Nomura H, Ando F, Niino N, Shimokata H, Miyake Y . The relationship between age and intraocular pressure in a Japanese population: the influence of central corneal thickness. Curr Eye Res 2002; 24 (2): 81–85.
Foster PJ, Baasanhu J, Alsbirk PH, Munkhbayar D, Uranchimeg D, Johnson GJ . Central corneal thickness and intraocular pressure in a Mongolian population. Ophthalmology 1998; 105 (6): 969–973.
Eysteinsson T, Jonasson F, Sasaki H, Arnarsson A, Sverrisson T, Sasaki K et al. Central corneal thickness, radius of the corneal curvature and intraocular pressure in normal subjects using non-contact techniques: Reykjavik eye study. Acta Ophthalmol Scand 2002; 80 (1): 11–15.
Nemesure B, Wu SY, Hennis A, Leske MC . Corneal thickness and intraocular pressure in the Barbados eye studies. Arch Ophthalmol 2003; 121 (2): 240–244.
Malik NS, Moss SJ, Ahmed N, Furth AJ, Wall RS, Meek KM . Ageing of the human corneal stroma: structural and biochemical changes. Biochim Biophys Acta 1992; 1138 (3): 222–228.
Dielemans I, de Jong PT, Stolk R, Vingerling JR, Grobbee DE, Hofman A . Primary open-angle glaucoma, intraocular pressure, and diabetes mellitus in the general elderly population. The Rotterdam study. Ophthalmology 1996; 103 (8): 1271–1275.
Mitchell P, Smith W, Chey T, Healey PR . Open-angle glaucoma and diabetes: the Blue Mountains eye study, Australia. Ophthalmology 1997; 104 (4): 712–718.
Larsson LI, Bourne WM, Pach JM, Brubaker RF . Structure and function of the corneal endothelium in diabetes mellitus type I and type II. Arch Ophthalmol 1996; 114 (1): 9–14.
Inoue K, Kato S, Inoue Y, Amano S, Oshika T . The corneal endothelium and thickness in type II diabetes mellitus. Jpn J Ophthalmol 2002; 46 (1): 65–69.
Shildkrot Y, Liebmann JM, Fabijanczyk B, Tello CA, Ritch R . Central corneal thickness measurement in clinical practice. J Glaucoma 2005; 14 (5): 331–336.
Harper CL, Boulton ME, Bennett D, Marcyniuk B, Jarvis-Evans JH, Tullo AB et al. Diurnal variations in human corneal thickness. Br J Ophthalmol 1996; 80 (12): 1068–1072.
Wickham L, Edmunds B, Murdoch IE . Central corneal thickness: will one measurement suffice? Ophthalmology 2005; 112 (2): 225–228.
Shah S, Spedding C, Bhojwani R, Kwartz J, Henson D, McLeod D . Assessment of the diurnal variation in central corneal thickness and intraocular pressure for patients with suspected glaucoma. Ophthalmology 2000; 107 (6): 1191–1193.
Miglior S, Albe E, Guareschi M, Mandelli G, Gomarasca S, Orzalesi N . Intraobserver and interobserver reproducibility in the evaluation of ultrasonic pachymetry measurements of central corneal thickness. Br J Ophthalmol 2004; 88 (2): 174–177.
Acknowledgements
We wish to thank Mrs S MacNab (Project Manager), Mr S Brown, Mrs J Button, Mr G Langton, and Mr M Kunz (Optometrists) for their work with the project. We thank Mr J Bapty, Mr N Connell, Mr P Jay, and Mrs G Poole for their work as the charity trustees of the Bridlington Eye Assessment Project. Financial support: The Bridlington Eye Assessment Project was funded by an unrestricted grant from Pfizer. We also thank the following organisations for financial support of the Project: Pharmacia, Yorkshire Wolds & Coast Primary Care Trust, the Lords Feoffees of Bridlington, Bridlington Hospital League of Friends, the Hull & East Riding Charitable Trust, the National Eye Research Centre (Yorkshire), the Rotary Club of Bridlington, the Alexander Pigott Wernher Memorial Trust, Bridlington Lions Club, the Inner Wheel Club of Bridlington, Soroptimist International of Bridlington, and the Patricia and Donald Shepherd Charitable Trust.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented as a free paper at the Royal College of Ophthalmologists Annual Congress 2006.
Competing interests: None.
Conflict of Interest: None of the authors have any financial interests to declare in relation to this manuscript.
Rights and permissions
About this article
Cite this article
Hawker, M., Edmunds, M., Vernon, S. et al. The relationship between central corneal thickness and the optic disc in an elderly population: the Bridlington Eye Assessment Project. Eye 23, 56–62 (2009). https://doi.org/10.1038/sj.eye.6703001
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703001
Keywords
This article is cited by
-
The thick and thin of the central corneal thickness in glaucoma
Eye (2018)
-
Relationship of corneal hysteresis and optic nerve parameters in healthy myopic subjects
Scientific Reports (2017)