Abstract
Purpose
To report the vision outcome following intravitreal triamcinolone acetonide (IVTA) as adjunctive therapy in four eyes of two patients with paraneoplastic autoimmune optic neuritis and vitreitis related to CRMP (Collapsin-Response-Mediator Protein)-5-IgG.
Design
Retrospective case series.
Methods
Chart review of four eyes.
Results
Preoperative visions were: patient 1, 20/50 OD, 20/25 OS; patient 2, counting fingers (CF) at two feet OD, and CF at three feet OS. At last follow-up, the postoperative visions were 20/40, 20/50 and 20/200, 20/60, respectively. All signs of optic disc swelling and vitreitis had abated.
Conclusions
Use of IVTAin paraneoplastic autoimmune optic neuritis and vitreitis related to CRMP-5-IgG was followed by a marked decrease in inflammation and stabilization or improvement of vision. These observations support this form of adjunctive therapy in patients whose intraocular pathology is attributed to paraneoplastic autoimmunity.
Similar content being viewed by others
Introduction
Autoimmune optic neuritis and vitreitis associated with CRMP-5–IgG1 is the most commonly encountered paraneoplastic vision loss disorder related to small-cell lung carcinoma (SCLC) (VA Lennon, personal observation). The CRMP-5 protein is expressed in the cytoplasm of this neoplasm as well as in neurons, retina, and optic nerve.2 The immune response initiated by tumoral CRMP-5 and marked by CRMP-5–IgG can result in progressive deterioration of vision accompanied by infiltration of the optic nerve and vitreous by CD8+ and CD4+ T lymphocytes, respectively.2 The efficacy of systemic immunomodulatory therapy in these cases is uncertain. We present four eyes in two patients with bilateral optic neuritis and vitreitis associated with CRMP-5–IgG whose vision improved after intravitreal triamcinolone acetonide therapy (IVTA).
Case 1
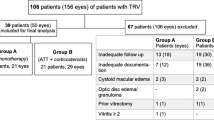
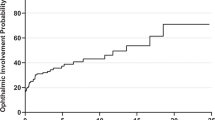
A 75-year-old man had a one-month history of photopsias with decreasing and fluctuating vision. He was known to have extensive SCLC with pelvic and adrenal gland metastases. Ophthalmic examination revealed visual acuities of 20/50 OD and 20/25 OS, with vitreous cellularity graded at 1–2+ OD and 1+ OS, without evidence of clumping. Both optic discs were swollen, right more than left (Figures 1 and 2). Fluorescein angiography revealed marked disc leakage. There was no evidence of cerebral or meningeal metastasis by contrast-enhanced MRI of the head or in two separate analyses of cerebrospinal fluid (CSF). Serological evaluation revealed a paraneoplastic autoantibody profile consistent with SCLC: CRMP-5–IgG positive at 1:491,520; Purkinje cell cytoplasmic autoantibody, type 2 (PCA-2) at 1:491,520; anti-neuronal nuclear autoantibody, type 1 (ANNA-1, or anti-Hu) at 1:122,880 (normal values: negative at 1:120); and N-type neuronal voltage-gated calcium channel antibody at 0.05 nmol/l (normal is <0.03 nmol/l). The CSF reflected a CRMP-5 predominant intrathecal autoimmune response (CSF positive at 1:4096; PCA-2 at 1:128; ANNA-1 at 1:64; normal values: negative at 1:2). Paraneoplastic optic neuritis and vitreitis related to SCLC was diagnosed.
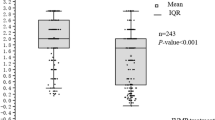
Triamcinolone acetonide (4 mg) was injected into the right vitreous and Solu-Medrol was given i.v. (1 g daily) for 5 days, followed thereafter by oral cytoxan (100 mg daily). Two weeks later, vision in the right eye stabilized. Vision in the left eye deteriorated to 20/50, and was injected with triamcinolone acetonide (4 mg). Three months after initial presentation, visual acuities were 20/40 OD and 20/50 OS, and there was no optic nerve swelling or cells in the vitreous (Figure 3). A significant partial tumour response was observed.
Case 2
A 59-year-old woman with a 43 pack-year smoking history, left hilar adenopathy, and segmental mastectomy for ductal breast carcinoma 22 months earlier presented with severe vision loss, vitreitis, and disc swelling. Visual acuity testing revealed CF at three feet OD and at two feet OS. Serological evaluation revealed CRMP-5-IgG at 1:30,720 (serum) and 1:1,120 (CSF), and N-type calcium channel autoantibody (serum, 0.05 nmol/l). We injected both eyes with triamcinolone acetonide (4 mg), the left eye two weeks after the right. She did not receive any form of systemic chemotherapy or immunomodulating therapy. After another two weeks, visual acuity was 20/200 OD and 20/300 OS. Inflammation and disc swelling were markedly decreased. Three months after initial presentation, visual acuities were 20/200 OD and 20/60 OS. Neither eye had evidence of inflammation.
Discussion
Intravitreal therapy with triamcinolone acetonide may be a valuable vision-sparing therapy for paraneoplastic autoimmune optic neuritis and vitreitis. Timely diagnosis is critical. Optic disc swelling and vitreitis are hallmarks of CRMP-5 autoimmunity related to occult or recurrent SCLC (rarely renal cell or thyroid carcinoma; not encountered yet with breast carcinoma).3 The favourable vision outcome in both cases of this report was accompanied by reduction in vitreous inflammation and optic nerve swelling. The relative contributions of high-dose intravenous Solu-Medrol, oral cyclophosphamide and cancer-directed therapy to the improvement in vision are uncertain. In the first case, vision in the left eye continued to deteriorate after the introduction of these therapies and improved only after IVTA. That patient's lack of tumour progression during 3 months of daily oral cyclophosphamide therapy is consistent with our hypothesis that cyclophosphamide may augment an effective antitumour immune response. In the second case, there was no concurrent systemic therapy, confirming the relative importance of intravitreal therapy for this disorder.
In summary, paraneoplastic autoimmune CRMP-5 optic neuritis and vitreitis is an important ocular disease that may be underdiagnosed. It appears to respond well to intravitreal corticosteroids.
References
Yu Z, Kryzer TJ, Griesmann GE, Kwang-kuk K, Benarroch EE, Lennon VA . CRMP-5 neuronal autoantibody: marker of lung cancer and thymoma-related autoimmunity. Ann Neurol 2001; 49 (2): 146–154.
Cross SA, Salomao DR, Parisi JE, Kryzer TJ, Bradley EA, Mines IA et al. Paraneoplastic autoimmune optic neuritis with retinitis defined by CRMP-5-IgG. Ann Neurol 2003; 54: 38–50.
Pittock SJ, Kryzer TJ, Lennon VA . Paraneoplastic antibodies co-exist and predict cancer, not neurological syndrome. Ann Neurol 2004; 56: 715–719.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pulido, J., Cross, S., Lennon, V. et al. Bilateral autoimmune optic neuritis and vitreitis related to CRMP-5-IgG: intravitreal triamcinolone acetonide therapy of four eyes. Eye 22, 1191–1193 (2008). https://doi.org/10.1038/sj.eye.6702959
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702959
Keywords
This article is cited by
-
An update on optic neuritis
Journal of Neurology (2023)