Abstract
Purpose
Ventilated patients in the intensive care unit (ICU) often develop exposure keratopathy. This predisposes to the development of bacterial keratitis, which in ICU is often bilateral, with a high risk of perforation. As regular examinations of all ventilated patients by ophthalmologists would be impractical, the purpose of this study was to assess whether ICU staff can screen reliably for keratopathy.
Methods
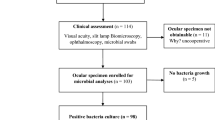
A prospective study was performed in a general adult ICU. Twice each week, two junior ICU doctors examined the lid position and ocular surface of all patients who had been continuously sedated for more than 24 h, using fluorescein and a pen torch with a blue filter. An ophthalmologist performed similar examinations using a portable slit lamp.
Results
A total of 48 ocular examinations were performed in 18 patients. Exposure keratopathy was found by the ophthalmologist in 37.5% of examinations and by ICU doctors in 31.3% of examinations. ICU doctors had a sensitivity of 77.8% and a specificity of 96.7% in detecting keratopathy, when compared with the findings of the ophthalmologist. All cases missed by ICU doctors had punctate erosions of less than 5% of the corneal surface. Keratopathy was significantly commoner in patients with incomplete lid closure than in patients with closed lids (70.0 vs28.9%; two-tailed Fisher's exact test P=0.027).
Conclusions
ICU staff can perform screening examinations for exposure keratopathy with reasonable sensitivity and specificity. Regular screening by ICU staff would facilitate appropriate treatment of exposure keratopathy and promote earlier identification of cases of keratitis.
Similar content being viewed by others
Introduction
Patients in the intensive care unit (ICU), especially ventilated patients, are at considerable risk of developing ocular surface disease. Sedation and muscle paralysis cause impaired blink reflexes and loss of eyelid muscle tone, while fluid imbalance and positive pressure ventilation may lead to chemosis. These factors often result in incomplete lid closure and consequent exposure keratopathy.1, 2, 3, 4 Whereas a conscious patient with intact corneal sensation will experience and report symptoms from even minor corneal damage, corneal disease may go unrecognised in comatose-ventilated patients until it reaches an advanced stage.
Ventilated patients are at particularly high risk of developing bacterial keratitis, especially with Pseudomonas aeruginosa. Pseudomonas is a common pathogen in the intensive care unit, colonising the airways of up to 30% of ventilated patients.5, 6 From here it may readily contaminate the ocular surface, for example when dispersed by routine suction of the airway.7 While Pseudomonas is unlikely to penetrate healthy corneal epithelium, it can invade the stroma via an abrasion within minutes of contact.8, 9, 10 The release of proteolytic enzymes and toxins and the associated immune response result in the development of an ulcer, which may rapidly progress to corneal perforation.11
There have been no large studies of bacterial keratitis in ICU. A literature review revealed reports of 22 patients who developed bacterial keratitis in intensive care, which in seven patients was bilateral.3, 7, 12, 13, 14, 15 Pseudomonas was the infectious agent in 20 of the 22 cases. Six patients died, and of the remaining 16, 11 suffered perforation requiring penetrating keratoplasty. In the largest series, the mean visual acuity of six surviving patients at discharge was 6/60.12
Although there is likely to be a significant reporting bias in favour of more severe cases among published case reports, it remains striking that so many of these cases were bilateral, with substantially worse outcomes than would be expected in an outpatient setting. A disproportionately large number were due to Pseudomonas, which is responsible for 24.8% of cases of bacterial keratitis in the general population.16 A key factor determining the prognosis may be lack of recognition of the risk of keratitis by ICU staff; failure to regularly examine the eyes of ventilated patients means that problems may not be detected until they reach an advanced stage.
Several of the authors of these case reports propose that exposure keratopathy is a key factor in the development of bacterial keratitis. Various small prospective studies have investigated the prevalence of corneal epithelial defects in the ICU. A study of 33 ventilated patients by Hernandez and Mannis17 found a 55% rate of corneal erosions. A prospective study by Merceica et al1 found an erosion rate of 42% in 26 patients; erosion was strongly associated with incomplete lid closure and deep sedation.
Various measures have been advocated to protect the eyes of ventilated patients, including regular instillation of topical lubricants or antibiotics, the creation of ‘moisture chambers’ to prevent tear evaporation using polyethylene film or polyacrylamide gel, and ensuring eyelid closure using either passive lid closure or tape.2, 3, 18, 19, 20, 21, 22 A systematic review identified only three small randomised controlled trials comparing eye care interventions in intensive care. No significant difference was found between polyethylene covers and lacrilube ointment in prevention of keratopathy, but polyethylene covers were found to be superior to methylcellulose drops. Duratears ointment was superior to passive eyelid closure.22
Mercieca et al performed a second study after the implementation of an eye care protocol based on regular use of ocular lubricants, and taping of incompletely closed eyes. The latter study found a substantially reduced corneal erosion rate of only 8.7% in 23 patients in whom the protocol had been correctly applied.2
Imanaka et al23 retrospectively reviewed medical notes and found that 3.5% of ventilated patients had documented corneal erosions, while a prospective study of 15 patients by the same authors found a corneal erosion rate of 60%. This discrepancy highlights how rarely keratopathy is detected unless ocular examinations are specifically performed to look for it. Routine examination by an ophthalmologist for every patient who was ventilated on the intensive care unit would be impractical. We therefore conducted a study to determine if intensive care staff without previous ophthalmic experience would be able to reliably screen for ocular surface disease in ventilated patients, using fluorescein and a pen torch with a cobalt blue filter.
Materials and methods
A prospective study was conducted in an 11-bed general adult ICU. Twice each week, every patient who had been ventilated and sedated continuously for more than 24 h had an ocular assessment by one of two junior ICU doctors with no previous experience in ophthalmology (JM, PA). A record was made of lid position, and the severity of conjunctival redness, chemosis, and discharge. The corneal epithelial surface was assessed with fluorescein and a pen torch with a cobalt blue filter. The presence of punctate or geographic erosions was noted, along with an estimate of the percentage of corneal area involved. All patients were examined within 4 h by the ophthalmologist (AK) who performed a similar assessment using a × 16 magnification portable slit lamp.
A record was made of age and sex, and an APACHE II score (an internationally recognised grading of severity of illness in critical care) was calculated for each patient at the time of assessment. Ventilator settings and central venous pressure were noted. The outcome of each patient's admission to ICU (death or discharge to a ward) was recorded retrospectively.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. Approval was granted by the Local Research Ethics Committee (reference 03.0116).
Results
Eighteen patients were examined. Four patients with prolonged stays in the ICU were examined twice and one patient three times. The findings for each eye were recorded separately, making a total of 48 ocular assessments. The mean age of patients was 57 years (range 21–80). Thirteen patients were male and five were female. Each patient had been sedated and ventilated for an average of 6 days at the time of ocular assessment. Three patients died in ICU and 15 were discharged to a ward.
The findings of examinations by ICU doctors and the ophthalmologist are summarised in Table 1. No ocular lubrication, taping, or polyethylene eye covers had been used for any of the patients. Similar rates of incomplete eye closure were found by both the ophthalmologist and ICU doctors (20.8 and 22.9% of eyes, respectively). Compared with the findings of the ophthalmologist, assessment of lid position by ICU doctors had a sensitivity of 90.0% and a specificity of 94.8% in detecting incomplete closure. ICU doctors recorded higher rates of chemosis, redness, and discharge than the ophthalmologist.
The ophthalmologist detected a higher rate of corneal erosions (37.5%) than the ICU doctors (31.3%). Examination for erosions by the ICU doctors had a sensitivity of 77.8% and a specificity of 96.7%, when compared to examination by the ophthalmologist.
Eyes found by the ophthalmologist to have incomplete lid closure had a much higher rate of keratopathy than eyes with closed lids (70.0 vs 28.9%; two-tailed Fisher's exact test P=0.027). There was no statistically significant association between the degree of keratopathy and age, sex, length of stay in ITU, APACHE score, ventilator settings, central venous pressure, degree of chemosis, redness, discharge, or mortality. No cases of bacterial keratitis occurred during the study.
Discussion
This study demonstrates that intensive care staff using fluorescein and a pen torch with a blue filter can assess eyes for incomplete lid closure and exposure keratopathy with reasonable sensitivity and specificity. Exposure keratopathy was identified in 37.5% of patients, a lower rate than in most previously published studies.1, 17, 23 Of those patients in whom corneal staining was missed by ICU doctors, none were found by the ophthalmologist to have geographic staining, and none had punctuate staining of more than 5% of the corneal surface; the eyes most severely affected by exposure keratopathy are thus least likely to be missed during a screening examination.
We suggest that ocular screening examinations by intensive care staff fulfil the criteria for a viable screening programme described by Wilson and Junger, being cheap, safe, acceptable, and reasonably sensitive and specific in identifying corneal disease.24 In terms of the specific requirements of a screening programme, we suggest the corneal epithelial defects can be regarded as a preclinical stage in the development of bacterial keratitis, which in ventilated patients carries a poor prognosis. Abnormal findings can be readily corroborated by an ophthalmologist. Exposure keratopathy is readily treatable with ocular lubricants and eyelid closure, while the benefits of earlier treatment of cases of bacterial keratitis are well established.2, 25
We advocate regular screening examinations by ICU doctors or nurses using fluorescein and a pen torch with a blue filter to identify patients with exposure keratopathy. Patients with exposure keratopathy can be treated by ICU staff and/or referred for assessment by ophthalmologists on the basis of locally agreed protocols. Once established, this practice would also help to identify any cases of bacterial keratitis at an early stage, allowing urgent assessment and treatment by ophthalmologists.
Although critically ill, admission of a patient to the ICU is undertaken on the basis that they have a significant chance of surviving with a reasonable quality of life following discharge. If bacterial keratitis develops in one or both eyes during their stay in ICU, the resulting loss of vision, or need for corneal graft surgery, may for some patients be the greatest consequence of their period of illness. We suggest that in many such cases ocular morbidity might be prevented or minimised by regular screening by ICU staff to allow recognition and treatment of problems at an early stage.
References
Mercieca F, Suresh P, Morton A, Tullo A . Ocular surface disease in intensive care patients. Eye 1999; 13: 231–236.
Suresh P, Mercieca F, Morton A, Tullo A . Eye care for the critically ill. Intensive Care Med 2000; 26: 162–166.
Kirwan JF, Potamitis T, El-Kasaby H, Hope-Ross MW, Sutton GA . Microbial keratitis in intensive care. BMJ 1997; 314: 433–434.
Wincek J, Ruttum MS . Exposure keratitis in comatose children. J Neurosci Nurs 1989; 21: 241–244.
Bergmans DCJJ, Bonten MJM, van Tiel FH, Gaillard CA, van der Geest S, Wilting RM et al. Cross-colonisation with Pseudomonas aeruginosa of patients in an intensive care unit. Thorax 1998; 53: 1053–1058.
Bertrand X, Thouverez M, Talon D, Boillot A, Capellier G, Floriot C et al. Endemicity, molecular diversity and colonisation routes of Pseudomonas aeruginosa in intensive care units. Intensive Care Med 2001; 27: 1263–1268.
Hilton E, Uliss A, Samuels S, Adams AA, Lesser ML, Lowy FD . Nosocomial bacterial eye infections in intensive-care units. Lancet 1983; 1(8337): 1318–1320.
Ramphal R, McNiece MT, Polack FM . Adherence of Pseudomonas aeruginosa to the injured cornea: a step in the pathogenesis of corneal infections. Ann ophthalmol 1981; 13: 421–425.
Stern GA, Weitzenkorn D, Valenti J . Adherence of Pseudomonas aeruginosa to the mouse cornea: epithelial v stromal adherence. Arch ophthalmol 1982; 100: 1956–1958.
Stern GA, Lubniewski A, Allen C . The interaction between Pseudomonas aeruginosa and the corneal epithelium. Arch ophthalmol 1985; 103: 1221–1225.
Fleiszig SMJ, Evans DJ . The pathogenesis of bacterial keratitis: studies with Pseudomonas aeruginosa. Clin Exper Optom 2002; 85: 271–278.
Parkin B, Turner A, Moore E, Cook S . Bacterial keratitis in the critically ill. Br J Ophthalmol 1997; 81: 1060–1063.
Hutton WL, Sexton RR . Atypical pseudomonas corneal ulcers in semicomatose patients. Am J Ophthalmol 1972; 73: 37–39.
Ommeslag D, Colardyn F, de Laey J . Eye infections caused by respiratory pathogens in mechanically ventilated patients. Crit care med 1987; 15: 80–81.
Johnson JL, Sagraves SG, Feild CJ, Block EF, Cheatham ML . An unusual case of corneal perforation secondary to Pseudomonas keratitis complicating a patient's surgical/trauma intensive care unit stay. Am Surg 2000; 66: 972–974.
Tuft SJ, Matheson M . In vitro antibiotic resistance in bacterial keratitis in London. Br J Ophthalmol 2000; 84: 687–691.
Hernandez EV, Mannis MJ . Superficial keratopathy in intensive care unit patients. Am J Ophthalmol 1997; 124: 212–216.
Parkin B, Cook S . A clear view: the way forward for eye care on ICU. Intensive Care Med 2000; 26: 155–156.
Farrell M, Wray F . Eye care for ventilated patients. Intensive Crit Care Nurs 1993; 9: 137–141.
Dua H . Bacterial keratitis in the critically ill and comatose patient. Lancet 1998; 351: 387–388.
Dawson D . Development of a new eye care guideline for critically ill patients. Intensive Crit Care Nurs 2005; 21: 119–122.
Joanna Briggs Institute for Evidence-Based Nursing & Midwifery. Eye care for intensive care patients. Best Practice 2002; 6 (1): 1–6.
Imanaka H, Taenaka N, Nakamura J, Aoyama K, Hosotani H . Ocular surface disorders in the critically ill. Anesth Analg 1997; 85: ndash;346.
Wilson JM, Junger CT . Principles and Practice of Screening for Disease, World Health Organisation Public Health Paper 34 World Health Organisation: Geneva, 1968, pp 26–37.
Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K et al. Microbial keratitis. Predisposing factors and morbidity. Ophthalmology 2006; 113: 109–116.
Acknowledgements
We thank Dr Jan Poloniecki, Reader in Medical Statistics, St George's University of London, for providing statistical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Part of this material has previously been published as a poster at the 2004 annual congress of the Royal College of Ophthalmologists. It has not been published in any other journal. Local ethics committee approval was granted before the study (reference 03.0116). No proprietary interests declared. No funding was received
Rights and permissions
About this article
Cite this article
McHugh, J., Alexander, P., Kalhoro, A. et al. Screening for ocular surface disease in the intensive care unit. Eye 22, 1465–1468 (2008). https://doi.org/10.1038/sj.eye.6702930
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702930
Keywords
This article is cited by
-
A comparison of antimicrobial regimen outcomes and antibiogram development in microbial keratitis: a prospective cohort study in Alexandria, Egypt
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
Incidence, risk factors and impact of protocolised care on exposure keratopathy in critically ill adults: a two-phase prospective cohort study
Critical Care (2018)