Abstract
Purposes
To investigate the degree of muscle slippage according to scleral suture techniques in extraocular muscle resection of rabbit eyes.
Methods
Twenty eyes from 10 rabbits (20 superior rectus muscles) were divided into four groups according to scleral suture techniques. The types of scleral suture technique used for the four groups were as follows: group 1 – double-arm mattress suture technique without midline suture; group 2 – double-arm mattress suture technique with midline suture; group 3 – long scleral tunnel suture technique without midline suture; and group 4 – long scleral tunnel suture technique with midline suture. Five superior rectus muscles were assigned to each group and they underwent resection with 6-0 prolene using one of the four suture techniques. The degree of muscle slippage was measured 3 months after the surgery, defined as the distance between the prolene materials at the centre of muscle insertion and the pre-placement suture.
Results
The mean degree of muscle slippage for treatment groups 1–4 was 2.3±0.62, 1.0±0.27, 1.5±0.45, 0.5±0.46 mm respectively. Group 1 had significantly more muscle slippage than groups 2–4 (P=0.006, P=0.046, P=0.001 respectively). Group 4 had the least slippage among the four groups, while group 3 had significantly more slippage than group 4 (P=0.009). The differences between groups 2 and 3 and between groups 2 and 4 were not statistically significant (P=0.083, P=0.077 respectively).
Conclusion
Long scleral suture technique is more effective method than double-arm mattress suture technique for the prevention of muscle slippage in rectus muscle resection. The addition of a midline suture of rectus muscle was helpful in the prevention of muscle slippage.
Similar content being viewed by others
Introduction
Slipped or lost muscle are well-known complications of strabismus surgery.1, 2, 3, 4 A slipped extraocular muscle (EOM) occurs when part or all of the EOM insertion slips posteriorly within its fascial sheath, leaving its anterior sheath connected to the globe. Lost muscle occurs as a result of detachment and retraction of the entire EOM and its capsule in a posterior direction through Tenon's capsule into the orbit.3, 4, 5, 6 Parks and Bloom5 reported that slipped muscle is probably caused when the pre-placed suture passes through the tendon capsule alone rather than through the tendon fibres, allowing the tendon fibres to slip posteriorly. Ohba et al7 presented a case in which the slipped muscle may have been caused by insufficient suturing and/or excessive rubbing of the eye by the patient.
The prevention of slipped muscle is important in strabismus surgery to increase the accuracy, reproducibility, and sustainability of the surgery. Chen et al8 reported that the frequency of muscle slippage after muscle surgery with an unsatisfactory outcome was 10.6%. Although numerous scleral suture techniques exist for securing the muscle or tendon, we are unaware of prior studies that correlated degree of muscle slippage with adequacy of scleral pass associated with these techniques. The technique with the least muscle slippage would be expected to improve surgical outcome in strabismus surgery.
We undertook this study to compare the degree of muscle slippage resulting from each of the four commonly used scleral suture techniques in rectus muscle resection of rabbit eyes.
Materials and methods
Experiments were performed on 10 healthy New Zealand white rabbits (2. 5–3.0 kg, 20 eyes) by one surgeon. All procedures followed the guidelines of the National Institutes of Health and the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. The 20 eyes were randomly allocated to four treatment groups, with each group undergoing surgical resection of the superior rectus muscle using a different scleral suture technique as described below. Resection in groups 1 and 2 was performed using a double-arm mattress suture technique with and without midline suture, respectively. Resection in groups 3 and 4 was achieved using a long scleral tunnel suture technique with and without midline suture respectively.
Each rabbit was anaesthetized with an intramuscular injection of ketamine and xylazine (1 : 1; 10 and 2 mg/kg, respectively). Proparacaine drops were placed in the conjunctival cul-de-sac to reduce blinking. Three months after surgery, we used non-absorbable double-arm 6-0 prolene (Ethicon) to measure the degree of muscle slippage, which was defined as the distance between suture materials at the centre of insertion and the pre-placement suture. Prolene is not commonly used suture material in modern strabismus surgery, but we thought that the non-absorbable suture material would be better for visualization of the degree of muscle slippage. The limbal conjunctiva and anterior Tenon's capsule were opened, the superior rectus muscle was exposed and the intermuscular membrane and check ligaments were dissected. The reason for which superior rectus muscles were used in our study was that it is the thickest extraocular muscle in rabbits, making it easy to observe. A double-arm suture was pre-placed by passage of a needle through the muscle substance at a distance of 5 mm from the insertion site using 6-0 prolene (non-absorbable). A locking bite on both margins of the muscle completed pre-placement of the double-arm suture. The muscle was cross-clamped with a hemostat just distal to the suture line, followed by transection of the muscle 1 mm anterior to the suture line. The muscle was disinserted and resected. The resected rectus was then securely attached to the sclera by the four scleral suture techniques. We spread the muscle broadly so that it was approximately the same width as the insertion to prevent central muscle sag.
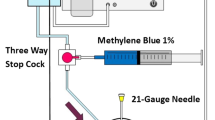
In group 1, each arm of the suture was brought out through the edge of the stump of the muscle's original insertion (Figure 1a). After that, the suture was gently sawed to bring the remaining muscle up to the original insertion without midline suture (double-arm mattress suture technique without midline suture, Figure 1b). In contrast, in group 2, one suture was then brought back through the insertion near its centre and through the central portion of the muscle from beneath. The suture was gently sawed to bring the remaining muscle up to the original insertion (double-arm mattress suture technique with midline suture, Figure 1c). In group 3, each needle passed intrasclerally on an oblique course, not through the tendon stump, creating a 3 mm tunnel (Figure 1d). The suture ends overlapped as they came out of the sclera resulting from the ‘crossed-swords’ intrascleral passage of the double-arm suture needles. The resected muscle was securely tied at the original insertion site (long scleral tunnel suture technique without midline suture, Figure 1e). In group 4, suture technique was similar to that of group 3 except that the sutures were brought through the central portion of the muscle from beneath (long scleral tunnel suture technique with midline suture, Figure 1f). After rectus muscle resection, ophthalmic antibiotic ointment was applied to the conjunctival sac. Three months after surgery, we measured the degree of muscle slippage as the distance between suture materials at the centre of insertion and the pre-placement suture. A Mann–Whitney U-test (SPSS 12.0 program for Windows) was used for the statistical analysis.
Schematic drawings of superior rectus muscle resection using double-arm mattress suture technique (a) without midline suture of rectus muscle (b, group 1), with midline suture of rectus muscle (c, group 2). Schematic drawings of long scleral tunnel suture technique (d) without midline suture of rectus muscle (e, group 3), with midline suture of rectus muscle (f, group 4).
Results
The mean degree of muscle slippage resulting from each of the four suture techniques were shown in Table 1 (Figure 2). Group 1 showed significantly more muscle slippage than groups 2–4 (P<0.05, Table 2). The degree of slippage in group 3 was more significant than in group 4 (P=0.009). Group 4 showed the least slippage. The differences between groups 2 and 3 and between groups 2 and 4 were not statistically significant (P>0.05, Table 2).
Photographs of muscle slippage after superior rectus muscle resection using double-arm mattress suture technique without midline suture of rectus muscle (a, group 1), with midline suture of rectus muscle (b, group 2). Photographs of muscle slippage after superior rectus muscle resection using long scleral tunnel suture technique without midline suture of rectus muscle (c, group 3), with midline suture of rectus muscle (d, group 4). Note the degree of muscle slippage (arrow).
Discussion
One of the well-known complications of strabismus surgery is slipped muscle and its repair is a highly challenging problem.3, 4, 5, 6 The extraocular rectus muscle most frequently slipped is medial rectus muscle and the frequent incidence of slipped medial rectus muscle may be due to the absence of intermuscular septum between the medial rectus muscle and oblique muscles in the sub-Tenon's space, as pointed out by Plager and Parks.9 Chatzistefanou et al10 suggested that this is because of the short arc of contact of the medial rectus muscle. Neural imaging is indispensable in locating the slipped muscle before attempts to retrieve and reattach it11 but Chatzistefanou et al10 reported that diagnostic imaging studies, including computerized tomography and magnetic resonance imaging may fail to differentiate accurately between empty connective tissue and muscle-tendon complex.
A slipped muscle should be suspected with any patient presenting after strabismus surgery with mild to moderate limitation of duction of the field of action of the muscle, with an unexpected undercorrection or overcorrection.8, 12, 13, 14 Differential intraocular pressure measurement and clinical manoeuvres such as forced ductions, active force generation tests, and saccadic velocity measurements support the diagnosis of large slipped muscle.8, 14 However, small slippage of muscle which is much more common, is unlikely to cause any of the specific clinical characteristic features, and its recognition is often missed. The ‘gold standard’ of diagnosis is direct intraoperative inspection, but if a muscle slippage is small, not suspected preoperatively, an intraoperative search may not be carried out.8
The strength of an extraocular muscle's reattachment to the globe in the early post-operative period depends on several factors. These include the location of the pre-placement suture, suture imbrication in the muscle or tendon,15 suture tensile strength, adequacy of the scleral pass, and the integrity of the knot.16 A study conducted by Coats et al15 suggested that the location of the pre-placement suture was another factor in muscle slippage. They reported that suture slippage occurred at a higher mean applied tension when sutures were placed 1.0 mm from the insertion (688 g) than at 0.5 mm (420 g) in resected human extraocular muscle preparations. Christiansen et al17 investigated the role of suture imbrication in the resulting tensile strength of the suture. The rectus muscles of 18 pigs randomly underwent either recession or resection using one of three imbrication suture techniques. There were no statistically significant differences in tensile strength between the three techniques.
Three months after surgery, in our investigation we compared and analyzed the four treatment groups and found that the long scleral tunnel suture technique resulted in less muscle slippage than the mattress suture technique, and that the addition of a midline suture also decreased muscle slippage. Our study evaluated the importance of the adequacy of the scleral pass for tensile strength by direct observation of the degree of muscle slippage according to the four scleral suture techniques commonly used in strabismus surgery. Our data also suggest that if strabismus surgery is performed by the same technique using the same suture materials, the inadequacy of scleral suture technique will be the single most important factor causing muscle slippage.
The limitation of our study is the anatomical differences in the fascial system between humans and rabbits. Another limitation is that the use of prolene rather than vicryl, which is the commonly used suture material in modern strabismus surgery, may limit the applicability of the findings to humans. However, we believe that the correlation between the degree of suture slippage and the scleral suture technique used is clearly demonstrated in our study.
In conclusion, among various scleral suture techniques in strabismus surgery, the long scleral tunnel suture technique is more effective than the double-arm mattress suture technique for the prevention of muscle slippage in rectus muscle resection and the addition of a midline suture further helps to prevent muscle slippage. We believe that proper application of the scleral suture techniques could prevent slipped muscle and improve surgical outcome in strabismus surgery.
References
Helveston EM . Atlas of Strabismus Surgery, 3rd edn. The CV Mosby Co: St Louis, 1985; 141–153.
Parks MM . Atlas of Strabismus Surgery, 1st edn. Harper & Row: Philadelphia, 1983; 116–131.
Hiller TL, Brown GC, Nelson LB, Fischer DH . The slipped rectus muscle. Ophthalmic Surg 1985; 16(5): 315–320.
Lenart TD, Lambert SR . Slipped and lost extraocular muscles. Ophthalmol Clin North Am 2001; 14(3): 433–442.
Parks MM, Bloom JN . The ‘slipped’ muscle. Ophthalmology 1979; 86(8): 1380–1396.
Bloom JN, Parks MM . The etiology, treatment and prevention of the ‘slipped muscle’. J Pediatr Ophthalmol Strabismus 1981; 18(1): 6–11.
Ohba M, Ohtsuka K, Hosaka Y, Ogawa K, Osanai H . A case of a slipped medial rectus muscle after strabismus surgery. Binocul Vis Strabismus Q 2004; 19(3): 165–168.
Chen SI, Knox PC, Hiscott P, Marsh IB . Detection of the slipped extraocular muscle after strabismus surgery. Ophthalmology 2005; 112(4): 686–693.
Plager DA, Parks MM . Recognition and repair of the slipped rectus muscle. J Pediatr Ophthalmol Strabismus 1988; 25: 270–274.
Chatzistefanou KI, Kushner BJ, Gentry LR . Magnetic resonance imaging of the arc of contact of extraocular muscles: implications regarding the incidence of slipped muscles. J AAPOS 2000; 4(2): 84–93.
Von Noorden GK . Binocular Vision and Ocular Motility, 6th edn. CV Mosby: St. Louis, 2002; 618–619.
Hong ST, Min BM . Recognition and repair of the slipped muscle. J Korean Ophthalmol Soc 1995; 36(3): 150–155.
Murray AD . Slipped and lost muscles and other tales of the unexpected. Philip Knapp Lecture. J AAPOS 1988; 2(3): 133–143.
Raz J, Bernhein J, Pras E, Saar C, Assia EI . Diagnosis and management of the surgical complication of postoperative ‘slipped’ medial rectus muscle: a new ‘tendon step test’ and outcome/results in 11 cases. Binocul Vis Strabismus Q 2002; 17(1): 25–33.
Coats DK, Paysse EA, Helveston EM . Secure suture placement for rectus muscle recession. Invest Ophthalmol Vis Sci 1994; 35(suppl): 2199 Abstract.
Estes RL, Sugar A . Knot integrity of coated synthetic absorbable sutures used for extraocular muscle surgery in a rabbit model. J Pediatr Ophthalmol Strabismus 1982; 19: 25.
Christiansen SP, Rettele GA, Soulsby ME, Wall RC . Tensile strength of insertional suture techniques in strabismus surgery. J Pediatr Ophthalmol Strabismus 1996; 33(2): 93–97.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, SM., Kim, SH. & Cho, Y. The difference in muscle slippage according to scleral suture techniques in rectus muscle resection of rabbit eyes. Eye 22, 564–568 (2008). https://doi.org/10.1038/sj.eye.6702803
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702803
Keywords
This article is cited by
-
Change in the location of the equator and recessed muscles in young rabbit eyes
Graefe's Archive for Clinical and Experimental Ophthalmology (2013)
-
The change of the extraocular muscle insertion after a slanted recession in rabbit eyes
Graefe's Archive for Clinical and Experimental Ophthalmology (2011)