Abstract
Purpose
To assess the agreement between ICare® rebound tonometer and Goldmann applanation tonometer in the hands of experienced and inexperienced tonometrists.
Patients and methods
Two tonometrists, experienced with both Goldmann applanation tonometry (GAT) and ICare® Tonometry (ICT) measured intraocular pressure (IOP), in a masked fashion, in 100 patients. In another series of 58 patients, ICT was performed by an inexperienced tonometrist and GAT by an experienced tonometrist.
Results
In approximately 80% of patients, the difference in IOP between GAT and ICT was ⩽2 mmHg in group 1 and ⩽3 mmHg in group 2. The 95% limits of agreement were −4.0–4.4 mmHg in group 1 and −6.0–5.0 mmHg in group 2.
Conclusion
ICT compares reasonably with GAT, in both experienced and inexperienced hands. Its ease of use, portability, and sterility make it an attractive tonometer. Its degree of accuracy in inexperienced hands would make it a useful instrument for health care workers with limited ophthalmic experience.
Similar content being viewed by others
Introduction
Goldmann applanation tonometry (GAT) is generally considered the gold standard method of measuring intraocular pressure (IOP).1 However, it has disadvantages: it requires a local anaesthetic (which may lower IOP),2 a slit lamp, a seated patient, and an experienced tonometrist; it is difficult in children, patients who are bedridden and those with corneal abnormalities; and the tonometer head needs chemical disinfection between patients.3
ICare® tonometry (ICT) is based on the principle of rebound tonometry.4, 5 The probe used is a disposable, thin magnetized steel wire with a round plastic tip. The moving magnet in the probe induces voltage in the enclosed solenoid. The probe bounces off the cornea and the impedance that is detected is used to calculate the IOP (Figure 1). This does not require topical anaesthesia, minimises corneal injury, and there is no risk of cross infection.6 It is potentially easier to use than GAT, and it was our impression, based on clinical experience, that it not only provides accurate IOP recordings, but that it can be accurately employed by inexperienced tonometrists. The aim of this study was to assess the agreement between ICT and GAT when performed by experienced and inexperienced tonometrists.
Subjects and methods
All patients attending a general clinic and a glaucoma clinic over a period of 2 months were potentially eligible for inclusion. The exclusion criteria were age less than 18 years, presence of severe corneal abnormalities, more than 2.00 D astigmatism, recent intraocular surgery, or active ocular infective disease. Written informed consent was obtained from all willing participants and the study was conducted according to the Declaration of Helsinki.
GAT was performed on a slit lamp (Haag-Streit, Bern, Switzerland) with a tonometer calibrated according to the manufacturer's guidelines. Before each reading, the measuring drum was reset to 10 mmHg. The tonometer head was disinfected according to the hospital infection control committee guidelines. IOP was measured after instillation of a drop of preservative-free lignocaine (4%) and fluorescein sodium (0.25%) solution.
The ICare® (Tiolat, Oy, Helsinki, Finland) software is preprogrammed for six measurements. An average of the best four readings, discarding the highest and lowest, is displayed as the final (6th) IOP. The software is also able to detect if all the parameters for measurement were acceptable. An unacceptable reading where the SD of the measurements is greater than normal is displayed with an error sign ‘−’. All measurements with error were discarded. Measurements were performed according to the manufacturer's guidelines. All patients were examined in sitting position.
The precision of ICT in experienced hands was determined by repeated measurements in the first 12 patients (repeatability coefficient 2.38 mmHg). Two studies were conducted:
ICT by experienced tonometrists
This comparison study was performed by two experienced ophthalmologists (examiners 1 and 2) on 200 eyes of 100 patients. These tonometrists were experienced in the use of both GAT and ICT.
Examiner 1 obtained an ICT measurement (average of six recordings) for each eye; then, after instilling topical anaesthesia, GAT was performed twice in a masked manner (examiner 1 performing the applanation and examiner 2 recording the IOP). ICT and GAT were then repeated with the examiners changing roles. The ICT readings are difficult to mask from the examiner; however, with this methodology, each examiner was unaware of the GAT measurement that they had obtained. The average IOPs by GAT and ICT were calculated for each eye. The IOPs of 100 right eyes were used for analysis.
ICT by inexperienced tonometrists
We investigated the agreement between IOP measurements by inexperienced tonometrists using ICT as compared to experienced tonometrists using GAT. A registered nurse with no previous experience in any form of tonometry was asked to use ICT after instruction and a trial run on four patients (eight eyes). Inexperience was considered to persist for a maximum of 15 measurements; hence, no single observer performed more than this. These 15 measurements did not include the trial run. There were six inexperienced tonometrists in total, and 58 patients were included in the study. The inexperienced tonometrists performed ICT on each eye and recorded the average of the six readings for each eye. An experienced tonometrist, masked to the ICT measurement, then performed GAT twice and recorded the average value.
The 95% limits of agreement between the two methods of tonometry were calculated by the Bland–Altman method.7 The mean (M) and standard deviation (SD) of the difference in IOP between GAT and ICT (GAT-ICT) were calculated. The 95% limits of agreement are calculated as M±(1.96 × SD). For the purposes of analysis, inexperienced tonometrists were pooled as if as they were a single observer. There was no wide variation in the readings by any of the observers.
Results
ICT by experienced tonometrists
Of the 100 patients (100 eyes) who entered the study, there were 45 males and 55 female patients with a mean age of 72 years. Thirty had glaucoma.
Table 1 shows the descriptive statistics of IOP measurements obtained with the two tonometers. In experienced hands, 81% of differences were within ±2 mmHg and 91% were within ±3 mmHg. There was no consistent over-or under-recording of the IOP by ICT.
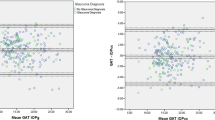
The mean difference in IOP between GAT and ICT (GAT-ICT) was 0.2 mmHg with a SD of 2.15. The 95% limits of agreement between the two tonometers using the Bland–Altman method were −4.0–4.4 mmHg. The agreement between the measurements, graphically analysed using the Bland–Altmann plot, is shown in Figure 2.
ICT by inexperienced tonometrists
Fifty-eight right eyes of 58 patients (31 males and 27 females) were included in this part of the study. The mean age was 67 years. Table 2 shows the descriptive statistics of IOP measurements obtained with the two tonometers. In inexperienced hands, 81% of patients had a mean difference of ⩽±3 mmHg. Here, the IOP measured using ICT was slightly higher than GAT, but the difference was not statistically significant.
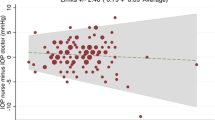
The mean difference between GAT and ICT in this group was −0.5 mmHg and SD was 2.8. The 95% limits of agreement between the two tonometers were −6.0–5.0 mmHg. Figure 3 shows the Bland–Altman plot to assess the agreement between ICT recorded by inexperienced tonometrists and GAT by experienced tonometrists.
Discussion
Recent reports about the accuracy (conformity with a standard) of ICT have been conflicting. In both normal and glaucomatous populations, van der Jagt and Jansonius8 reported ‘good agreement’ between ICT and GAT. The 95% limits of agreement for ICT compared with GAT in their study were −6–+7 mmHg. In contrast, Fernandes et al6 compared ICT with GAT in 43 university students and found a statistically significant difference between the mean IOP measurements. In addition, they reported that ICT systematically overestimated the IOP value by 1.34 mmHg on average when compared with GAT. The 95% limits of agreement in their study were ±3.98 mmHg. Similarly, Martinez-de-la-Casa et al9 also reported that ICT consistently overestimated IOP compared with GAT (median difference, 1.8±2.8 mmHg). In a recent report, Iliev et al10 have reported moderate to good agreement between these two devices. Here again, ICT recorded higher readings.
To some extent, the ‘agreement’ of a new method of measurement compared with the gold standard depends on the method of comparison. We used the Bland–Altman test of the limits of agreement. In addition, we examined the frequency distribution of the IOP difference between ICT and GAT.
Unlike the study by Fernandes et al6 and Iliev et al,10 in our study, ICT did not consistently under- or overestimate the IOP. The Bland–Altman analysis is generally considered the ideal method for assessing agreement of a new instrument with the gold standard.11 Using this method, we determined that 95% of ICT readings by experienced tonometrists are within −4.0–4.4 mmHg of those measured with GAT. In inexperienced hands the discrepancy was slightly greater. Finally, in more than 80% of patients, in both groups, the difference in IOP between GAT and ICT was ⩽3 mmHg.
Limitations of this study can be particularly addressed on comparison of ICT with GAT in inexperienced hands. Here, we used nurses who had no experience with tonometry. In this sub study, the patient numbers were relatively small, and the tonometrists were pooled as if they were a single, persistently inexperienced observer. The validity of this approach may be debatable. In addition, the number of patients with IOPs >30 or <10 mmHg was small; hence, we cannot comment on possible systematic errors at the lower or upper IOP range. In group 2, there were more patients with IOP above the normal range. Although this could be considered a reason for a wider range in the limits of agreement in this group, most patients with a GAT-ICT measurement of 5 mmHg or greater actually had IOPs in the normal range. However, as most patients had IOPs in the normal range, our conclusions are principally limited to this group. Assessment of the limits of agreement at higher IOPs would require further study.
In summary, ICT compares reasonably with GAT, in both experienced and inexperienced hands. Its ease of use, portability, and sterility make it an attractive tonometer. Furthermore, the intraobserver variation of GAT in the study by Dielemans et al12 was reported to be 1.50 mmHg (SD 1.96), and the limits of agreement for GAT vs GAT can be calculated as −2.3–5.3 mmHg. Hence, ICT in our study compares favourably. Also, its degree of accuracy in inexperienced hands would make it a useful instrument for health care workers with limited ophthalmic experience. It could be usefully employed in a number of settings, including optometric practice, general practice, and in the Emergency Department.
References
Kass MA . Standardizing the measurement of intraocular pressure for clinical research. Guidelines from the Eye Care Technology Forum. Ophthalmology 1996; 103 (1): 183–185.
Baudouin C, Gastaud P . Influence of topical anesthesia on tonometric values of intraocular pressure. Ophthalmologica 1994; 208 (6): 309–313.
Walia JS, Chronister CL . Possible iatrogenic transmission of Creutzfeldt-Jakob disease via tonometer tips: a review of the literature. Optometry 2001; 72 (10): 649–652.
Dekking HM, Coster HD . Dynamic Tonometry. Ophthalmologica 1967; 154 (1): 59–74.
Danias J, Kontiola AI, Filippopoulos T, Mittag T . Method for the noninvasive measurement of intraocular pressure in mice. Invest Ophthalmol Vis Sci 2003; 44 (3): 1138–1141.
Fernandes P, Diaz-Rey JA, Gonzalez-Meijome JM et al. Comparison of ICare rebound tonometer with Goldmann applanation tonometer in a normal population. Ophthal Physiol Opt 2005; 25: 436–440.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1 (8476): 307–310.
van der Jagt LH, Jansonius LM . Three portable tonometers, the TGDc-01, the ICARE and the Tonopen XL, compared with each other and with Goldmann applanation tonometry. Ophthalmic Physiol Opt 2005; 25 (5): 429–435.
Martinez -de-la-Casa JM, Gracia-Feijoo J, Castillo A et al. Reproducibility and clinical evaluation of rebound tonometry. Invest Ophthalmol Vis Sci 2005; 46 (12): 4578–4580.
Iliev ME, Goldblum D, Katsoulis K et al. Comparison of rebound tonometry with Goldmann applanation tonometry and correlation with central corneal thickness. Br J Ophthalmol 2006; 90: 833–835.
Bland JM, Altman DG . Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet 1995; 346 (8982): 1085–1087.
Dielemans I, Vingerling JR, Hofman A et al. Reliability of intraocular pressure measurement with Goldmann applanation tonometer in epidemiological studies. Graefes Arch Clin Exp Ophthalmol 1994; 232 (3): 141–144.
Acknowledgements
We are grateful to Arkon Proprietary Ltd, Mordialloc, Victoria, Australia, for the loan of the ICare® tonometer. We thank all the nurses who helped us with conducting this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary or commercial interest in ICare®
Rights and permissions
About this article
Cite this article
Abraham, L., Epasinghe, N., Selva, D. et al. Comparison of the ICare® rebound tonometer with the Goldmann applanation tonometer by experienced and inexperienced tonometrists. Eye 22, 503–506 (2008). https://doi.org/10.1038/sj.eye.6702669
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702669
Keywords
This article is cited by
-
Audit of outcomes following attendance at the City West drive-through IOP glaucoma clinic during the COVID-19 pandemic
Irish Journal of Medical Science (1971 -) (2022)
-
Agreement of patient-measured intraocular pressure using rebound tonometry with Goldmann applanation tonometry (GAT) in glaucoma patients
Scientific Reports (2017)
-
Twenty-four-hour efficacy of preservative-free tafluprost for open-angle glaucoma patients, assessed by home intraocular pressure (Icare-ONE) and blood-pressure monitoring
Japanese Journal of Ophthalmology (2016)
-
Handhabung von Reboundselbsttonometern der ersten und zweiten Generation
Der Ophthalmologe (2016)
-
Reboundtonometrie nach vitreoretinaler Chirurgie
Der Ophthalmologe (2015)