Abstract
Background
Macular holes have been described in association with benign vascular tumours of the retina. However, their successful treatment has not been reported.
Patients and methods
Three patients with macular holes associated with retinal vascular tumours had vitrectomy, peeling of the internal limiting membrane, and intraocular gas tamponade.
Results
In all three cases, the macular holes were successfully closed, and the visual acuity improved.
Conclusion
Macular holes associated with benign retinal vascular tumours respond to conventional macular hole surgical techniques.
Similar content being viewed by others
Case reports
Case 1
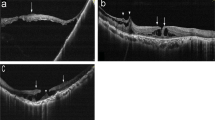
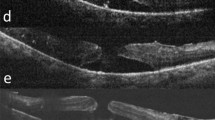
A 38-year-old woman, who had an isolated retinal angioma in the right eye, presented with a 2-week history of visual loss. The angioma had been treated 8 years previously for macular exudates which regressed. The exudates recurred and she received two additional laser treatments in the 2 months before her presentation. On examination, her visual acuity had declined from 6/9 to 6/36. There was an angioma approximately two disc diameters above the superotemporal arcade and exudates encroaching on the macula (Figure 1a). She had a full-thickness stage III macular hole (Figure 1b) and epiretinal membrane (Figure 1d). The patient underwent right vitrectomy, internal limiting membrane (ILM) peel, injection of 12% C3F8 gas, and cryotherapy and laser to the angioma. She had a plaque adherent to the surface of the angioma that bled slightly when it was avulsed during induction of a posterior vitreous detachment (Figure 1c). Six months later, her right visual acuity was stable at 6/24 and the macular hole was closed (Figure 1e). The exudates had partially regressed.
(a) Colour fundus photograph of right eye with isolated retinal angioma, surface neovascularization, drainage and feeder vessels, and surrounding lipid exudates. (b) Optical coherence tomogram of right macula showing full-thickness hole. (c) Intraoperative video still showing avulsed plaque (arrow) and bleeding on surface of angioma. (d) Intraoperative video still showing epiretinal membrane and macular hole stained with trypan blue. (e) Optical coherence tomogram showing closed macular hole, with residual subfoveal fluid, after vitrectomy and gas.
Case 2
A 57-year-old woman presented with a 3-month history of poor vision in the left eye. On examination her visual acuity was 6/60. There was a stage IV full-thickness macular hole, and a vasoproliferative tumour in the inferior peripheral retina, surrounded by exudates and shallow sub-retinal fluid. She had a pars plana vitrectomy, with ILM peel and injection of 12% C3F8, and the vasoproliferative tumour was treated with cryotherapy and laser. Six months after surgery, her vision improved to 6/24, the macular hole was closed, and the mass had shrunk with regression of the exudates and subretinal fluid.
Case 3
A 47-year-old man with noninsulin-dependent diabetes mellitus presented with poor vision in his left eye following uncomplicated cataract surgery. On examination, the left visual acuity was 6/18. There was a vasoproliferative tumour in the inferotemporal retina, and a stage II full-thickness macular hole. There was no evidence of diabetic retinopathy. He had a pars plana vitrectomy with ILM peel and injection of C3F8 gas. Six weeks after surgery, the macular hole was closed and the vision improved to 6/6 with a pinhole.
Comment
Isolated peripheral retinal angiomas and vasoproliferative tumours of the retina (VPTR) are benign glial lesions, which have in common telangiectasia and leakage of lipid and protein exudate.1, 2, 3 They are to be distinguished from haemangiomas associated with von Hippel–Lindau disease, which none of our patients had. Epiretinal membrane formation, macular pucker, cystoid macular oedema, and macular hole4 may all occur with these lesions, as can tractional macular detachment.5 The association between benign peripheral vascular lesions and these findings suggests that pathological changes occur specific to the macula.6 Laser treatment for peripheral retinal lesions can itself, over a period of time, be associated with retinal gliosis affecting the macula.7
It has been suggested that peripheral retinal telangiectasis with chronic exudate could cause vitreomacular traction resulting in the formation of a full-thickness macular hole.8 The mechanism remains unclear, but the authors suggest constitutional changes within the vitreous and the posterior hyaloid face.
This is the first case series report of the successful treatment of macular hole associated with benign peripheral vascular retinal lesions.
References
Shields CL, Shields JA, Barrett J, De Potter P . Vasoproliferative tumours of the ocular fundus. Classification and clinical manifestations in 103 patients. Arch Ophthalmol 1995; 113: 615–623.
Heimann H, Bornfeld N, Vij O, Coupland SE, Bechrakis NE, Kellner U et al. Vasoproliferative tumours of the retina. Br J Ophthalmol 2000; 84: 1162–1169.
Singh AD, Shields CL, Shields JA . von Hippel–Lindau disease. Surv Ophthalmol 2001; 46: 117–142.
Raju B, Majji A, Jalali S . von Hippel angioma in South Indian subjects—a clinical study. Retina 2003; 23: 670–674.
McDonald HR, Schatz H, Johnson RN, Abrams GW, Brown GC, Brucker AJ et al. Vitrectomy in eyes with peripheral retinal angioma associated with traction macular detachment. Ophthalmology 1996; 103: 329–335.
Wise GN, Wangvivat Y . The exaggerated macular response to retinal disease. Am J Ophthalmol 1966; 61: 1359–1363.
Rosa Jr RH, Goldberg MF, Green WR . Clinicopathologic correlation of argon laser photocoagulation of retinal angiomas in a patient with von Hippel–Lindau disease followed for more than 20 years. Retina 1996; 16: 145–156.
Jaycock PD, Thomas D, Zakir R, Laidlaw DAH . Retinal telangiectasis in association with macular hole formation. Eye 2004; 18: 342–343.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors has a proprietary interest in this case, nor are they in receipt of financial support
Rights and permissions
About this article
Cite this article
Clare, G., Yorston, D., Charteris, D. et al. Successful treatment of macular holes associated with peripheral retinal vascular tumours. Eye 21, 419–420 (2007). https://doi.org/10.1038/sj.eye.6702423
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702423