Abstract
Aims
Smoking is associated with several serious eye diseases. Awareness of smoking and blindness, and its potential to act, as a stimulus to assist stopping smoking has not been investigated.
Methods
A cross-sectional survey using a structured interview of adult patients attending district general hospital ophthalmology, general surgery, and orthopaedic clinics. The interview investigated the awareness and fear of blindness for three established smoking-related diseases, and a distractor condition (deafness), and the likelihood that smokers would quit on developing early signs of each condition.
Results
Response was 89.1% (358/402). In all, 183 (51.1%) of responders were male and 175 (48.9%) female. Only 9.5% of patients believed that smoking was definitely or probably a cause of blindness, compared with 92.2% for lung cancer, 87.6% for heart disease, and 70.6% for stroke. Patients ranked their fear of each of the five conditions, scoring five for the most feared and one for the least feared. Patients were significantly (P<0.01) less fearful of blindness (mean score 2.80) than lung cancer (3.89), heart disease (3.58), and stroke (3.35). About one-half of smokers stated that they would definitely or probably quit smoking if they developed early signs of blindness or the three established smoking-related conditions, with no significant differences in proportions for these four conditions.
Conclusion
The findings suggest that awareness of the risk of blindness from smoking is low, but that the fear of blindness is as compelling a motivation to quit as fear of lung cancer, heart disease, and stroke. The link between smoking and eye disease should be publicised to help reduce smoking prevalence.
Similar content being viewed by others
Introduction
The association between smoking and eye diseases is well established, especially for age-related macular degeneration (AMD), though also for thyroid eye disease and cataract among others.1 AMD is the principal cause of blindness in developed countries. It is the commonest cause for blind registration in the UK, where there are approximately 214 000 (95% confidence interval (CI): 151 000–310 000) individuals with impaired vision secondary to AMD,2 and an estimated 54 000 people with visual impairment and almost 18 000 with blindness caused by AMD related to smoking.3
There is minimal understanding of the public's awareness about smoking as a risk factor for blindness. While certain diseases, such as lung cancer and heart disease, receive a high profile in health-promotional campaigns as illnesses caused by smoking, this is not the case for smoking-related eye diseases. It is known that if smokers believe their health will improve as a result of stopping smoking, they have an increased chance of quitting.4 We have not identified any studies examining the level of awareness of the link between smoking and eye diseases and the possible impact such awareness would have on smoking behaviour. Preliminary findings from New Zealand5 on the impact of television advertisement campaigns on calls to a national Quitline service suggest that information about the link between smoking and blindness may be a potent stimulus for smokers to try and quit.
We performed a cross-sectional study to explore the level of knowledge of the link between smoking and eye disease and the likely impact of that knowledge among UK patients attending ophthalmic and other outpatient departments. Our hypothesis was that few patients would be aware of the risk of eye disease by smoking, but that awareness of the risks to eyesight from smoking would be a strong stimulus for smokers to quit.
Methods
Subjects and setting
Adults attending ophthalmology, orthopaedics, and general surgery clinics at a UK District General Hospital between May and June 2004 were invited to participate. We excluded persons aged less than 18 years, or who were unable to give written informed consent or complete the interview. The survey was restricted to individuals with competent English language. The hospital serves a local population of approximately 261 000 residents, of whom 49% are male and 51% are female, 11% are non-white (mainly of South Asian origin), and 20% are aged over 60. Bolton has many areas of high social deprivation, as indicated by a variety of deprivation indices.6, 7 Approximated social groups for the local census indicated that 80% of the local population are from low socioeconomic groups.7
Data collection
Data were collected through a structured interview in the three clinic waiting areas, which included demographic details (age, sex, ethnicity, and job title) and smoking status. Socioeconomic status was assigned from job title using the Registrar General's Occupational Social Class classification, and we then divided participants into high and low socioeconomic status.
Subjects were asked about their awareness of a link between smoking and four smoking-attributable conditions (lung cancer, heart disease, stroke, and blindness) and a ‘distractor’ condition (deafness). The latter condition (for which we are unaware of evidence of a link with smoking) was included for comparison purposes, and to reduce the risk of over-reporting for the questions relating to blindness because of subjects guessing the focus of the study. Fear of developing each of the five conditions was assessed by asking subjects to rank the five conditions from most to least feared. Responses were scored from a score of 5 (most feared) to 1 (least feared). For each condition, smokers were asked the likelihood that they would quit smoking if they developed early signs of the condition.
Statistical analysis
Data from the orthopaedic and general surgery patients were combined for the analysis. Statistical analysis was carried out using SPSS version 10.1 (SPSS Inc., Chicago, IL, USA) or Confidence Interval Analysis (CIA) software.8 Differences in means and medians were calculated using the CIA software. The Wilcoxon signed rank and Mann–Whitney tests were used to compare fear rankings for paired and independent sample data, respectively. CIs for differences in proportions were calculated using CIA software, using Wilson's method for paired data and Newcombe's method for nonpaired data.
Approval for this study was granted by the Bolton Local Research Ethics Committee.
Results
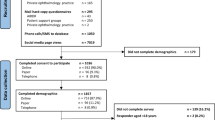
Response and demographic profile of patients
The researcher approached 402 patients attending the outpatient clinics, of whom 358 (89.1%) agreed to participate. Demographic details of the clinic attenders are given in Table 1.
The age of participants ranged from 18 to 93 years. The mean age was 59.3 years and was higher among the eye clinic attenders. The numbers of men and women were approximately equal. The population was predominantly (95%) white. There were no statistically significant differences in sex and ethnicity between eye and other clinic attenders. A significantly higher proportion of eye clinic attenders than attenders at other clinics were from occupational social classes III–V (difference 11% (95% CI: 1–22%)).
Awareness of the link between smoking and blindness
The proportion of clinic attenders who believed smoking ‘definitely’ or ‘probably’ caused stroke, heart disease, and lung cancer was high—over 70% for stroke, over 85% for heart disease, and over 90% for lung cancer (Table 2). However, only 12% of eye clinic patients and 7% of other clinic attenders believed smoking caused blindness, with a similar proportion responding positively to the ‘distractor’ condition—deafness.
There was a highly statistically significant difference for each comparison between the proportions believing that heart disease, stroke, or lung cancer was caused by smoking and the proportion believing that blindness could be caused by smoking. The proportion of smokers (5%) believing that smoking caused blindness was lower than for nonsmokers (11%), though the difference 6% (95% CI: −2 to 11%) was not significant.
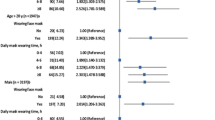
Fear of blindness and other conditions
The median (mean) fear ranking score was 4 (3.9) for lung cancer, 4 (3.6) for heart disease, 3 (3.4) for stroke, 2 (2.8) for blindness, and 1 (1.4) for deafness. The differences in rankings between each of the four other conditions and the ranking for blindness were all statistically significantly different (P<0.001, Wilcoxon signed rank test). The median (mean) score for fear of blindness was 3 (3.1) among eye clinic attenders and 2 (2.6) among other clinic attenders, with a significant difference in rankings (Mann–Whitney test, P=0.01). The median (mean) score for fear of blindness was 2 (2.9) among nonsmokers and 2 (2.5) among other clinic attenders, with a significant difference in rankings (Mann–Whitney test, P=0.02).
Stimulus to quit with early signs of disease
The difference in proportions stating that they would quit with early signs of blindness compared with early signs of lung cancer was 4% (95% CI: −2 to 9%), and for early signs of stroke or heart disease compared with early signs of blindness was 2% (95% CI: −3 to 6%). These differences were not statistically significant.
Discussion
This is the first study to have examined the awareness and likely impact of the link between smoking and blindness. Strengths of this project included a large sample size and an excellent response rate. We found that few patients, both smokers and nonsmokers, were aware that smoking could cause blindness. This contrasted with high levels of awareness that smoking causes lung cancer and cardiovascular disease. The perceived risk of blindness from smoking, however, was only slightly greater than that for the distractor variable condition, deafness. Although patients were slightly less fearful of blindness from smoking than developing lung cancer or cardiovascular diseases, there was no significant difference in the proportion of smokers who stated that they would quit smoking on developing early signs of eye disease, compared with developing early signs of the three other established smoking-related conditions. We acknowledge that hospital clinic samples may not be representative of the local population (though in practice this is difficult to determine in a hospital sample), and therefore the knowledge and attitudes reported may not be representative of those among the general public.
The findings suggest that increasing the awareness of the link between smoking and blindness may be an effective additional approach to encouraging smoking cessation. The low level of awareness of the link between smoking and blindness, even among eye clinic patients, may reflect both a lack of general public and patient information on the matter and further lack of effective advice about smoking at ophthalmic clinics.
Our finding that fear or awareness of early signs of eye disease might stimulate smoking cessation suggests that health-promotional campaigns and health warnings providing information about the risks of smoking-related eye diseases and blindness to smokers may well be effective in eye clinic and optometry settings, as well as with the general public. Further work exploring these fears as a motivator to stop smoking among the general public in different population settings is planned.
We have developed a leaflet targeted at smokers attending eye clinics and optometrists and propose to carry out further work investigating current practice in relation to providing smokers with advice and support in these settings (this leaflet is available at www.nwash.co.uk).
References
Solberg Y, Rosner M, Belkon M . The association between cigarette smoking and ocular diseases. Surv Ophthalmol 1998; 42: 535–547.
Owen CG, Fletcher AE, Donoghue AR, Rudnicka AR . How big is the burden of visual loss caused by age related macular degeneration in the United Kingdom? Br J Ophthalmol 2003; 87: 312–317.
Kelly SP, Thornton J, Lyratzopoulos G, Edwards R, Mitchell P . Smoking and blindness. Strong evidence for the link, but public awareness lags. Br Med J 2004; 328: 357–358.
Walters N, Coleman T . Comparison of the smoking behaviour and attitudes of smokers who attribute respiratory symptoms to smoking with those who do not. Br J Gen Pract 2002; 52: 132–134.
Wilson N, Hodgen E, Mills J, Wilson G, Field A, Thomson G . Journal article on smoking and blindness prompts significantly more calls to Quitline. N Z Med J 2002; 115: 199–200.
Office for National Statistics. Neighbourhood Statistics. London: ONS, 2005. Accessed 23/02/2005. http://neighbourhood.statistics.gov.uk/
Bolton Metropolitan Council. Access Bolton: People in Bolton. Bolton: Bolton Metropolitan Council, 2003. Accessed 23/02/2005. http://www.bolton.gov.uk/pls/portal92/docs/7084.HTM#socio
Bryant T . Confidence Interval Analysis: Version 2.0.0. Southampton: University of Southampton, 2000.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing Interest: RE is an unpaid chairman of North West Action on Smoking and Health, a campaigning charity
Rights and permissions
About this article
Cite this article
Bidwell, G., Sahu, A., Edwards, R. et al. Perceptions of blindness related to smoking: a hospital-based cross-sectional study. Eye 19, 945–948 (2005). https://doi.org/10.1038/sj.eye.6701955
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701955
Keywords
This article is cited by
-
Smoking kills you, littering butts damages others too: analysing sustainable consumer behaviour in the era of circular economy
Environment, Development and Sustainability (2022)
-
Advice about diet and smoking for people with or at risk of age-related macular degeneration: a cross-sectional survey of eye care professionals in the UK
BMC Public Health (2013)
-
Can genetic risk information for age-related macular degeneration influence motivation to stop smoking? A pilot study
Eye (2012)
-
Awareness of blindness and other smoking-related diseases and its impact on motivation for smoking cessation in eye patients
Eye (2011)
-
Awareness of smoking risks and attitudes towards graphic health warning labels on cigarette packs: a cross-cultural study of two populations in Singapore and Scotland
Eye (2010)