Abstract
Aims
The mucopolysaccharidoses (MPS) are a heterogeneous group of rare disorders characterised by accumulation of glycosaminoglycans within multiple organ systems. This study aimed to determine the prevalence and severity of ocular complications in patients with MPS.
Methods
Clinical ophthalmic features and electrodiagnostic results of 50 patients with a diagnosis of MPS were retrospectively reviewed.
Results
A total of 79% of MPS IH patients had a visual acuity of less than 6/12 equivalent in their better eye, compared to 44% of MPS IH/S and 25% of MPS VI patients. In total, 16% of MPS IH and 25% of MPS IH/S had severe corneal opacification, compared to 38% of MPS VI patients. 16% of MPS IH patients had optic atrophy; 21% of MPS VI patients had mild disc swelling, 29% had markedly swollen discs, and 14% had optic atrophy. One patient with MPS IH, one with MPS IH/S and six with MPS VI had ocular hypertension. One MPS VI patient had glaucoma that required topical therapy. Nine patients with MPS IH had electrodiagnostic evidence of retinopathy, as did one MPS VI patient.
Conclusions
Ocular complications causing significant reduction in vision are common in MPS. The majority of MPS I and MPS VI patients have corneal opacification, which can lead to difficulties in diagnosis and monitoring of glaucoma, optic disc changes, and retinopathy.
Similar content being viewed by others
Introduction
The mucopolysaccharidoses (MPS) are a group of disorders characterised by accumulation of glycosaminoglycans (GAG) within a wide variety of tissues, including those of the eye. The MPS have been historically subdivided into different types depending on clinical manifestations and they encompass a wide spectrum of phenotypes, ranging from those disorders, which are fatal in the first months of life to those compatible with a normal lifespan.1, 2 The MPS result from inherited abnormalities of specific lysosomal enzymes involved in degradation of GAG3 (Table 1).
Ophthalmic complications are common in MPS, including corneal opacification. This occurs as a result of GAG accumulation both intra- and extracellularly in corneal epithelium, keratocytes, stroma, and endothelium, with subsequent disruption of the optically important arrangement of collagen fibrils.4, 5 Ocular hypertension and glaucoma occur in MPS due to GAG acumulation within anterior chamber structures. This can lead to narrowing of the anterior chamber angle,6, 7 and deposition within trabecular cells may lead to obstruction of outflow.8, 9 Retinopathy occurs as a result of GAG accumulation within retinal pigment epithelial cells and interphotoreceptor matrix, leading to progressive photoreceptor loss.10 Optic nerve abnormalities are reported to be common in MPS.11 Optic disc swelling and subsequent optic atrophy occur secondary to raised intraocular pressure (IOP),12 or as a result of compression of the nerve by GAG in thickened dura and sclera,11, 13 or accumulation of GAG within ganglion cells.14
Mucopolysaccharidoses type I (MPS I) is caused by abnormalities of the enzyme α-L-iduronidase. This manifests as a phenotypic spectrum of skeletal, cardiac, and respiratory problems.3, 15 MPS IH Hurler syndrome presents with facial dysmorphism and respiratory disease in early life, and patients may be referred to the ophthalmologist once the diagnosis is already made for detection of associated corneal opacification.15 Retinopathy is a common complication in older children with MPS IH but may be difficult to detect because of corneal opacity.16 Electroretinography (ERG) usually demonstrates a reduction in dark-adapted b-wave in the early stages. MPS IS Scheie has milder systemic and ophthalmic manifestations, and MPS IH/S Hurler/Scheie is an intermediate phenotype.3
Hunter syndrome (MPS II) exhibits a wide variation in clinical severity, with seizures and learning difficulties as common features.3 MPS III Sanfilippo results from defects in four different enzymes (Table 1), which result in clinically indistinguishable phenotypes. Patients with MPS III Sanfilippo present with learning difficulties and severe behavioural disturbance, but have mild systemic manifestations.3 The main feature of MPS IV Morquio is the severe skeletal changes.17 Maroteaux-Lamy (MPS VI) results in a spectrum of phenotypic severity, including short stature and variable skeletal deformities.3 Affected individuals are usually intellectually normal.
The ocular management of many patients with MPS has traditionally been conservative because of their short lifespan and intellectual impairment. However, modern treatments including bone marrow transplantation (BMT) and enzyme replacement therapy (ERT) in MPS I can result in a longer and better quality life for many patients.18, 19, 20 ERT is currently licensed for use in MPS I (as Laronidase) and is undergoing clinical trials for use in MPS II and VI. ERT improves respiratory function, endurance, joint mobility, growth (in prepubertal patients), and hair and facial appearance in MPS I.21 The effects of these treatments on the ophthalmic complications of MPS is, at present, unknown. This study aimed to determine the prevalence and severity of ophthalmic complications in patients with MPS seen at the Willink Unit, Royal Manchester Children's Hospital, and Manchester Royal Eye Hospital.
Methods
We retrospectively reviewed the notes of patients seen in the Manchester Royal Eye Hospital paediatric ophthalmology clinic from 1996 to 2003 with a diagnosis of MPS. The patients were identified from the paediatric ophthalmology diagnostic database. The age of the patient at most recent examination was documented, as well as the visual acuity, presence of strabismus, refractive error, and IOP measurement if possible (performed by noncontact air-puff tonometry in the clinic). The degree of corneal opacification was subjectively graded (by a single observer, ICL) as mild (+), moderate (++), or severe (+++). The appearance of the optic disc, if visualisation was possible, was noted as normal, atrophic, swollen, or cupped. The presence of retinopathy was determined by dilated fundal examination of the retina and by electroretinography (ERG). Visual evoked potentials (VEPs) were performed in cases of suspected optic nerve dysfunction.
Results
A total of 50 patients were identified with a diagnosis of MPS. Among them, 19 patients had MPS IH Hurler, nine had MPS IH/S Hurler/Scheie, and three had MPS IS Scheie. There were two patients with MPS II Hunter and one patient had MPS III Sanfilippo. There were 16 patients with MPS VI Maroteaux-Lamy.
The age range of the patients with MPS IH was 4 months to 23 years, with a mean of 6 years and 2 months. The age range of the MPS IH/S patients was 2–22 years and the mean was 12 years 9 months. The range of the MPS IS patients was 7–16 years and the mean was 11 years 4 months. The MPS II patients were 10–12 years old with a mean of 11 years, and the MPS III patient was 20 years old. The age range of the MPS VI patients was 2–21 years with a mean of 8 years 8 months.
Refraction was available in 14 patients with MPS IH Hurler. In all, 13 patients (93%) were hypermetropic and one patient (7%) was myopic. All seven MPS IH/S Hurler/Scheie and all three MPS IS Scheie patients who had refraction available were hypermetropic. One MPS II patient was hypermetropic and one was myopic, and the MPS III patient was myopic. Out of the 12 patients, 11 (92%) with refraction available and a diagnosis of MPS VI Maroteaux-Lamy were hypermetropic and one (7%) was myopic.
Out of 19, 15 (79%) patients with MPS IH Hurler had a visual acuity of less than 6/12 equivalent in their better eye, compared to four out of nine (44%) patients with MPS IH/S Hurler/Scheie. Two patients (11%) with MPS IH Hurler had visual acuity 3/60 or less in their better eye. The severe visual impairment was attributed in one patient (patient 10H, Table 2) to cortical visual impairment, and to optic atrophy secondary to previous raised intracranial pressure in another (patient 13H, Table 2). Six out of 19 (32%) of MPS IH patients had amblyopia, compared to three out of nine (33%) patients with MPS IH/S. All three patients with MPS IS Scheie had vision better than 6/12 in at least one eye, and only one had amblyopia. Both MPS II Hunter patients had 6/6 vision or better in both eyes and neither had amblyopia. The MPS III patient had severe learning difficulties, and his vision was measured at 6/38 with Cardiff cards. Four out of 16 (25%) of patients with MPS VI Maroteaux-Lamy had vision less than 6/12 in the better eye. Two (13%) MPS VI patients had vision 3/60 or less in their better eye, and both these patients both had optic atrophy secondary to previous raised intracranial pressure (patients 3VI and 16VI, Table 7). Seven out of 16 (44%) MPS VI patients had amblyopia.
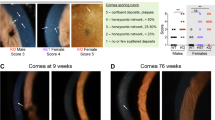
All MPS I patients had some degree of corneal opacification (Graph 1), although one patient with MPS IH/S had previously undergone penetrating keratoplasty with a centrally clear donor cornea in both eyes at 3 and 6 years follow-up (patient 4H/S, Table 3). Nine out of 19 (47%) patients with MPS IH Hurler had mild corneal opacification (Figure 1), seven out of 19 (37%) had moderate opacification, and three out of 19 (16%) had severe corneal opacification. Three out of eight (38%) patients with MPS IH/S Hurler/Scheie had mild corneal opacification, three (38%) had moderate, and two (25%) had severe opacification. Two out of three (66%) MPS IS Scheie patients had mild opacification and one had moderate opacification (Table 4). All MPS II Hunter and MPS III Sanfilippo patients had clear corneas (Tables 5 and 6). Five out of 16 (31%) MPS VI Maroteaux-Lamy patients had mild corneal opacity, four (25%) had moderate, and six (38%) severe (Figure 2). One MPS VI patient with severe corneal opacification had undergone successful penetrating keratoplasty in one eye with maintenance of a clear donor cornea at 5 years, but had limitation of vision due to optic atrophy (patient 3VI, Table 7).
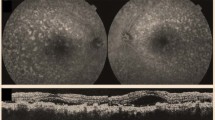
In total, 16 (84%) MPS IH Hurler patients had normal optic discs and three (16%) had optic atrophy (Graph 2). Only one (11%) of the MPS IH/S patients had disc swelling and the other eight patients all had normal discs. All three MPS IS Scheie patients had healthy discs. Both patients with MPS II Hunter had mild disc swelling, and the patient with MPS III Sanfilippo had temporal optic atrophy. Four out of 14 (29%) MPS VI Maroteaux-Lamy patients had normal discs, three (21%) had mild disc swelling, four (29%) had markedly swollen discs, two (14%) had optic atrophy (Figure 3), and one (7%) had a cupped disc due to raised IOP. The view of the optic disc was obscured by marked corneal opacification in two patients with MPS VI.
The incidence of ocular hypertension and glaucoma in the MPS patients was low (Graph 3). Only one patient with MPS IH Hurler had ocular hypertension with IOPs of 22 mmHg right and 25 mmHg left eye, and normal optic discs. All other MPS IH patients (95%) had IOPs less than 21 mmHg. One patient with MPS IH/S had IOPs of 31 mmHg right and 33 mmHg left with normal optic discs. All MPS IS Scheie and MPS III Sanfilippo patients had IOPs less than 21 mmHg. IOP measurements were not available for the MPS II Hunter patients. In total, 13 patients with MPS VI had IOP measurements documented. Of these, five (38%) had IOPs greater than 21 mmHg and a further two had IOPs greater than 30 mmHg (15%). One of these had IOPs of 33 mmHg in both eyes, marked corneal opacification and a cup : disc ratio of 0.7 both eyes. This patient (4VI, Table 7) was started on topical antihypertensive medication (latanoprost).
IOP was higher in the patients with more severe corneal opacification (Graph 4). The mean IOP in MPS I patients with mild corneal opacification was 13.23±4.75 mmHg. The mean IOP was 17.00±3.98 mmHg in those MPS I patients with moderate corneal opacification and 19.40±7.19 mmHg in those with severe corneal opacification (ANOVA analysis, P=0.03). As a statistically significant difference between the three groups was found, a Tukey multiple comparison test was carried out. This showed that IOP in the mild corneal opacification group was significantly different from both the moderate and severe groups, while there was no significant difference between the moderate and severe corneal opacification groups. In the MPS VI patients, the mean IOP was 16.00±5.44 mmHg in those with mild corneal opacity, 20.66±7.86 mmHg in those with moderate opacity and 24.00±5.56 mmHg in patients with severe opacification (ANOVA analysis, P=0.05). Tukey's multiple comparison test demonstrated a statistically significant difference in IOP between the mild and severe corneal opacity groups, but not between mild and moderate, or moderate and severe corneal opacity groups.
Retinal pigment epithelial atrophic changes were documented in two (11%) patients with MPS IH Hurler, five (56%) patients with MPS IH/S Hurler/Scheie (Figure 4), and two (66%) patients with MPS IS Scheie. All MPS II Hunter and MPS III Sanfilippo patients had clinically normal fundii. There were three MPS VI Maroteaux-Lamy patients in whom it was impossible to get a clear fundal view due to the marked corneal opacification, but all of those fundii visualised were clinically normal.
A total of 13 patients with MPS IH Hurler had undergone ERGs. Nine (69%) of these had reduced b-waves in dark-adapted conditions, and one of these had reduced b-waves when light adapted also. Only one patient with MPS IH/S Hurler/Scheie had an ERG performed, which showed reduced b-waves on dark adaptation. Electroretinography was not available on any patients with MPS IS Scheie or MPS II Hunter. The MPS III Sanfilippo patient demonstrated reduced amplitude of their dark-adapted ERG. Eight patients with MPS VI Maroteaux-Lamy underwent ERGs, and one (12%) had a reduced dark-adapted amplitude (patient 6VI, Table 7). VEPs were performed on nine patients with MPS IH Hurler. Four (44%) of these were abnormal (patients 7H, 9H, 10H, and 13H). Only one patient with MPS IH/S Hurler/Scheie had VEPs performed, which were normal. All MPS II Hunter and MPS III Sanfilippo patients had VEPs, which were all normal. Seven patients with MPS VI Maroteaux-Lamy underwent VEPs. Of these, four (57%) were abnormal (patients 2VI, 3VI, 8VI, and 4VI).
Four (21%) patients with MPS IH Hurler had exotropia, two (11%) had esotropia, and one (5%) had a fourth nerve palsy. Four (44%) patients with MPS IH/S Hurler/Scheie had exotropia. No MPS IS Scheie or MPS II Hunter patient had any manifest deviation. The MPS III Sanfilippo patient had an alternating exotropia. One (6%) MPS VI Maroteaux-Lamy patient had exotropia and three (19%) were esotropic.
Two patients with MPS I Hurler (patients 15H and 17H, Table 2) developed bilateral posterior subcapsular cataracts. These patients had both undergone two previous bone marrow transplants. Eight MPS IH patients were examined after undergoing bone marrow transplant with a follow-up of 1 month–9 years, and mean follow-up of 5 years 5 months. The age range of these patients was 15 months–23 years, with a mean of 8 years 5 months. Two of these patients (25%) had mild corneal opacification, five (62.5%) had moderate, and one (12.5%) marked opacification. Six (75%) of these patients had visual acuities less than 6/12 Snellen equivalent in the better eye.
Discussion
This is the first large case series to comprehensively describe the ophthalmic features seen in patients with MPS. This study demonstrates that corneal opacification is a common feature in all MPS I subgroups (Hurler, Hurler/Scheie, and Scheie) and also in MPS VI Maroteaux-Lamy.22, 23, 24, 25, 26, 27, 28 Our results suggest that corneal opacification tends to be more severe in MPS VI Maroteaux-Lamy than MPS I subgroups. We have confirmed that corneal opacity is not a prominent feature in MPS II or MPS III.24, 29
Retinopathy is known to occur to a variable degree in all MPS I subgroups, MPS II Hunter and moderate or severe retinopathy is a common feature of MPS III Sanfilippo.16, 30, 31 Pigmentary retinopathy may also occur in MPS IV Morquio.32 We have electrodiagnostic evidence of retinopathy in a high proportion (69% of those who had ERGs performed) of MPS I Hurler patients, and clinical retinal pigment epithelial changes suggestive of retinopathy in a significant proportion of MPS IH/S Hurler/Scheie (56%) and MPS IS Scheie patients (66%). In keeping with other reports, the patient with MPS III Sanfilippo had ERG evidence of retinopathy consistent with their reduced visual acuity. Retinopathy has not previously been reported in MPS VI, but we found one patient with ERG attenuation despite normal acuity and a normal retinal examination, suggesting that retinopathy may be an additional feature in some cases of MPS VI Maroteaux-Lamy.
The incidence of optic disc swelling in MPS I was much lower than reported in previous studies. Collins et al11 described optic disc abnormalities in a series of 108 MPS patients and found that 57% of patients with MPS IH Hurlers and 43% of MPS IH/S Hurler/Scheie patients had optic disc swelling. None of the MPS IH patients and only one patient with MPS IH/S had disc swelling in the current study. Our figures may perhaps be attributed to better recognition and management of raised intracranial pressure in this group of patients. Our findings in the MPS VI Maroteaux-Lamy patients were similar to those of Collins, who found 41% to have optic disc swelling and 8% atrophy.11 Optic atrophy occurred secondary to previous episodes of raised intracranial pressure in three out of six patients in this study. Visual loss was profound (to perception of light level only) in these patients, suggesting that raised intracranial pressure and subsequent optic atrophy is a significant cause of severe visual loss in MPS patients.
There have been no previous studies of the incidence of ocular hypertension or glaucoma in MPS patients. Previous case reports have described open angle glaucoma in MPS IH,9, 33, 34 MPS IH/S,35 and MPS VI.36 Angle closure glaucoma has been reported in MPS IS Scheie,37 MPS IH/S,38 MPS II Hunter,39 and MPS VI Maroteaux-Lamy.36 In our study, there was a low incidence of ocular hypertension and glaucoma in all MPS I subgroups, with only one MPS IH Hurler patient and one MPS IH/S Hurler/Scheie patient having raised IOP. Ocular hypertension was more common in the MPS VI Maroteaux-Lamy patients, with 38% having IOP greater than 21 mmHg and a further 15% having IOP greater than 30 mmHg, perhaps due to the more marked corneal changes in these patients. Only one MPS patient required topical glaucoma medication, and there were no cases of acute glaucoma in our series. However, the incidence of open angle glaucoma could be expected to increase with age.
Diagnosis and monitoring of ocular hypertension and glaucoma is often difficult in patients with MPS due to their multiple physical and intellectual difficulties hampering assessment of IOP and visual fields. In addition, the presence of corneal opacity may cause difficulties in visualisation of the optic disc, and assessment of disc cupping may also be made more difficult due to coexistent disc abnormalities. Corneal thickening due to GAG deposition may also lead to falsely high IOP readings. We found a statistically significant relationship between IOP and degree of corneal opacification in MPS I and MPS VI patients. Future studies are needed to assess the correlation between corneal opacification, corneal thickness, and IOP readings in MPS patients.
This study demonstrates that visual impairment is common in MPS patients, and that a significant proportion of both MPS I Hurler (11%) and MPS VI Maroteaux-Lamy (13%) patients have marked visual impairment with a Snellen acuity of 3/60 or less in their better eye. Optic atrophy secondary to raised intracranial pressure was the cause of severe visual impairment in three of the four patients in this study with vision 3/60 or less, highlighting the importance of early diagnosis and monitoring of raised intracranial pressure in these patients. The overall incidence of visual impairment (measured as vision worse than 6/12 Snellen equivalent in the better eye) was higher in the MPS IH Hurler (79%) and MPS IH/S Hurler/Scheie (44%) than in the MPS VI patients (25%), despite the more marked corneal opacification and higher incidence of optic nerve involvement in the MPS VI patients. This may perhaps reflect the low incidence of retinopathy in MPS VI, or be attributed to nonocular causes of visual impairment in MPS I patients such as cortical visual impairment. This study demonstrates that mild corneal opacity is compatible with excellent Snellen acuity, although patients may experience glare and reduced contrast sensitivity, visual modalities not assessed here. Refractive error, which occurs due to refractive changes in the cornea,40 squint and amblyopia were all common in this series of MPS patients.
Previous studies have suggested a possible beneficial effect of BMT on the ocular manifestations of MPS.41, 42 Summers et al41 prospectively followed 11 patients after BMT for up to 2.8 years and found evidence of clearing of corneal opacification, resolution of optic nerve oedema, and stabilised or improved retinal function. Gullingsrud et al found in a retrospective study that six out of 20 patients had clinical improvement in corneal clouding and five patients had increase in clouding at 7–24 months after BMT. In total, 81% of patients had improvement in ERG in the first year, followed by a slowly progressive deterioration in all patients over a further 5 years.42 Our study has not analysed the effect of BMT on the ophthalmic complications, but there was still a significant proportion (75%) of MPS IH patients with viusal impairment who had undergone previous BMT. The effects of ERT, and combined early treatment with BMT and ERT, on the ocular manifestations of MPS are not yet defined, and further studies are needed to determine whether ocular complications are stabilised or improved by these treatments.
Patients with MPS require regular ophthalmic assessment to detect, monitor, and treating ocular complications. The profound effect of poor vision on a young patient, who may also be suffering multiple physical and intellectual problems, means that the ocular management of these patients is a crucial part of their multidisciplinary care. In addition, the ophthalmologist may pick up signs of raised intracranial pressure, which as this study demonstrates is a major cause of visual impairment.
References
Neufeld EF, Muenzer J . The mucopolysaccharidoses. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds). The Metabolic and Molecular Bases of Inherited Disease, Vol 8. The McGraw-Hill Companies, Inc.: Berkshire, UK, 2001, pp 3421–3452.
Lorincz AE . The mucopolysaccharidoses: advances in understanding and treatment. Pediatr Ann 1978; 7(2): 104–122.
Wraith JE . The mucopolysaccharidoses: a clinical review and guide to management. Arch Dis Child 1995; 72: 263.
Rawe IM, Leonard DW, Meek KM, Zabel RW . X-ray diffraction and transmission electron microscopy of Morquio syndrome type A cornea: a structural analysis. Cornea 1997; 16(3): 369–376.
Quantock AJ, Meek KM, Fullwood NJ, Zabel RW . Scheie's syndrome: the architecture of corneal collagen and distribution of corneal proteoglycans. Can J Ophthalmol 1993; 28(6): 266–272.
Mullaney P, Awad AH, Millar L . Glaucoma in mucopolysaccharidosis 1-H/S. J Pediatr Ophthalmol Strabismus 1996; 33(2): 127–131.
Cantor LB, Disseler JA, Wilson FM . Glaucoma in the Maroteaux-Lamy syndrome. Am J Ophthalmol 1989; 108(4): 426–430.
McDonnell JM, Green WR, Maumenee IH . Ocular histopathology of systemic mucopolysaccharidosis, type II-A (Hunter syndrome, severe). Ophthalmology 1985; 92(12): 1772–1779.
Spellacy E, Bankes JL, Crow J, Dourmashkin R, Shah D et al. Glaucoma in a case of Hurler disease. Br J Ophthalmol 1980; 64: 773–778.
Lazarus HS, Sly WS, Kyle JW, Hageman GS . Photoreceptor degeneration and altered distribution of interphotoreceptor matrix proteoglycans in the mucopolysaccharidosis VII mouse. Exp Eye Res 1993; 56(5): 531–541.
Collins MLZ, Traboulsi EI, Maumenee IH . Optic nerve head swelling and optic atrophy in the systemic mucopolysaccharidoses. Ophthalmology 1990; 97: 1445–1449.
Goldberg MF, Scott CI, McKusick VA . Hydrocephalus and papilloedema in the Maroteaux-Lamy syndrome (mucopolysaccharidoses type VI). Am J Ophthalmol 1970; 69: 969–975.
Beck M, Cole G . Disc oedema in association with Hunter's syndrome: ocular histopathological findings. Br J Ophthalmol 1984; 68(8): 590–594.
Chan CC, Green WR, Maumenee IH, Sack GH . Ocular ultrastructural studies of two cases of the Hurler syndrome (systemic mucopolysaccharidoses I-H). Ophthalmic Paediatr Genet 1982; 2: 3–19.
Cleary MA, Wraith JE . The presenting features of mucopolysaccharidoses type IH (Hurler syndrome). Acta Paediatr 1995; 84(3): 337–339.
Caruso RC, Kaiser-Kupfer MI, Muenzer J, Ludwig IH, Zasloff MA, Mercer PA . Electroretinographic findings in the mucopolysaccharidoses. Ophthalmology 1986; 93(12): 1612–1616.
Northover H, Cowie RA, Wraith JE . Mucopolysaccharidosis type IVA (Morquio syndrome): a clinical review. J Inherit Metab Dis 1996; 19(3): 357–365.
Wraith JE . Enzyme replacement therapy in mucopolysaccharidosis type I: progress and emerging difficulties. J Inherit Metab Dis 2001; 24(2): 245–250.
Kakkis ED, Muenzer J, Tiller GE, Waber L, Belmont J, Passage M et al. Enzyme-replacement therapy in mucopolysaccharidoses I. N Eng J Med 2001; 344: 182–188.
Vellodi A, Young EP, Cooper A, Wraith JE, Winchester B, Meaney C et al. Bone marrow transplantation for mucopolysaccharidosis type I: experience of two British centres. Arch Dis Child 1997; 76(2): 92–99.
Wraith JE . Lysosomal disorders. Semin Neonatol 2002; 7(1): 75–83.
Viestenz A, Shin YS, Viestenz A, Naumann GO . Ocular manifestation of mucopolysaccharidosis I-S (Scheie's syndrome). Klin Monatsbl Augenheilkd 2002; 219(10): 745–748.
Rummelt V, Meyer HJ, Naumann GO . Light and electron microscopy of the cornea in systemic mucopolysaccharidosis type I-S (Scheie's syndrome). Cornea 1992; 11(1): 86–92.
Francois J . Metabolic disorders and corneal changes. Dev Ophthalmol 1981; 4: 1–69.
Tremblay M, Dube I, Gagne R . Corneal changes in Scheie disease. (Mucopolysaccharidosis type I S). J Fr Ophthalmol 1979; 2(3): 193–197.
Girard B, Hoang-Xuan T, D'Hermies F, Savoldelli M, Bennouna M, Poenaru L et al. Mucopolysaccharidosis type I, Hurler–Scheie phenotype with ocular involvement. Clinical and ultrastructural study. J Fr Ophthalmol 1994; 17(4): 286–295.
Laver NM, Friedlander MH, McLean IW . Mild form of Maroteaux-Lamy syndrome: corneal histopathology and ultrastructure. Cornea 1998; 17(6): 664–668.
Casanova FH, Adan CB, Allemann N, de Freitas D . Findings in the anterior segment on ultrasound biomicroscopy in Maroteaux-Lamy syndrome. Cornea 2001; 20(3): 333–338.
Spranger J, Cantz M, Gehler J, Liebaers I, Theiss W . Mucopolysaccharidosis II (Hunter disease) with corneal opacities. Report on two patients at the extremes of a wide clinical spectrum. Eur J Pediatr 1978; 129(1): 11–16.
Gills JP, Hobson R, Hanley WB, McKusick VA . Electroretinography and fundus oculi findings in Hurler's disease and allied mucopolysaccharidoses. Arch Ophthalmol 1965; 74: 596–603.
Leung LS, Weinstein GW, Hobson RR . Further electroretinographic studies of patients with mucopolysaccharidoses. Birth Defects Orig Artic Ser 1971; 7(3): 32–40.
Dangel ME, Tsou BH . Retinal involvement in Morquio's syndrome (MPS IV). Ann Ophthalmol 1985; 17(6): 349–354.
Lalive d'Epinay S, Reme CE . Congenital glaucoma in Hurler's syndrome and in Lowe's syndrome. Clinical and electron microscopy findings. Adv Ophthalmol 1978; 36: 80–89.
Nowaczyk MJ, Clarke JTR, Morin JD . Glaucoma as an early complication of Hurler's disease. Arch Dis Child 1988; 63: 1091–1093.
Girard B, Hoang-Xuan T, D'Hermies F, Savoldelli M, Bennouna M, Poenaru L et al. Mucopolysaccharidosis type I, Hurler–Scheie phenotype with ocular involvement. Clinical and ultrastructural study. J Fr Ophthalmol 1994; 17(4): 286–295.
Cantor LB, Disseler JA, Wilson FM . Glaucoma in the Maroteaux-Lamy syndrome. Am J Ophthalmol 1989; 108(4): 426–430.
Quigley HA, Maumenee AE, Stark WJ . Acute glaucoma in systemic mucopolysaccharidosis I-S. Am J Ophthalmol 1975; 80(1): 70–72.
Mullaney P, Awad AH, Millar L . Glaucoma in mucopolysaccharidosis 1-H/S. J Pediatr Ophthalmol Strabismus 1996; 33(2): 127–131.
Kaiden JS . Angle closure in a patient with Hunter's syndrome. J Ocul Ther Surg 1982; 1: 250.
Traboulsi EI, Maumenee IH . Ophthalmologic findings in mucolipidosis III (pseudo-Hurler polydystrophy). Am J Ophthalmol 1986; 102: 592–597.
Summers CG, Purple RL, Krivit W, Pineda R, Copland GT, Ramsay NK et al. Ocular changes in the mucopolysaccharidoses after bone marrow transplantation. A preliminary report. Ophthalmology 1989; 96(7): 977–984.
Gullingsrud EO, Krivit W, Summers CG . Ocular abnormalities in the mucopolysaccharidoses after bone marrow transplantation. Longer follow-up. Ophthalmology 1998; 105(6): 1099–1105.
Acknowledgements
We thank Anna Maino, specialist registrar at Manchester Royal Eye Hospital for help with analysis of the data, and the medical illustration department of Manchester Royal Eye Hospital for help with the illustrations.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work has been presented as a poster at the Royal College of Ophthalmologists Annual Congress, Manchester, May 2004 and as a presentation at the European Paediatric Ophthalmology Society meeting in Manchester, October 2004.
Rights and permissions
About this article
Cite this article
Ashworth, J., Biswas, S., Wraith, E. et al. The ocular features of the mucopolysaccharidoses. Eye 20, 553–563 (2006). https://doi.org/10.1038/sj.eye.6701921
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701921