Abstract
Purpose
To report the safety and efficacy of combined trabeculotomy and trabeculectomy (CTT) in advanced primary developmental glaucoma with corneal diameter 14 mm or more.
Patients and Methods
A total of 74 (121 eyes) consecutive patients aged 3 days–100 months (median, 10 months) with advanced developmental glaucoma were included. Primary CTT was performed by a single surgeon at a tertiary eye care centre in India over a 13-year period. The main outcome measures were changes in and final levels of intraocular pressure (IOP), corneal clarity, visual acuity, and refractive status.
Results
Mean preoperative IOP was 29.4±7.6 mmHg (range, 10–56 mmHg) and mean postoperative IOP was 15.5±6.6 mmHg (range, 6–38 mmHg) (P<0.0001) with percentage reduction of 44.5±27.1. Kaplan–Meier survival analysis revealed 3-, 6-, 9-, 12-, 24-, 48-, and 72-month success rates of 86.5, 80.5, 78.1, 75.5, 71.1, and 60.5%, respectively. Majority (80.5%) of the patients were myopes with mean spherical equivalent of 5.8±4.5D (range, 0.75–22.0D). Using various age-appropriate testing procedures, at the final follow-up visit, 14 patients (41.2%) had age-appropriate normal visual acuity and 20 patients (58.8%) had subnormal visual acuity. Best-spectacle-corrected visual acuity of ⩾20/60 was achieved in seven patients (26.9%). There were no sight-threatening intraoperative and postoperative complications.
Conclusion
CTT is safe and effective in patients with advanced primary developmental glaucoma. It offers good IOP control with a low complication rate, with about one-third of patients achieving a visual acuity of 20/60 or better.
Similar content being viewed by others
Introduction
In India, developmental glaucoma is more frequent and more severe than in other parts of the world.1, 2, 3 According to a population-based study, the prevalence of developmental glaucoma has been estimated to be 1 in 3300 in the Indian state of Andhra Pradesh and the disease accounts for 4.2% of all childhood blindness.1, 4 In order to reduce the burden of blindness due to developmental glaucoma, early surgery has been advocated.5 There has been much debate about the choice of surgery for management of advanced developmental glaucoma. Although goniotomy is reported to be safe and successful when performed by experienced surgeons,6, 7, 8 trabeculotomy ab externo is easier and more predictable than goniotomy.9, 10, 11 Nonetheless, the prerequisite for successful goniotomy is a clear cornea to visualize the angle structures during the procedure.5, 10 However, compared to the Western and European population, a large number of Indian children (>80%) present with a severe cloudy cornea at birth, and goniotomy is technically impossible.2, 3, 12 Furthermore, goniotomy is challenging in cases of advanced developmental glaucoma and Barkan13 felt that eyes with corneal diameter >15 mm are not suitable for goniotomy. The most compelling argument favouring primary combined trabeculotomy–trabeculectomy (CTT) in developmental glaucoma in India is the higher incidence of successful control of intraocular pressure (IOP) with a single procedure already reported by us.12, 14, 15, 16, 17, 18
The aim of the present study was to evaluate the safety and efficacy of CTT in advanced primary developmental glaucoma with corneal diameter of 14 mm or more.
Methods
Patients
A retrospective chart review was performed of all patients who underwent CTT for advanced primary developmental glaucoma from 1 January 1990, through 31 December 2002. In case of bilateral affliction, the choice of simultaneous bilateral surgery was offered to all patients after thoroughly discussing the risks and benefits with the parents. In all, 12 patients (16.2%) underwent CTT as the second surgical intervention while in the remaining patients (62, 83.8%) CTT was performed as the initial procedure. All surgeries were performed by a single surgeon (AKM) with the informed consent of parents of all patients. We excluded patients who had less than 3 months of follow-up from the present study. The use of primary CTT as the main therapeutic modality was approved by the Ethics Committee for Human Research at the LV Prasad Eye Institute.
The study population consisted of different types of primary developmental glaucoma identified based on the basis of classification system of Hoskins et al:19 congenital (existing at or usually before birth), infantile (occurring from birth until age 2 years), and juvenile (age 2 years or older).
Examination procedures
Intraocular pressure
IOP was measured with a Perkin's hand-held applanation tonometer in the early phase of inhalation anaesthesia using 1% halothane, and IOP was measured by the Goldmann applanation tonometer in children who cooperated for a slit-lamp examination in the postoperative period.
Visual function
Visual function could not be quantitatively assessed in most of the cases in the preoperative period due to severe corneal clouding and Haab's straie rendering these eyes extremely photophobic. However, visual acuity could be recorded in most of the children during the follow-up period. Various suitable procedures were used to assess visual acuity in the follow-up period as has been reported earlier by us.17, 18 In brief, these included preferential looking assessments using Teller Acuity Cards (Vistech Consultants, Inc. Dayton, OH, USA) which measure resolution acuity, a 3-m folding chart containing Lea symbols to measure recognition acuity, and the logMAR chart.20 For children to whom these procedures could not be applied, the ability to fix and follow light was used. Although the ability to fix and follow light does not provide a measure of visual acuity, it can help identify children who are totally blind.21
Visual acuity was reported according to the World Health Organization classification of visual impairment.22 These categories have been defined based on the best-corrected visual acuity in the better eye and consist of (a) no impairment (⩾20/60), (b) low vision (<20/60–20/400), and (c) blindness (<20/400).
Refraction
Retinoscopy was not possible in the preoperative period due to corneal oedema in almost all the children. However, retinoscopy was performed, using a streak retinoscope (Heine, Beta 2000) under cycloplegia (cyclopentolate 1% eye drops) in the postoperative period, after 6 weeks in eyes with clear corneas. It was performed in the office on cooperative children and during examination under anaesthesia (EUA) with uncooperative children. In such children, the refractive correction was prescribed based on the objective value after appropriate adjustments for cycloplegia. In cooperative children, where the retinoscopic reflex was irregular and dull due to the presence of a corneal scar, subjective procedures such as axial length measurements and keratometry were used to obtain a rough estimate, which was then used as a baseline value for further refinements in the subjective refraction.23, 24
Data collection
All preoperative, surgical, and postoperative parameters were entered in a computer-friendly data entry form. Any intra- and perioperative surgical complications and retreatments were also recorded.
Outcome measures
The outcome measures included preoperative and postoperative IOPs, corneal clarity and diameter, visual acuity, refractive errors, success rate, time of surgical failure, and complications. The incidence of endophthalmitis (if any) and anaesthetic morbidity and mortality were analysed.
Surgical procedure
The surgical technique employed in all cases was primary CTT. This technique has been previously described by us.3, 12, 14, 15, 16, 17, 18 In brief, the Schlemm's canal was dissected under a partial thickness limbal-based triangular scleral flap and trabeculotomy ab externo was performed on both sides of the radial incision. Trabeculectomy was then performed in the usual manner. In cases of bilateral affliction, after completion of surgery on the first eye, the second eye was operated using a similar technique but with a new set of instruments, drapes, drops, gown, gloves, etc, simulating a surgical procedure on a different patient.
Postoperative regimen
All patients were treated with topical 1% cyclopentolate twice daily for 1 month and the corticosteroid-antibiotic preparation (0.1% betamethasone and neomycin) six times a day, tapered gradually over a 6-week period. All patients were examined 1, 2, and 3 days after surgery, followed by examination in the office at the end of 1, 3, and 6 weeks and in the office every 3 months thereafter. At each visit, patients were examined fully with a slit-lamp biomicroscope, and the anterior chamber depth, corneal appearance, IOP, bleb appearance, and fundus picture were documented. Patients who could not be examined in the office were scheduled for EUA at the end of 1, 3, and 6 weeks and every 3 months thereafter.
Success criteria
Surgical success and failure were defined before data analysis. The surgery was considered a complete success when the IOP was less than 16 mmHg in patients examined under general anaesthesia or less than 21 mmHg in patients who were old enough to be examined with the slit-lamp and when there was no progression of disc cupping or corneal diameter. Qualified success was defined as cases in which such pressure was maintained with a single topical antiglaucoma medication (timolol maleate 0.25% twice daily) or when ocular hypotony was present without visual loss. Failure was defined as IOP greater than 21 mmHg or the development of hypotony-related maculopathy or other sight-threatening complications.
Statistical analyses
To avoid bias, we evaluated the results in terms of patients rather than eyes.25 For the purpose of statistical analysis, only one randomly chosen eye was included for patients with a bilateral affliction. Results are expressed as mean±standard deviation (SD). A P-value <0.05 was considered statistically significant. Cumulative success probability was determined using the Kaplan–Meier survival analysis. Spherical equivalent (SE) was used to analyse the refractive errors. SE was calculated by adding half the cylindrical value to the spherical value of the refractive error. Subjects with SE higher than +0.50D were considered as having hyperopia. However, SE ⩾−0.50D was considered for analysis of myopia.
The effect of individual clinical and demographic variables on the outcome of treatment was analysed by a series of univariate Cox proportional hazards models.26 Any factor with P<0.15 from the univariate analysis was then entered into a multivariate analysis using the forward step-wise method. The effect of each category of a two-category variable was assessed by keeping either of the two categories as the reference. Results are expressed as hazard ratios (HRs) with 95% confidence intervals (CIs). P<0.05 was considered as statistically significant.
Using the SPSS (SPSS for Windows, version 10.0, SPSS, Chicago, IL, USA) software, analyses of continuous data were made using the paired ‘t’-test. Ordinal data were analysed by the Wilcoxon signed rank test.
Results
Demographic data
A total of 74 patients (121 eyes) were included in the study. The demographic data (age, gender, type of glaucoma, and follow-up) are provided in Table 1. The mean age at presentation was 21.1±23.2 months (range, 3 days–100 months; median, 10 months). The ratio of males to females was 3 : 2 and 47 (63.5%) patients were affected in both eyes. The mean follow-up was 22.1±29.0 months (range, 3–108 months; median, 10.5 months).
Intraocular pressure
The mean preoperative IOP was 29.4±7.6 mmHg (range, 10–56 mmHg). Although some of the patients had normal IOP preoperatively, they were operated because they were receiving antiglaucoma medication and the diagnosis of glaucoma was confirmed based on a comprehensive ocular examination that also included corneal diameters. At the final follow-up visit, the mean IOP was significantly lower than the preoperative level (15.5±6.6 mmHg; range, 6–38 mmHg) (P<0.0001, paired t-test) with percentage reduction in IOP of 44.5±27.1 mmHg. Preoperatively, 20 of 157 eyes (12.8%) were receiving antiglaucoma medication (mean 0.5±0.7, range 0–3). However, at the last follow-up 11 of 157 eyes (7.0%) required antiglaucoma medication (mean 0.2±0.4, range 0–1) for the control of IOP (P=0.088, Wilcoxon's signed rank test).
Corneal diameter and clarity
Mean (±SD) horizontal corneal diameters at presentation were 14.6±0.8 mm (range, 14.0–18.0 mm). Preoperatively, nine eyes (12.2%) had clear corneas and the decision for surgery in these eyes was based on high IOP, megalocornea, and gonioanamoly suggestive of congenital glaucoma. Two-third of the eyes (49, 66.2%) had corneal oedema; however, the extent of the oedema varied. Sixteen eyes (21.6%) had corneal scarring. At the final follow-up visit, approximately one-quarter of the eyes (18, 24.3%) had clear corneas while the oedema persisted in another quarter of the eyes (19, 25.7%). Half of the eyes (37, 50.0%) continued to have corneal scarring. There was statistically significant clearing of corneal oedema (P=0.049). Figure 1 demonstrates the preoperative appearance of the week-old child with congenital glaucoma showing megalocornea and corneal oedema. Figure 2 demonstrates the 8-year postoperative appearance of the child in Figure 1.
Visual acuity
Preoperative visual acuity could be tested in only 19 patients (25.7%). Postoperatively, best-corrected visual acuity could be recorded for one-quarter of the patients (34, 25.7%). In the remaining patients (40, 74.3%), an ability to fix and follow light was recorded. Using various age-appropriate testing procedures, at the final follow-up visit, 14 patients (41.2%) had age-appropriate normal visual acuity and 20 patients (58.8%) had subnormal visual acuity. Visual acuity assessment using Snellen's chart was possible in 26 patients, (35.1%) and of these, a best-corrected visual acuity of ⩾20/60 was achieved in seven patients (26.9%).
Factors associated with poor visual outcome
Table 2 presents univariate comparisons of final surgical outcome according to several patient characteristics and the study groups were balanced at baseline in all the factors presented. In univariate analysis, the failure rate was higher in patients who presented with IOP >35 mmHg than those with IOP ⩽35 mmHg (46.2 vs 18.0%; HR=2.92). Patients who underwent prior glaucoma surgery had greater chances of failure with CTT as the second procedure (41.7 vs 19.4%; HR=2.17). However, in the multivariate analysis, only preoperative IOP >35 mmHg was a significant risk factor for failure for surgery with a Cox proportional HR of 2.92 (95% CI: 1.06–7.98, P=0.04) (Table 2). That is, the failure rate increased two- to three-fold in the presence of a preoperative IOP >35 mmHg.
Refractive errors
Data regarding refractive status were available for 41 (55.4%) patients. For the remaining patients, refraction was not possible due to media haze. Of the 41 patients, 33 (80.5%) were myopic with mean SE of 5.8±4.5D (range, 0.75–22.0D), two patients (4.9%) were hyperopic with mean SE of 3.6±1.9D (range, 2.25–5.0D), and six patients (14.6%) had SE of zero (emmetropic).
Success rate
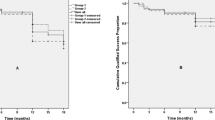
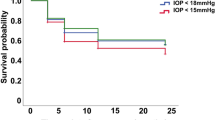
Complete success as defined in the present study was obtained in 51 eyes (68.9%). Kaplan–Meier survival analysis revealed 3-, 6-, 9-, 12-, 24-, 48-, and 72-month success rates of 86.5±4.0, 80.5±4.9, 78.1±5.4, 75.5±5.9, 71.1±6.9, and 60.5±11.1%, respectively, that was maintained for 8 years of follow-up (Figure 3). Qualified success was obtained in six eyes (8.1%), while 17 eyes (23.0%) were considered to be failures.
Surgical complications
There was no sight-threatening intraoperative complication. Of the minor postoperative complications, shallow anterior chamber occurred in eight (6.6%) eyes in the first postoperative week; however, surgical reformation was required in only four (3.3%) eyes. In the remainder (four eyes, 3.3%), the anterior chamber deepened spontaneously. Schlemm's canal could not be visualized and as a result, trabeculectomy alone was performed in five (4.1%) eyes. In another seven (5.9%) eyes, it was possible to rotate the trabeculotome on only one side of the radial incision. Rhegmatogenous retinal detachment that was too advanced for any surgical intervention occurred in five (4.1%) eyes. There was no incidence of bleb leakage, bleb-related infection or endophthalmitis.
Discussion
CTT is a promising new surgical technique for the treatment of developmental glaucoma.12, 15, 16, 17, 18 The classical operation for developmental glaucoma is goniotomy;27 however, the trend seems to be changing and there are increasing numbers of advocates of primary trabeculotomy.10, 28, 29, 30, 31, 32, 33 The reason underlying this change in trend is that trabeculotomy offers several major advantages over the alternative procedure of goniotomy as emphasized by Luntz.10 There have been several successful reports of primary trabeculotomy for developmental glaucoma.6, 7, 8, 9, 11, 28, 29, 30, 31, 32, 33 McPherson and Berry11 compared external trabeculotomy and goniotomy in a similar group of patients with developmental glaucoma. External trabeculotomy was statistically more successful as a first operation (19 of 23 eyes; 83%) than goniotomy (8 of 24 eyes; 33%; P=0.003).11 Furthermore, the prerequisite for successful goniotomy is a clear cornea to visualize the angle structures during the procedure.5, 10 In our series, only nine patients (12.2%) presented with clear corneas, in whom goniotomy would have been possible; the remaining patients (65, 87.8%) had corneal oedema and scarring. Despite the presence of a clear cornea, eyes with corneal diameter greater than 15 mm are not suitable for goniotomy, as reported by Barkan.13 The problems of goniotomy in children with hazy corneas, the advantages of trabeculotomy over goniotomy, coupled with encouraging reports of primary trabeculotomy in developmental glaucoma and the advanced nature of the disease process at birth or at presentation, prompted us to combine trabeculectomy ab externo with trabeculectomy during the initial surgery in our patient population.
Corneal enlargement is a poor prognostic factor in the management of the developmental glaucoma.34 It is generally accepted that the success of goniotomy is not as good in eyes with significant buphthalmos. In patients with significant increase in corneal diameter goniotomy is technically difficult to perform13 and CTT may be considered as the initial procedure. The aim of the present study was to evaluate the safety and efficacy of CTT in advanced developmental glaucoma with corneal diameter, greater than 14 mm. Kaplan–Meier survival analysis revealed 3-, 6-, 9-, 12-, 24-, 48-, and 72-month success rates of 86.5, 80.5, 78.1, 75.5, 71.1, and 60.5%, respectively, that was maintained for 8 years of follow-up. It is of interest that most of our patients (65, 87.8%) presented with severe corneal oedema or scarring associated with advanced megalocornea (mean corneal diameter, 14.6±0.8 mm). To our knowledge, there is no report in the literature where outcome of surgery on patients with advanced buphthalmos has been reported. Our success rate with initial surgery is significantly better than most of the reported results of initial goniotomy6, 7, 8 or trabeculotomy ab externo.9, 10, 11, 28, 29, 30, 31, 32, 33 The superior results of the combined procedure may be because of the dual outflow pathway as explained by Elder,35 and Mandal and co-workers3, 12, 14, 15, 16, 17, 18 The additional advantage of CTT is that it allows greater surgical flexibility in advanced buphthalmos. For example, conversion to trabeculectomy is feasible in cases where identification of Schlemm's canal is not possible. In our study, such a situation was encountered in five (4.1%) eyes. It was possible to rotate the trabeculotome on only one side of the radial incision in seven (5.9%) eyes. The addition of trabeculectomy is of significant advantage in such cases.
Whether primary CTT is superior to trabeculotomy or trabeculectomy alone is a subject of considerable debate. In a small series of seven Arab Bedouin infants, Biender and Rothkoff36 found no difference between trabeculotomy and CTT in patients with congenital glaucoma. Dietlein et al37 investigated the outcome of trabeculotomy, trabeculectomy, and a combined procedure as initial surgical treatment in primary congenital glaucoma. Although the combined procedure seems to have a favourable outcome, the advantages of this procedure over trabeculotomy or trabeculectomy were not statistically significant after 2 years. Elder35 compared primary trabeculectomy with CTT and found the latter to be superior. In the present study, all patients underwent CTT and our results are comparable to those reported by Elder35 and better than the results of goniotomy6, 7, 8 or trabeculotomy,9, 11, 28, 29, 30, 31, 32, 33 or trabeculectomy alone.38, 39, 40 Considering the significant corneal oedema or scarring, 360° trabeculotomy described by Beck and Lynch41 could have been considered as an alternative surgical technique that was reported to have an 87% success rate after one procedure. But the technique of performing a 360° trabeculotomy is highly demanding compared with trabeculotomy using metal probes. We do not have any experience in performing a 360° trabeculotomy, but excellent IOP control and an efficacy equal to that of multiple standard procedures make it an attractive choice amongst the available angle procedures. Filous and Brunova42 reported the results of modified trabeculotomy in the treatment of primary congenital glaucoma employing trabeculotomy probes more closely corresponding to the variable course of Schlemm's canal. They reported a success rate of 87% over a mean follow-up of 38.4±22.5 months and concluded that probing with the innovative instrument was easier and safer compared to standard trabeculotomy probes. We speculate that our success rate of trabeculotomy–trabeculectomy could be further enhanced with the use of a modified trabeculotomy probe.
Mullaney et al43 and Al-Hazmi et al44 used mitomycin-C (MMC) in primary CTT and reported a higher success rate. Our results are comparable to Mullaney et al43 but we do not believe in using MMC in primary surgery. However, MMC-augmented trabeculectomy may improve the outcome of repeat filtering surgery in refractory developmental glaucoma. Further prospective randomized studies are required to explore the surgical results of trabeculotomy, primary combined trabeculotomy and trabeculectomy, and 360° trabeculotomy. However, such a study is difficult to conduct because most glaucoma specialists are better trained in, and more comfortable with, one angle procedure than the other.
One of the aims of the study was to evaluate and analyse the functional outcome of advanced developmental glaucoma. Data regarding visual acuity was available for 34 patients (45.9%). Using various age-appropriate assessment procedures, normal visual acuity was observed in 14 patients (41.2%) and it was subnormal in 20 patients (58.8%). Of the 34 patients, visual acuity assessment using Snellen's chart was possible in approximately two-thirds of the patients (23, 67.6%); final best-corrected visual acuity of ⩾20/60 (⩾6/18) was achieved in approximately one-third (7, 30.4%) of the patients. Four patients (17.4%) had low vision and the remaining patients (12, 52.7%) were blind according to WHO categories of visual loss.22 However, given the advanced nature of the disease, the visual outcome of our series is encouraging.
Myopia was the most common refractive error found in the present study. It was found in 80.5% of the eyes of the study population. Previous studies have reported occurrence of myopia in children with developmental glaucoma.5, 6, 45 However, the incidence and severity of myopia is higher in the present series compared to our previously reported series on developmental glaucoma operated within 1 month17 and 6 months,18 respectively. We attribute the higher incidence of myopia in the present series to the severity of the disease.
There were no serious intraoperative complications. Of the minor postoperative complications, shallow anterior chamber occurred in eight (6.6%) eyes in the first postoperative week; however, surgical reformation was required in only four (3.3 %) eyes. In the remainder (four eyes, 3.3%), the anterior chamber deepened spontaneously. In the present study, approximately two-thirds (47, 63.5%) of the patients underwent simultaneous bilateral surgery to avoid another long anaesthesia despite the theoretical risk of endophthalmitis. There was no incidence of bleb leakage, bleb-related infection or endophthalmitis. Based on these results, we believe that simultaneous bilateral surgery can be undertaken safely in these patients. However, strict intraoperative asepsis is mandatory and the second eye should be operated as if performing a surgical procedure on a different patient.16
Children with advanced developmental glaucoma carry poor surgical prognosis and the frequency of failure is high.5 However, the chances of success are highest with the first surgical procedure.9, 46, 47 The present study confirms the reported observations; we expect that the outcome of our study will have a positive impact on parental counseeling.18, 48 The benefits of long-term IOP control and good visual outcome with a single surgery as achieved in the present study are attractive to both the parents and the treating ophthalmologist and a similar view has been expressed by Mendicino et al.48 However, the risk of long-term drift of the results must be borne in mind, as has been reported in the literature.36, 45, 49
The limitations of the present study are its nonrandomized, retrospective noncomparative design and the variability in the timing of the surgery depending on the clearance for anaesthesia and the unavailability of visual acuity data in 40 patients (54.0%).
In conclusion, primary CTT may be considered as an initial procedure in advanced cases of primary developmental glaucoma with a corneal diameter of 14 mm or more. These patients experienced good visual outcomes and IOP control with a low complication rate, with one-third achieving a visual acuity of 20/60 or better. Appropriate optical correction of the refractive error, coupled with aggressive amblyopia therapy instituted early, helped to improve the outcome.
References
Dandona L, Dandona R, Srinivas M, Giridhar P, Vilas K, Prasad MN et al. Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci 2001; 42: 908–916.
Agarwal HC, Sood NN, Kalra BR . Clinical presentation of congenital glaucoma. Indian J Ophthalmol 1983; 31: 619–622.
Mandal AK . Current concepts in the diagnosis and management of developmental glaucomas. Indian J Ophthalmol 1993; 41: 51–70.
Dandona L, Williams JD, Williams BC, Rao GN . Population-based assessment of childhood blindness in Southern India. Arch Ophthalmol 1998; 116: 545–546.
deLuise VP, Anderson DR . Primary infantile glaucoma (congenital glaucoma). Surv Ophthalmol 1983; 28: 1–19.
Shaffer RN . Prognosis of goniotomy in primary infantile glaucoma (trabeculodysgenesis). Trans Am Ophthalmol Soc 1982; 80: 321–325.
Hoskins Jr HD, Shaffer RN, Hetherington J . Goniotomy vs trabeculotomy. J Pediatr Ophthalmol Strabismus 1984; 21: 153–158.
Broughton WL, Parks MM . An analysis of treatment of congenital glaucoma by goniotomy. Am J Ophthalmol 1981; 91: 566–572.
McPherson Jr SD, McFarland D . External trabeculotomy for developmental glaucoma. Ophthalmology 1980; 87: 302–305.
Luntz MH . The advantages of trabeculotomy over goniotomy. J Pediatr Ophthalmol Strabismus 1984; 21: 150–153.
McPherson Jr SD, Berry DP . Goniotomy vs external trabeculotomy for developmental glaucoma. Am J Ophthalmol 1983; 95: 427–431.
Mandal AK, Naduvilath TJ, Jayagandhan A . Surgical results of combined trabeculotomy-trabeculectomy for developmental glaucoma. Ophthalmology 1998; 105: 974–982.
Barkan O . Goniotomy for the relief of congenital glaucoma. Br J Ophthalmol 1948; 32: 701–728.
Mandal AK . Microsurgical technique combines trabeculotomy and trabeculectomy to treat developmental glaucoma. Ocular Surg News, Internat Ed 1994; 5(8): 38–43.
Mandal AK . Primary combined trabeculotomy-trabeculectomy for early onset glaucoma in Sturge–Weber syndrome. Ophthalmology 1999; 78: 745–748.
Mandal AK, Bhatia PG, Gothwal VK, Reddy VM, Sriramulu P, Prasad MS et al. Safety and efficacy of simultaneous bilateral primary combined trabeculotomy–trabeculectomy for developmental glaucoma in India. Indian J Ophthalmol 2002; 50: 13–19.
Mandal AK, Gothwal VK, Bagga H, Nutheti R, Mansoori T . Outcome of surgery on infants younger than 1 month of age with congenital glaucoma. Ophthalmology 2003; 110: 1909–1915.
Mandal AK, Bhatia PG, Bhaskar A, Nutheti R . Long-term surgical and visual outcomes in Indian children with developmental glaucoma operated within 6 months of birth. Ophthalmology 2004; 111: 283–290.
Hoskins Jr HD, Shaffer RN, Hetherington J . Anatomical classification of the developmental glaucomas. Arch Ophthalmol 1984; 102: 1331–1336.
Bailey IL, Lovie-Kitchin JE . New design principles for visual acuity letter charts. Am J Optom Physiol Opt 1976; 53(11): 740–745.
Hatton DD . Model registry of early childhood visual impairment: first-year results. J Vis Imp Blindness 2001; 95(7): 418–433.
World Health Organization. The prevention of blindness—report of a study group. Technical Report Series, No. 518, WHO, Geneva, 1973.
Belkin M, Ticho U, Susal A, Levinson A . Ultrasonography in refraction of aphakic infants. Br J Ophthalmol 1973; 57: 845–848.
Gordon RA, Doniz BB . Refractive development of the human eye. Arch Ophthalmol 1985; 103: 785–789.
Newcombe RG, Duff GR . Eyes or patients ? Traps for the unwary in the statistical analysis of ophthalmological studies. Br J Ophthalmol 1987; 71: 645–646.
Cox DR . Regression models and life-tables (with discussion). J R Stat Assoc 1972; 34: 187–220.
Barkan O . Technique of goniotomy. Arch Ophthalmol 1938; 19: 217–223.
Harms H, Danheim R . Trabeculotomy—results and problems. Adv Ophthalmol 1965; 22: 121–131.
Harms H, Danheim R . Epicritical consideration of 300 cases of trabeculotomy ‘ab externo’. Trans Ophthalmol Soc UK 1970; 89: 491–499.
McPherson Jr SD . Results of external trabeculotomy. Am J Ophthalmol 1973; 76: 18–20.
Quigley HA . Childhood glaucoma: results with trabeculotomy and study of reversible cupping. Ophthalmology 1982; 89: 219–226.
Akimoto M, Tanihara H, Negi A, Nagata . Surgical results of trabeculotomy ab externo for developmental glaucoma. Arch Ophthalmol 1994; 112: 1540–1544.
Luntz MH . Primary buphthalmos (infantile glaucoma). Treated by trabeculotomy ab externo. S Afr Arch Ophthalmol 1974; 2: 319–333.
Gregerson E, Kessing SVV . Congenital glaucoma before and after the introduction of microscopy. Results of ‘macrosurgery’ 1943–1963 and of ‘microsurgery’ (trabeculotomy/ectomy) 1970–1974. Acta Ophthalmologica 1977; 55: 422–430.
Elder MJ . Combined trabeculotomy–trabeculectomy compared with primary trabeculectomy for congenital glaucoma. Br J Ophthalmol 1994; 78: 745–748.
Biedner BZ, Rothkoff L . Combined trabeculotomy–trabeculectomy compared with primary trabeculotomy for congenital glaucoma. J Pediatr Ophthalmol Strabismus 1998; 35: 49–50.
Dietlein TS, Jacob PC, Krieglstein GK . Prognosis of primary ab externo surgery for primary congenital glaucoma. Br J Ophthalmol 1999; 83: 317–322.
Debnath SC, Teichmann KD, Salamah K . Trabeculectomy versus trabeculotomy in congenital glaucoma. Br J Ophthalmol 1989; 73: 608–611.
Rao CV, Sai CM, Babu BVN . Trrabeculectomy in congenital glaucoma. Indian J Ophthalmol 1984; 32: 439–440.
Burke JP, Bowell R . Primary trabeculectomy combined with beta radiation for congenital glaucoma. Br J Ophthalmol 1991; 75: 584–590.
Beck AD, Lynch MG . 360° trabeculotomy for primary congenital glaucoma. Arch Ophthalmol 1995; 113: 1200–1202.
Filous A, Brunova B . Results of the modified trabeculotomy in the treatment of primary congenital glaucoma. J AAPOS 2002; 6: 182–186.
Mullaney PB, Selleck, Al-Awad A, Al-Mesfer S, Zwaan J . Combined trabeculotomy and trabeculectomy as initial procedure in uncomplicated congenital glaucoma. Arch Ophthalmol 1999; 117: 457–460.
Al-Hazmi A, Zwaan J, Awad A, Al-Mesfer S, Mullaney PB, Wheeler DT et al. Effectiveness and complications of mitomycin- C use during pediatric glaucoma surgery. Ophthalmology 1998; 105: 1915–1920.
Rice NSC . The surgical management of the congenital glaucomas. Auts J Ophthalmol 1977; 5: 174–179.
Haas J . Principles and problems of therapy in congenital glaucoma. Invest Ophthalmol 1968; 7: 140–146.
O' Connor G . Combined trabeculotomy-trabeculectomy for congenital glaucoma. Br J Ophthalmol 1994; 78: 735.
Mendicino ME, Lynch MG, Drack A, Beck AD, Harbin T, Pollard Z et al. Long-term surgical and visual outcomes in primary congenital glaucoma: 360° trabeculotomy versus goniotomy. J AAPOS 2000; 4: 205–210.
Russell-Eggitt IM, Rice NS, Jay B, Wyse RK . Relapse following goniotomy for congenital glaucoma due to trabecular dysgenesis. Eye 1992; 6: 197–200.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a poster at the annual meeting of the American Academy of Ophthalmology, Anaheim, California, November 15–18, 2003.
Supported in part by the Hyderabad Eye Research Foundation, L V Prasad Eye Institute, Hyderabad, India.
The authors have no proprietary interest in any of the materials or techniques used in this study.
Rights and permissions
About this article
Cite this article
Mandal, A., Matalia, J., Nutheti, R. et al. Combined trabeculotomy and trabeculectomy in advanced primary developmental glaucoma with corneal diameter of 14 mm or more. Eye 20, 135–143 (2006). https://doi.org/10.1038/sj.eye.6701817
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701817
Keywords
This article is cited by
-
Combined trabeculotomy–trabeculectomy with and without augmentation in primary congenital glaucoma: triple-armed randomized controlled trial
International Ophthalmology (2022)
-
Combined trabeculotomy-trabeculectomy using the modified Safer Surgery System augmented with MMC: its long-term outcomes of glaucoma treatment in Asian children
Graefe's Archive for Clinical and Experimental Ophthalmology (2018)
-
Long-term surgical outcome of conventional trabeculotomy for childhood glaucoma
Japanese Journal of Ophthalmology (2017)
-
Early-onset glaucoma in Axenfeld–Rieger anomaly: long-term surgical results and visual outcome
Eye (2016)
-
Combined trabeculotomy and trabeculectomy: outcome for primary congenital glaucoma in a West African population
Eye (2011)