Abstract
Purpose
To study the results of intravitreal tissue plasminogen activator (tPA) and expansile gas injection for submacular haemorrhage in Thai patients.
Methods
The medical records of Thai patients who presented with submacular haemorrhage between January 1998 and December 2002 were reviewed. The inclusion criteria were acute onset of bleeding (<1 month), treatment with intravitreal injection of tPA solution (50–100 μg in 0.1 ml) and expansile gas (0.3–0.4 ml of 100% perfluoropropane or sulphur hexafluoride), and at least 6 months of follow-up. Our main outcome measures were best final postoperative visual acuity and surgical complications.
Results
A total of 19 eyes of 19 patients completed the inclusion criteria with a mean duration of 13.1 days. The causes of haemorrhage were age-related macular degeneration in 15 eyes (78.9%), idiopathic choroidal neovascularization in two eyes (10.5%), and traumatic, and valsalva retinopathy in one eye each (5.2%). After a mean follow-up of 13 months (range 6–39 months), postoperative visual acuity improved two lines or greater in 12 eyes (63.2%), stabilized in six eyes (31.6%) and worsened in one (5.2%). The final visual acuity measured 20/63 or better in 10 eyes (52.6%). The surgical complications were breakthrough vitreous haemorrhage (three eyes) and cataracts (three eyes), and two had retinal detachments.
Conclusion
The treatment of submacular haemorrhage with intravitreal injection of tPA and expansile gas improved visual acuity in more than half of the patients. In all, 10 in 19 eyes demonstrated final visual acuity at a functional level.
Similar content being viewed by others
Introduction
Submacular haemorrhage is a bleeding condition between the neurosensory retina and the retinal pigment epithelium layer surrounding the foveolar area. Without appropriate treatment, severe toxicity to photoreceptors and the outer retinal layer probably causes irreversible visual loss. Bennett et al1 found a mean visual acuity of 20/1700 in 12 age-related macular degeneration (ARMD) patients with submacular haemorrhage after 3 years of follow-up. In another series, Avery et al2 found that at 36 months, a mean of 3.5 lines of visual acuity had been lost in 16 out of 41 eyes and 44% of eyes had lost 6 or more lines of visual acuity. They also found that 21% of patients showed a spontaneous improvement of 3 or more lines at the end of the study. Berrocal et al3 found that only 30% of patients had a final visual acuity of 20/80 or better. Therefore, it is suggested that prolonged toxicity of blood products to photoreceptors in submacular haemorrhage could lead to severe and permanent visual deficit.4, 5, 6
There are several aetiologies of submacular haemorrhage associated with or without choroidal neovascularization. Among these conditions, ARMD is the most common cause worldwide of submacular haemorrhage in the elderly with permanent visual loss. A number of treatments have been carried out to remove the haematoma from the foveolar area urgently. These include vitrectomy and manual clot extraction, vitrectomy and adjunctive tissue plasminogen activator (tPA), or intravitreal injection of tPA and expansile gas.7, 8, 9, 10 Each technique has various outcomes and there are no reliable comparative studies. Nevertheless, the intravitreal injection of tPA and expansile gas is an easy, simple procedure that can be performed in an outpatient unit. This technique has become a popular alternative.
The intravitreal injection of tPA and expansile gas for submacular haemorrhage has been used in our hospital since 1998. The purpose of this study was to evaluate the results and complications of the treatment in order to provide accurate data for our patients about the possible outcomes, especially in the Asian races.
Methods
The medical records of 24 consecutive patients with submacular haemorrhage in Songklanagarind Hospital (Songkhla Province, Thailand) between January 1998 and December 2002 were reviewed retrospectively. The inclusion criteria were (1) acute onset of bleeding within 1 month, (2) treatment with intravitreal injection of tPA 50–100 μg/0.1 ml with expansile gas (100% perfluoropropane 0.3 ml or 100% sulphur hexafluoride 0.4 ml), and (3) a follow-up period of at least 6 months.
The examinations were performed by two retinal specialists, including a complete eye examination, visual acuity using ETDRS chart, applanation tonometry, and fundus examination with indirect ophthalmoscope or fundus contact lens. The clinical appearances of soft drusen and retinal pigmentary changes in either eye or the presence of subretinal fluid and exudate associated with drusen and pigmentary changes in patients over 50 years of age suggested the diagnosis of ARMD.
The patients were explained about the treatments and informed consents were signed. The procedures were performed in an operating room under topical anaesthesia using sterile techniques. After paracentesis, 50–100 μg/0.1 ml of tPA in a balanced salt solution (BSS) was injected into the midvitreous cavity by a 30-gauze needle at pars plana superotemporally. As a result of the retrospective design, the decision for doses of tPA injection and types of expansile gas was dependent on surgeons' preferences (two retinal specialists). All patients were admitted to the hospital to remain in a proper prone position for at least 24 h.
The patients were examined on the first following day, one week and then monthly for a period of at least 6 months. Our outcome measures were (1) the patient demographic data and (2) the initial and final visual acuity by ETDRS chart. The visual acuity improvement was defined as at least 2 lines improvement from the preoperative level, (3) pre-, postoperative, and final fundus findings, (4) the doses of tPA and number of injections, (5) the postoperative fluorescein angiographic study within a few weeks, if necessary, and (6) complications and adjunctive procedures.
Results
In all, 19 of 24 eyes (79.1%) completed the inclusion criteria. The other five eyes had less than 6 months follow-up and were excluded from the study. The demographic data and results are shown in Table 1. Mean age and duration of haemorrhage were 56.3 years (range 22–80 years) and 13.1 days (range 1–20 days), respectively. The aetiologies were defined as age-related macular degeneration in 15 eyes (78.9%), idiopathic choroidal neovascularization in two eyes (10.5%), and traumatic and valsalva retinopathy in one eye each (5.2%).
The size of the haematoma was more than 3 disc diameters in 15 eyes (78.9%), 2–3 disc diameters in two eyes and less than 2 disc diameters in the other two eyes. This result showed that most cases had severe bleeding and were assumed to have poor prognosis without any intervention. Most were injected with 100 μg of tPA (16 of 19 eyes) and 63% (12 in 19 eyes) used sulphur hexafluoride gas for a tamponade effect. There is no difference in the results or complications between the two expansile gases.
By clinical observation, the treatment resulted in displacement of the haematoma from the fovea within 1 week in most of our cases. Only one patient received reinjection due to rebleeding within a month. This patient showed a good visual restoration after 8 months (case No. 18 from Table 1) and developed retinal pigmentary changes and a scar outside the foveolar area.
After a mean follow-up time of 13 months (range 6–39 months), the final visual acuity improved 2 lines or greater in 12 eyes (63.2%), and 3 lines or greater in 10 eyes (52.6%). Totally, the level of visual acuity was improved (better than the preoperative level at least 2 lines) or unchanged (the same as the preoperative level) in 18 eyes (94.7%) and measured 20/63 or better in 10 eyes (52.6%). A severe subfoveal disciform scar was found in one patient who had final visual acuity below the preoperative level (case No. 5 from Table 1). Two eyes with detachments experienced poor surgical results but still had the visual acuity of hand motion, unchanged from the preoperative level.
Fluorescein angiography was performed in 10 eyes at a mean time of 12.7 weeks (3–32 weeks) after the injections. It revealed active choroidal neovascularization in seven eyes (three for occult subfoveal types, two for occult juxtafovea, and two for occult extrafoveal lesions), leading to four eyes having further treatment with laser photocoagulation and one with photodynamic therapy. In the other eyes of ARMD and idiopathic causes, the angiography or fundus examinations demonstrated subfoveal disciform scars without active vessels in five eyes, while another five eyes showed juxta or extrafoveal disciform scars and did not require any laser treatment. These findings indicated that more than half of ARMD and idiopathic cases in this study had a bleeding site outside the foveolar area (nine in 17 eyes, 52.9%).
Among the complications, breakthrough vitreous haemorrhage and cataracts were the most common, with an incidence of 15.7% each (three of 19 eyes). One patient with vitreous haemorrhage underwent vitrectomy while the others showed spontaneous clearing of the blood. Two eyes with detachments also had multiple vitrectomies and experienced unfavourable outcomes.
Discussion
Submacular haemorrhage is associated with or without choroidal neovascularization. Among these diseases, ARMD is the most common aetiology of irreversible macular damage caused by submacular haematoma. Experimental studies in animals4, 5, 6 have found that the blood components cause severe and irreversible damage to the retina within 24 h. In humans, several studies demonstrated poor visual prognosis in most cases. Therefore, many techniques to remove the blood from a foveolar area have been described. Lewis7 reported a pilot study of tPA and surgical drainage in 24 eyes. In all, 83% of cases had notable improvement and 33% attained visual acuity of 20/200 or better. Lim et al8 reviewed 18 cases with subretinal injection of tPA during pars plana vitrectomy to evacuate dense subretinal haemorrhage. The visual acuity improved by 2 or more lines in 61% of eyes and did not change in 22%. It was concluded that the visual improvement was limited by underlying diseases. In contrast, Ibanez et al9 reported poor visual prognosis whether or not the surgical drainage was performed and found that tPA did not appear to significantly improve the outcome. Nevertheless, to date, one of the most widely used techniques is intravitreal injection of tPA and expansile gas to displace the blood from a fovea. Heriot described this technique as a high-success procedure (Heriot WJ, presented at the AAO Annual Vitreoretinal Update, San Francisco, October 1997) and Hassan et al10 reported 67% of 2 lines or greater improvement of visual acuity in 15 patients. This technique has been used worldwide but few data have been reported in Asian patients.
tPA is the fibrinolytic agent that activates plasminogen to become plasmin and fibrin breakdown products. Johnson et al11 reported retinal toxicity in rabbit eyes with intravitreous injection of 50 μg/0.1 ml or greater. For human eyes, however, Hassan et al10 found no evidence of retinal or other intraocular toxic reactions to tPA solution in doses of 25–100 μg in 0.1 ml. In this study, tPA at 50–100 μg in 0.1 ml solution followed by one of the two expansile gases (0.3 ml of 100% perfluoropropane or 0.4 ml of 100% sulphur hexafluoride) was used, with no clinical retinal toxicity found in any case.
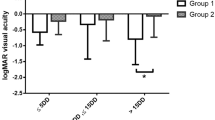
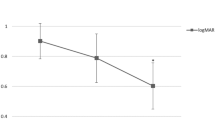
In this study, 63.2% (12 of 19 eyes) had visual acuity improvement of 2 or more lines and 52.6% (10 in 19 eyes) had 3 lines or greater (Figure 1). By the last follow-up of the average of 13 months, 52.6% showed visual acuity of 20/63 or better and one eye (5.2%) deteriorated. Considering the fluorescein or fundus findings, the disciform scars were found outside a foveolar area in 52.9% of ARMD and idiopathic cases (nine in 17 eyes). Seven eyes showed active neovascularization, four of these were extrafoveal or juxtafoveal lesions and treatable with argon laser photocoagulation. Although ARMD were the majority in this study, more than half of the lesions demonstrated a bleeding site outside the foveolar area, which accounted for the good visual results.
This study in Asian patients has confirmed the results of the previous studies.10, 12, 13, 14 Our results were comparable to Hassan et al10 for final visual improvement by 2 lines or greater in 67% (10 of 15 eyes) with a few complications such as breakthrough vitreous haemorrhage, with similar aetiologies of ARMD and disciform scar afterwards. However, Yannuzzi et al15 showed a specific type of choroidopathy in some black and Asian patients, such as an idiopathic polypoidal choroidal vasculopathy (IPCV). This condition usually had a different prognosis from ARMD, and resulted in a favourable outcome in about 50% of patients.16 We believe that some of our cases might have been an IPCV, which accounted for the good visual results after turning out to be scars that spared a fovea. Unfortunately, an indocyanine green angiography machine was not available to confirm the diagnosis; therefore, all the angiographic diagnosis was based on the fluorescein findings alone. Nevertheless, due to difficulty labelling the definite diagnosis when the patients presented to us, all patients should be provided a chance of visual recovery by being treated as soon as possible.
Our study also reviewed the dimension of the haematoma. In all, 15 eyes (78.9%) had more than 3-disc diameter size but most of them made a recovery to some extent. However, the effect of haematoma size was not included in the analysis due to a rough estimate in some cases. We believe that the location of neovascularization influenced the visual outcome in this study rather than the amount of bleeding.
Breakthrough vitreous haemorrhage and cataracts were the most common complications in the study (three eyes each, 15.7%), followed by retinal detachments. Only one eye with vitreous haemorrhage needed pars plana vitrectomy to remove the blood with subsequent good visual recovery. Two eyes with detachments did not have visual recovery because of severe conditions but still had the same level of visual acuity. However, the rate of complications was considered small and acceptable.
This study is a good example for developing countries that do not have sophisticated equipment for ocular investigations. The results showed that even though there is no indocyanine green angiography machine to facilitate identification of the exact causes of haemorrhage at the presenting day, we could still treat the patients with acute submacular haemorrhage and provide acceptable visual results. An urgent treatment is a crucial factor for visual recovery especially in our Asian patients at the age between 50 and 60 years who are assumed to be IPCV rather than ARMD.
In conclusion, in this study of Asian patients, the treatment of submacular haemorrhage using intravitreal injection of tPA and expansile gas revealed favourable results and a low rate of complications. As the definite cause of bleeding cannot be determined in the beginning, every patient should be treated immediately for a better chance of visual improvement and further definite treatments.
References
Bennett SR, Folk JC, Blodi CF, Klugman M . Factors prognostic of visual outcome in patients with subretinal hemorrhage. Am J Ophthalmol 1990; 109: 33–37.
Avery RL, Fekrat S, Hawkins BS, Bressler NM . Natural history of subfoveal subretinal hemorrhage in age-related macular degeneration. Retina 1996; 16: 183–189.
Berrocal MH, Lewis ML, Flynn Jr HW . Variations in the clinical course of submacular hemorrhage. Am J Ophthalmol 1996; 122: 486–493.
Glatt H, Machemer R . Experimental subretinal hemorrhage in rabbits. Am J Ophthalmol 1982; 94: 762–773.
Lewis H, Resnick SC, Flannery JG, Straatsma BR . Tissue plasminogen activator treatment of experimental subretinal hemorrhage. Am J Ophthalmol 1991; 111: 197–204.
Toth CA, Morse LS, Hjelmeland LM, Landers III MB . Fibrin directs early retinal damage after experimental subretinal hemorrhage. Arch Ophthalmol 1991; 109: 723–729.
Lewis H . Intraoperative fibrinolysis of submacular hemorrhage with tissue plasminogen activator and surgical drainage. Am J Ophthalmol 1994; 118: 559–568.
Lim JI, Drews-Botsch C, Sternberg Jr P, Capone Jr A, Aaberg TM . Submacular hemorrhage removal. Ophthalmology 1995; 102: 1393–1399.
Ibanez HE, Williams DF, Thomas MA, Ruby AJ, Meredith TA, Boniuk I et al. Surgical management of submacular hemorrhage. A series of 47 consecutive cases. Arch Ophthalmol 1995; 113: 62–69.
Hassan AS, Johnson MW, Schneiderman TE, Regillo CD, Tornambe PE, Poliner LS et al. Management of submacular hemorrhage with intravitreous tissue plasminogen activator injection and pneumatic displacement. Ophthalmology 1999; 106: 1900–1907.
Johnson MW, Olsen KR, Hernandez E, Irvine WD, Johnson RN . Retinal toxicity of recombinant tissue plasminogen activator in the rabbit. Arch Ophthalmol 1990; 108: 259–263.
Meier P, Zeumer C, Jochmann C, Wiedemann P . Management of submacular hemorrhage by tissue plasminogen activator and SF6 gas injection. Ophthalmologe 1999; 96: 643–647.
Buhl M, Scheider A, Schonfeld CL, Kampik A . Intra-vitreal rt-PA and gas introduction in submacular hemorrhage. Ophthalmologe 1999; 96: 792–796.
Krepler K, Kruger A, Tittl M, Stur M, Wedrich A . Intravitreal injection of tissue plasminogen activator and gas in subretinal hemorrhage caused by age-related macular degeneration. Retina 2000; 20: 251–256.
Yannuzzi LA, Sorenson J, Spaide RF, Lipson B . Idiopathic polypoidal choroidal vasculopathy. Retina 1990; 10: 1–8.
Uyama M, Wada M, Nagai Y, Matsubara T, Matsunaga H, Fukushima I et al. Polypoidal choroidal vasculopathy: natural history. Am J Ophthalmol 2002; 133: 639–648.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ratanasukon, M., Kittantong, A. Results of intravitreal tissue plasminogen activator and expansile gas injection for submacular haemorrhage in Thais. Eye 19, 1328–1332 (2005). https://doi.org/10.1038/sj.eye.6701769
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701769
Keywords
This article is cited by
-
Submakuläre Blutung bei AMD
Spektrum der Augenheilkunde (2009)