Abstract
Purpose To investigate the influence of ionizing radiation on the corneal epithelium and endothelium of rabbit eyes.
Methods Five healthy mature albino rabbits were unilaterally irradiated with 20 Gy of X-rays (250 kV, 12 mA). Slit-lamp biomicroscopic observation and specular microscopic examination of the corneal epithelium and endothelium were carried out before and 1, 4, 8, 12, 16, 20, 24, and 36 weeks after irradiation. We evaluated mean area of the superficial corneal epithelial cells, mean area and the percentage of hexagonal cells of the corneal endothelial cells, and corneal thickness. The statistical difference between the irradiated and control eyes was assessed using paired t-test.
Results All animals developed cataract within 24 weeks. Slit-lamp biomicroscopy showed no apparent corneal abnormalities over the 36-week follow-up period. Specular microscopy revealed a significant enlargement of the superficial corneal epithelial cells from 4 to 12 weeks after irradiation (P<0.01), which disappeared at 16 weeks post-irradiation. Specular microscopy of the corneal endothelium showed enlargement and morphological alterations of the cells beginning 8 weeks after irradiation (P<0.05). These changes persisted throughout the study period. There were no statistically significant changes in corneal thickness.
Conclusion After X-ray radiation of 20 Gy, transient damage occurred in the corneal epithelium, while delayed and irreversible changes were seen in the endothelium.
Similar content being viewed by others
Introduction
The influence of ionizing radiation on the eye has been studied for a long time.1, 2, 3, 4, 5, 6, 7, 8 Cataract is one of the most common complications of radiotherapy,4 and many clinical and experimental studies are available on radiation-induced cataract.5, 6, 7, 8 Optic neuropathy9 and chorioretinopathy10 related to radiation exposure have also been studied clinically. Keratopathy is another form of complication associated with ionizing radiation. Merriam et al11 reported that a dose of 6000 rad within 5–6 weeks caused corneal ulceration in three of 25 patients treated for orbital tumours. In two patients, the cornea perforated and the eye was enucleated 4–12 months after the completion of radiation therapy. Despite these clinical reports, there has been a paucity of basic research on the influence of ionizing radiation on the cornea. Most of the previous studies evaluated the corneal epithelium because of its high sensitivity to ionizing radiation.12, 13, 14, 15 Moreover, histopathological techniques were mainly used in those studies.
The specular microscope is a useful tool in analysing corneal endothelial and epithelial cells. It has been used to evaluate the cornea following refractive surgery16, 17 and ultraviolet irradiation.18 There has been no specular microscopic study, however, on the corneal morphological changes after ionizing radiation, and thus the time course of changes in the corneal epithelium and endothelium after irradiation remains unknown. The current study was aimed at investigating the long-term influence of moderate ionizing radiation on the corneal epithelial and endothelial cells.
Materials and methods
Animals and radiation exposure
Five healthy mature albino rabbits (2.5–3.0 kg) were used. The animals were used in accordance with the guidelines laid down by the ARVO statement for the Use of the Animals in Ophthalmic and Vision Research. Rabbits were anaesthetized with an intravenous injection of 1.5 g/kg urethane. The deep therapy X-ray was used for the source of ionizing radiation. The X-ray unit was operated at 200 kVp, 12 mA. After the eyelid of a rabbit was forced open by a lid retractor, one eye of each rabbit received a single dose of 20 Gy. The X-ray beam was collimated to a diameter of 15 × 20 mm through a lead collimator of 5.0 mm thickness, so as to prevent exposure of the tissue around the eye ball (Figure 1). The entire cornea including the limbus was irradiated. The contralateral eye served as a control. The rabbits were euthanized by pentobarbital sodium overdose after the study.
Examinations
The cornea was observed with a portable slit-lamp microscope with fluorescein staining. Examinations using a wide-field specular microscope (Keeler-Konan, Tokyo) were conducted before and 1, 4, 8, 12, 16, 20, 24, and 36 weeks afterwards. A drop of sodium hyaluronate was instilled on the cone of the microscope to obtain clear observations of the epithelial and endothelial cells. Specular microscopy was performed on the central cornea. Corneal thickness was also measured with the pachymeter (Keeler-Konan, Tokyo) attached to the specular microscope. Photographs of the epithelium and endothelium taken with the specular microscope were enlarged by 40 times and quantitatively analysed with a computerized cell analysis system. Cell shape was determined by digitizing the apex of each cell. A total of 40 epithelial cells were examined per eye, and the mean area of the superficial corneal epithelial cells was calculated. A total of 100 endothelial cells were examined per eye. We evaluated two parameters: mean cell area and the percentage of hexagonal cells.
Statistical analysis
Data are reported as mean±SD. Values were compared between the irradiated and the control eyes. The significance of changes was assessed with paired t-test. Differences were considered statistically significant at P<0.05.
Results
Slit-lamp biomicroscopy
Slight, transient erythema of the eyelid margin with conjunctival injection was noted in all animals 1 week following irradiation. Two of five animals exhibited cataract within 20 weeks after irradiation, and the remaining three animals developed cataract within 24 weeks. No treatment was performed on these cataracts. On slit-lamp microscopic examination, there were no apparent abnormalities in the cornea and the anterior chamber. Any signs of limbal deficiency such as pannus formation were not observed during the study.
Specular microscopy
The mean area of the superficial corneal epithelial cells before the irradiation was 468±19 μm2 (Figure 2a). The time course of change in the mean cell area after irradiation is shown in Figure 3. Enlargement of the epithelial cells was found at 4 weeks post-treatment (Figure 2b). The mean cell area in the treated group was significantly larger than that in the control group from 4 to 12 weeks after procedure (P<0.01). At 16 weeks and thereafter, there were no abnormal findings in the epithelium (Figure 2c).
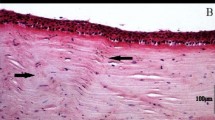
The changes in endothelial cells following irradiation were analyzed in terms of the mean cell area and percentage of hexagonal cells. The irradiation significantly increased the mean cell area (Figure 4a) and decreased the percentage of hexagonal cells (Figure 4b). There was no significant intergroup difference 4 weeks after treatment, but values at 8 weeks and thereafter in the treatment group were significantly different from those in the control group (P<0.05). After irradiation, several giant cells were seen in the endothelium (Figure 5).
There were no statistically significant changes in corneal thickness throughout the follow-up period of this study (Figure 6).
Discussion
The single dose of X-ray or gamma-ray that caused slight corneal injury has been reported to be 500–2700 rad (5–27 Gy) in experimental sutudies.12, 13, 14 Serious injury such as corneal ulcer was produced by doses over 2000 rad (20 Gy).13, 14, 15 In the present attempt to elucidate the effect of moderate ionizing radiation on the cornea, we selected a dose of 20 Gy in order to avoid serious corneal damages. In the current study, slit-lamp microscopic examinations revealed no abnormal findings in the rabbit cornea irradiated with 20 Gy of X-rays. Owing to the relatively low dose of X-irradiation administered and the usage of a lead collimator (Figure 1), damage of the lacrimal gland seemed minimal. We thought this was important because alterations in the tear secretion might have modified the physiological status of corneal structure.
Although specular microscopic analysis is an established technique in evaluating the corneal endothelium, it has not been widely used to assess the corneal epithelium. Tsubota et al19 reported that evaluation of the mean cell area is useful for detecting subtle changes in the superficial corneal epithelium. Enlargement of epithelial cells was demonstrated in diabetic aphakic patients, extended soft contact lens wearers, and aphakic patients who used 0.5% indomethacin eye drops.20 Such conditions may influence the metabolism of epithelial cells, resulting in alteration of differentiation and mitosis of epithelial cells. In contrast, small epithelial cells were commonly observed in patients with dry eye.21
The mechanism of the cell injury caused by ionizing radiation has not been fully elucidated. Both lethal and sublethal damages can occur in the cells,22 and sublethal damages are repairable.23 A delay in cell division and a suppression of mitosis have been confirmed in the basal cells of the corneal epithelium after sublethal damages.24 Specular microscopic examination in the present study revealed significant increases in the mean cell area of the superficial corneal epithelium from 4 weeks after irradiation, but changes were transient. At 16 weeks and thereafter, there were no abnormal findings in the epithelium. These results indicate that the corneal epithelial injury observed herein represent sublethal damage of the basal cells in corneal epithelium. In addition, because any signs of limbal deficiency were not observed during the study, we considered that stem cell damage of the cornea was minimal under the condition of X-irradiation used in this experiment. The sensitivity of tissues to irradiation depends on the turnover rate of the cells.25 The corneal epithelial cells possess very high division potential.26, 27 It is not surprising that corneal epithelium showed early response to X-irradiation, and changes were practically reversible. The recovery of corneal epithelium is expected unless stem cells are damaged completely.28
The current study represents the first in vivo, longitudinal investigation on the corneal endothelial injury after X-ray irradiation. The results showed that there were no significant morphological changes in the endothelium immediately after irradiation, presumably due to the low turnover rate of corneal endothelial cells. The turnover rate of vascular endothelial cells is similarly low,29 and it has been reported that these cells also show delayed responses to X-ray irradiation.30 Calvo et al30 reported that the structural abnormality involving damaged nucleus and loss of endothelial cells in the choroid plexus of rat brain developed 12 weeks after a single dose of X-ray irradiation. In the current study, increases in the mean cell area and decreases in the percentage of hexagonal cells were observed at 8 weeks post-treatment. These endothelial changes persisted, or even progressed throughout the 36-week study period. De Gowin et al31 reported that X-irradiation inhibited mitosis of human vascular endothelial cells in culture. Yao demonstrated that X-ray induced destruction of chromosome in the cultured corneal endothelial cell of rat kangaroo.32 It seems that X-ray exposure in the present study inhibited cell division and/or mitosis of rabbit endothelium, leading to progressive and irreversible changes in the endothelial cellular morphology. On the other hand, corneal thickness remained unchanged throughout the experiment, suggesting that the corneal endothelial function in the irradiated eyes was maintained during the current observation period. In comparison to humans, rabbits hold greater healing potential of the corneal endothelium, including migration, elongation, and proliferation of the adjacent cells.33 Therefore, functional capacity after endothelial trauma can be much larger in rabbits, and thus the results obtained herein may not directly apply to human eyes. Moreover, the primary anatomical event after ionizing radiation was reported to be endothelial cell damage, followed by alterations of the surrounding tissues in the retina and optic nerve.34, 35, 36 Further studies will be needed to discuss the long-term structural integrity of the cornea after ionizing radiation.
References
Upton AC, Christenberry KW, Melville GS, Furth J, Hurst GS . The relative biological effectiveness of neutrons, X-rays, and gamma rays for the production of lens opacities: observations on mice, rats, guinea-pigs, and rabbits. Radiology 1956; 67: 686–696.
Geeraets WJ, Ham WT, Mueller HA, Williams RC, Cleary SF . Effects of acute and protracted ionizing radiation on the rabbit lens. Acta Ophthalmol 1971; 49: 817–855.
Lipman RM, Tripathi BJ, Tripathi RC . Cataracts induced by microwave and ionizing radiation. Surv Ophthalmol 1988; 33: 200–210.
Cogan DG, Donaldson DD, Reese AB . Clinical and pathological characteristics of radiation cataract. Arch Ophthalmol 1952; 47: 55–70.
Focht EF, Merriam GR, Schwartz MS, Velasquez J, McNeill D . A method for radiation cataract analysis and its uses in experimental fractionation studies. Radiology 1966; 87: 465–474.
Merriam GR, Focht EF . A clinical study of radiation cataracts and the relationship to dose. Am J Roentgenol 1957; 77: 759–785.
Ramsell TG, Berry RJ . Recovery from X-ray damage to the lens. Br J Radiol 1966; 39: 853–858.
Cogan DG, Dreissler KK . Minimal amount of X-ray exposure causing lens opacities in the human eye. Arch Ophthalmol 1953; 50: 30–34.
Kline LB, Kim JY, Ceballos R . Radiation optic neuropathy. Ophthalmology 1985; 92: 1118–1126.
Brown GC, Shields JA, Sanborn G, Augsburger JJ, Savino PJ, Schatz NJ . Radiation retinopathy. Ophthalmology 1982; 89: 1494–1501.
Merriam GR, Szechter A, Focht EF . The effects of ionizing radiation on the eye. In: Vaeth JM (eds). Frontiers of Radiation Therapy and Oncology, Vol. 6. Karger, Basel and University Park Press: Baltimore, 1972; pp 346–385.
Scheie HG, Dennis RH, Ripple RC, Calkinis LL, Buesseler JA . The effect of low-voltage roentgen rays on the normal and vascularized cornea of the rabbit. Am J Ophthalmol 1950; 33: 549–571.
Cogan DG, Donaldson DD . Experimental radiation cataracts. Arch Ophthalmol 1951; 45: 508–522.
Biegel AC . Experimental ocular effects of high-voltage radiation from betatron. Arch Ophthalmol 1955; 54: 392–406.
Blodi FC . The effects of experimental X-radiation on the cornea. Arch Ophthalmol 1960; 63: 20–29.
Perez-Santonja JJ, Sakla HF, Gobbi F, Alio JL . Corneal endothelial changes after laser in situ keratomileusis. J Cataract Refract Surg 1997; 23: 177–183.
Amano S, Shimizu K, Tsubota K . Specular microscopic evaluation of the corneal epithelium after excimer laser photorefractive keratectomy. Am J Ophthalmol 1994; 117: 381–384.
Ringvold A, Davenger M, Olsen EG . Changes of the cornea endothelium after ultraviolet radiation. Acta Ophthalmol 1982; 60: 41–53.
Tsubota K, Yamada M, Naoi S . Specular microscopic observation of normal human corneal epithelium. Ophthalmology 1991; 99: 89–94.
Tsubota K, Yamada M, Naoi S . Specular microscopic observation of human corneal epithelial abnormalities. Ophthalmology 1990; 98: 184–191.
Lemp MA, Gold JB, Wong S, Mahmood M, Guimaraes R . An in vivo study of corneal surface morphologic features in patients with keratoconjunctivitis sicca. Am J Ophthalmol 1984; 98: 426–428.
Tobias CA, Blakely EA, Ngo FQH, Yang TCH . The rapair–misrepair model of cell survival. In: Meyn RE, Withers HR (eds) Radiation Biology in Cancer Research.. Raven Press: New York, 1980, pp 195–230.
Elkind MM, Sutton H . Radiation response of mammalian cells grown in culture. I. Repair of X-ray damage in surviving Chinese hamster cells. Radiat Res 1960; 13: 556–593.
Rubin NH . Influence of the circadian rhythm in cell division on radiation-induced mitotic delay in vivo. Radiat Res 1982; 89: 65–76.
Rubin P, Casarett GW Radiopathologic basis of the radiosensitivity and radioresistance of tumors. In: Clinical Radiation Pathology, Vol. II. WB Saunders: Philadelphia, 1968, pp 894–933.
Hanna C . Proliferation and migration of epithelial cells during corneal wound repair in the rabbit and the rat. Am J Ophthalmol 1966; 61: 55–63.
Lavker RM, Dong G, Cheng SZ, Kudoh K, Cotsarelis G, Sun TT . Relative proliferative rates of limbal and corneal epithelia. Implications of corneal epithelial migration, circadian rhythm, and suprabasally located DNA-synthesizing keratinocytes. Invest Ophthalmol Vis Sci 1991; 32: 1864–1875.
Cotsarelis G, Cheng SZ, Dong G, Sun TT, Lavker RM . Existence of slow-cycling limbal epithelial basal cells that can be preferentially stimulated to proliferate: implications on epithelial stem cells. Cell 1989; 57: 201–209.
Tannock IF, Hayashi S . The proliferation of capillary endothelial cells. Cancer Res 1972; 32: 77–82.
Calvo W, Hopewell JW, Reinhold HS, Yeung TK . Radiation induced damage in the choroid plexus of the rat brain: a histological evaluation. Neuropathol Appl Neurobiol 1986; 12: 47–61.
De Gowin RL, Lewis LJ, Hoak JC, Mueller AL, Gibson DP . Radiosensitivity of human endothelial cells in culture. J Lab Clin Med 1974; 84: 42–48.
Yao KT . Haploid cells in rat kangaroo corneal endothelium cultures and X-ray-induced chromosome aberrations. Genetics 1971; 67: 399–409.
Matsuda M, Sawa M, Edelhauser HF, Bartels SP, Neufeld AH, Kenyon KR . Cellular migration and morphology in corneal endothelial wound repair. Invest Ophthalmol Vis Sci 1985; 26: 443–449.
Levin LA, Gragoudas ES, Lessell S . Endothelial cell loss in irradiated optic nerves. Ophthalmology 2000; 107: 370–374.
Archer DB, Amoaku WM, Gardiner TA . Radiation retinopathy—clinical, histopathological, ultrastructual and experimental correlations. Eye 1991; 5: 239–251.
Egbert PR, Fajardo LF, Donaldson SS, Moazed K . Posterior ocular abnormalities after irradiation for retinoblastoma: a histopathological study. Br J Ophthalmol 1980; 64: 660–665.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kiuchi, T., Tatsuzaki, H., Hommura, S. et al. Specular microscopic study of X-ray-irradiated rabbit cornea. Eye 18, 929–934 (2004). https://doi.org/10.1038/sj.eye.6701350
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701350