Abstract
Aims To report on the clinical efficacy of verteporfin photodynamic therapy (PDT) in the treatment of choroidal neovascularisation (CNV) in an NHS setting and to compare treatment rates and outcomes with those in the published literature.
Patients and methods Patients with a visual acuity of 6/60 or better Snellen equivalent and predominantly classic or classic/no occult CNV within 200 μm of the centre of the fovea were enrolled and followed for a minimum of 12 months. Assessment at baseline and all follow-up visits comprised refraction protocol logMAR visual acuity, contrast sensitivity, and stereoscopic fluorescein angiography.
Results A total of 170 eyes of 159 patients were enrolled with CNV due to: 147 age-related macular degeneration (AMD) (90 classic/no occult, 21 recurrent after confluent laser, 36 predominantly classic with occult), 10 pathological myopia, and 13 others. Response to treatment (loss of <15 letters) at 12 months was 73% overall, 76% in AMD, 70% in classic/no occult, and 89% in predominantly classic. The mean number of treatments in the first year was 2.7. Contrast sensitivity was unchanged.
Conclusions Verteporfin PDT delivered in a NHS setting can be at least as effective as and requires fewer treatments than reported in the literature.
Similar content being viewed by others
Introduction
Subfoveal choroidal neovascularisation (CNV) is a major cause of visual disability in the developed world.1, 2, 3 While a number of conditions such as pathological myopia, angioid streaks, and punctate inner choroidopathy cause CNV particularly in younger patients, the great majority is due to age-related macular degeneration (AMD). This condition increases sharply with age, and thus is likely to become increasingly prevalent with ageing of the population.
In the treatment of age-related macular degeneration with photodynamic therapy (TAP) study, verteporfin photodynamic therapy (PDT) has been shown to be effective in reducing the likelihood of visual loss due to CNV in AMD when the lesion is predominantly classic and/or classic/no occult.4, 5 Evidence from the Verteporfin in PDT (VIP) study also indicates a beneficial treatment effect in selected occult/no classic lesions, and in CNV in pathological myopia.6, 7 While PDT has thus been effective in clinical trials, very real questions have remained as to its feasibility and cost-effectiveness in the more general UK National Health Service (NHS) setting with its inherent delays and constraints.8 In the UK, the National Institute for Clinical Excellence has been conducting an appraisal of the clinical effectiveness of PDT, a process that is being mirrored in many countries worldwide.9 Data from routine clinical practice are needed to inform this process.
In this paper, we present the 12-month clinical experience of PDT in an NHS setting in a regional medical retina service, including types of lesions treated and number of treatments per patient, and we compare the visual outcomes with baseline characteristics. We also present retreatment guidelines that were developed specifically for this new service. In addition, we postulate that it might be possible to give fewer re-treatments than in the TAP study, while still maintaining a clinical benefit.
Materials and methods
The population studied comprised all patients with CNV enrolled in a named patient verteporfin PDT treatment program at St. Paul's Eye Unit, Royal Liverpool University Hospital. Patients were initially identified on the basis of referral by an ophthalmologist and accompanying fluorescein angiograms. If these suggested that entry criteria were likely to be met, then the appropriate Health Authority was contacted with a request for funding for assessment ± treatment, which, if granted, was followed by a screening visit.
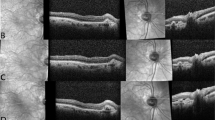
Screening assessment followed published procedures from TAP4, and was performed by staff previously accredited by TAP. In brief, after protocol refraction, best-corrected visual acuity (VA) was measured on a logMAR chart and contrast sensitivity on a Pelli–Robson chart, both at 1 m. Stereoscopic 30-degree fluorescein angiography was recorded on film using a Zeiss FF450+ camera with × 2.9 magnification. After clinical examination, lesion characterisation including measurement of the greatest linear dimension was undertaken by investigators from TAP (SPH, MCB).
Eligibility criteria, detailed in Table 1, were based on TAP,4 but with limited extension developed at expert workshops between 1999 and 2001 in Liverpool10 to include juxtafoveal lesions, lesions larger than 5400 μm and lesions due to causes other than AMD. A few patients were also enrolled for follow-up, having started their treatment elsewhere if baseline logMAR visions and lesion characteristics were available from their referring centres. Patients with CNV secondary to pathological myopia were only recruited in the presence of a history of recent reduction of vision.
Patients were seen for follow-up every 3 months, with protocol assessments performed as at baseline. Re-treatment was undertaken if the angiographic and clinical features suggested continued CNV activity. Eight clinical and angiographic factors that were considered in deciding whether to retreat were also developed at expert workshops, and are listed in Table 2.
Data from the first 12 months of follow-up were analysed using descriptive statistics, Student's t and χ2 tests. Response to treatment was defined as loss of fewer than 15 letters on the logMAR chart, and was the primary end point. This is equivalent to doubling of the visual angle, a standard developed in previous landmark ophthalmic studies to represent moderate visual loss.11, 12 Other measures of clinical efficacy studied were mean logMAR VA (letters), mean loss of distance VA (letters) contrast sensitivity, and greatest linear dimension on fundus fluorescein angiography.
Results
Between 5/11/99 and 13/07/01, 170 eyes of 159 patients were enrolled and treated at baseline. The underlying pathology was AMD in 147 eyes, pathological myopia in 10, juxtapapillary membranes in four, idiopathic in four, angioid streaks in two, and one each of dominant drusen, previous laser to central serous retinopathy and presumed toxoplasmosis scar. Of the AMD eyes, 111 of 147 had classic/no occult lesions, including 21 patients with recurrent CNV following previous confluent thermal laser treatment, and 36 had predominantly classic lesions with occult. Of the eyes treated, 41 were considered ‘first eyes’ with vision in the fellow eye of 63 letters or more (approximately 6/18). 109 were second eyes (VA< 63 letters) and 11 patients received bilateral treatment.
Data on 12-month follow-up were available for 143 eyes (84%) and 9-month data were available and included in the analysis, as the last observation brought forward, for a further eight eyes (5%). In the 19 eyes (11%) in whom follow-up was not available, this was due to death in two patients, ill health in one, fluorescein allergy at 3 months in one, and discharge to local follow-up in nine patients. Five patients failed to attend for follow-up, with no explanation given. The overall response rate in those with follow-up data was 72%. In the group with AMD, follow-up data were available at 12 months for 130 eyes (88%). The response rate among those with AMD was 71%. More detailed data on response rate by baseline characteristics are given in Table 3.
The proportion of eyes requiring treatment decreased with subsequent visits as shown in Figure 1. The average number of treatments in the first year was 2.7, excluding any treatment received at the 12-month visit.
VA declined over time in all the groups, except those with myopia. The mean visual acuity at baseline was 50 letters (approximately 6/30) for the group as a whole, and this had declined to 41 letters (approximately 6/36) by 12 months. In the subgroup with myopia, there was a small increase in mean vision from 57 letters to 59 letters. Those patients with AMD and classic/no occult lesions lost an average of 11 letters and those with predominantly classic lesions with occult lost an average of 4 letters. The mean vision at each time point for each of the groups is illustrated in Figure 2.
Contrast sensitivity was not measured at every visit, due to time constraints. However, data were available at baseline in 139 eyes and, of these, 99 (71%) also had 12-month contrast sensitivity data. Contrast sensitivity was stable in the group over the period of follow-up. The mean number of letters seen on the Pelli–Robson chart at baseline and 12 months was unchanged at 22. The mean contrast sensitivity at each point in follow-up is shown in Figure 3.
We compared those who had good vision in their fellow eye (≥63 letters, approximately 6/18) with those whose fellow eye had poor vision, excluding those who had bilateral treatment. There was no significant difference in response rate for first eyes compared with second eyes (first eye 72%, second eye 69% (P=0.76)).
The influence of lesion size on outcome was also investigated. The mean greatest linear dimension (GLD) of the lesions seen in our patients was 3335 μm (range 345–6827). The baseline lesion size was lower in responder eyes than nonresponders, but the difference was not statistically significant (mean GLD in responders = 3208μm, non-responders = 3648 μm, P=0.1). The response rate at 12 months was 9/14 (64%) for eyes with a GLD >5400 μm at baseline, compared with 72% in those with lesions ≤5400 μm. However, this difference was also not statistically significant (P= 0.33). A greater proportion of eyes with larger lesions experienced a loss of 20 or more letters between baseline and 3 months compared with smaller lesions, but this also was not statistically significant (GLD > 5400 μm, 3/14 (21%) GLD ≤5400 μm, 19/137 (13%) P=0.44.) One of the larger GLD eyes subsequently recovered to a loss of seven letters from baseline at the month 12 follow-up visit.
Other than loss of 20 letters between baseline and 3 months, as outlined above, other adverse reactions were as expected from TAP data, and included hypersensitivity in one patient, back pain in nine patients, photosensitivity in two patients, and transient visual loss in two patients.
Discussion
Our response rate at 12 months of 72% in eyes with AMD is very similar to the response rate at 12 months of 67% in the TAP predominantly classic subgroup. 4 This is encouraging, as it not only adds weight to the findings from TAP, but also shows that equally good results are possible outside the rigorous setting of a multicentre clinical trial.
The response rates in our patients varied somewhat, depending on baseline characteristics. In the group with AMD, those with classic/no occult lesions had a response rate of 66%, those with predominantly classic with occult had a response rate of 90%, and those in whom the lesion was a recurrence after confluent argon laser had a response rate of 58%. The high response rate in the predominantly classic with occult group may reflect lesions that were behaving less aggressively than those in the other groups. By contrast, the response rate in the recurrent after laser group was lower than the overall rate, and these lesions do seem to be difficult to control. The response rate was higher than that of the placebo group in the TAP study at 1 year, but further study is needed to determine whether there is indeed a true treatment benefit in this subgroup. In the group with myopia, the response rate was 67% using either our definition, or that of the VIP study of loss of fewer than eight letters. Caution needs to be exercised in interpreting our results for this group, as we only have information on nine patients. However, our results are similar to the VIP response rate at 12 months of 72%7 and indicate a beneficial effect of treatment in patients with pathological myopia, at least in the short term.
Overall, there was a mean decrease in VA of nine letters (1.8 lines on the ETDRS chart) at 12 months. As expected, this loss occurred mainly in the first 3–6 months, following which the mean acuities were relatively stable. Interestingly, the mean VA loss was much higher at 11 letters in the group with classic/no occult lesions compared to the group with predominantly classic with occult lesions, in which the mean loss was only four letters. This reflects the greater response rate in the group with partly occult lesions, and may again be an indication of lesions that are not as aggressive. The group with myopia showed an increase in mean vision of two letters on the ETDRS chart. This is a similar finding to that of the VIP myopia study in which there was a mean increase of 0.2 lines (one letter) at 12 months.7
Contrast sensitivity remained stable in all of the subgroups at the 12-month follow-up. This mirrors findings in the TAP 4, 5 and VIP7 studies, in which the treated groups retained stable contrast sensitivity, whereas the placebo groups experienced a decrease in contrast sensitivity. Contrast sensitivity has been shown to be important in visual functioning in patients with AMD.13
We treated 14 patients with lesions greater than 5400 μm maximum diameter who would not have been included in the TAP study. The response rate at 64% was lower than the 74% in the group with smaller lesions. Patients with larger lesions were more likely to suffer an early drop in vision and, indeed, three out of 14 (21%) patients in this group did lose 20 or more letters between baseline and 3 months. One of these subsequently recovered to a loss of seven letters from baseline at the month 12 follow-up visit. By comparison, in the group with smaller lesions, there was a loss of 20 letters or more in 19 of 137 (13%) patients out of a total of 118 at the month 3 visit, with subsequent recovery in 4. Although numbers were small in the larger lesion group and the differences between the groups were not statistically significant, the possibility that treatment effectiveness is poor in larger lesions merits further investigation.
At the 12-month follow-up, but excluding any treatment given at that visit, the average number of treatments per patient in our study was 2.7. This was less than the average in the treatment arm of the TAP study of 3.4 treatments at the same time point.4 In the TAP study, retreatment was based purely on the presence or absence of leakage on fluorescein angiography. In our patients, greater freedom was allowed for the clinician to consider a range of factors during re-treatment decision-making, using criteria developed for the service (Table 2). Clinical indices of continuing activity comprised the presence of blood, exudates, subretinal fluid (especially if under the foveal centre) or decreasing VA. Most loss of acuity occurs during the first 6 months in both treated and untreated eyes, and treatment can therefore reasonably be expected to have the greatest effect early in the disease history. As a result, re-treatment tended not to be applied after 9 months in the absence of definite features of progression. Treatment was not repeated in the presence of a large serous RPE detachment due to increased risk of an RPE tear. Finally, re-treatment was not performed if there was evidence that the patient was unlikely to notice any benefit—if the VA had dropped below 20 letters (approximately 3/60) or an RPE tear had developed. Our finding of similar visual outcomes as TAP but with fewer treatments gives important information to funding agencies in planning PDT services, as it suggests that the number of treatments required may not be as high as first indicated.
Many funding agencies will only authorise treatment at present for second or only eyes, typically where end-stage AMD has developed in the fellow eye. In our study, there was no difference in the response rate between first and second eyes. Cost utility analyses that have been performed to date are based solely on treatment of the better seeing eye.14 Further cost-effectiveness studies including measurement of visual functioning and quality of life are required to allow purchasers to make informed decisions on the value of treating first eyes.
Conclusions
The results of verteporfin PDT in AMD in a regional NHS service were comparable to those in the TAP study. These results could be achieved with fewer retreatments than used in clinical trials. In myopia and other underlying pathology, early indications suggest good results at least in the short term. This evidence of good effectiveness in NHS practice should encourage funding agencies in this and other similar public-funded health systems, to proceed with PDT service development.
References
Klein R, Klein BE, Linton KL . Prevalence of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology 1992; 99: 933–943.
Vingerling JR, Dielemans I, Hofman A et al. The prevalence of age-related maculopathy in the Rotterdam study. Ophthalmology 1995; 102: 205–210.
Bressler NM, Bressler SB, Fine SL . Age-related macular degeneration. Surv Ophthalmol 1988; 32: 375–413.
TAP study group. Photodynamic therapy of subfoveal choroidal neovascularisation in age-related macular degeneration with verteporfin: one-year results of 2 randomised clinical trials. TAP report. Arch Ophthalmol 1999; 117: 1239–1245.
TAP study group. Photodynamic therapy of subfoveal choroidal neovascularisation in age-related macular degeneration with verteporfin: two-year results of 2 randomised clinical trials. TAP report 2. Arch Ophthalmol 2001; 119: 198–207.
VIP study group. Verteporfin therapy of subfoveal choroidal neovascularisation in age-related macular degeneration: two-year results of a randomised clinical trial including lesions with occult with no classic choroidal neovascularisation – verteporfin in photodynamic therapy report. Am J Ophthalmol 2001; 131: 541–560.
VIP study group. Photodynamic therapy of subfoveal choroidal neovascularisation in pathologic myopia with verteporfin: one-year results of a randomised clinical trial – VIP report no. Ophthalmology 2001; 108(5): 841–852.
Harding SP . Verteporfin photodynamic therapy in the UK: implications of the NICE appraisal. Eye 2003; 17: 119–122.
National Institute for Clinical Excellence. Final appraisal determination: photodynamic therapy for age-related macular degeneration. http://www.nice.org.uk/Docref.asp?d=5410. Accessed 25-05-2003.
Harding SP . Photodynamic Therapy in the Treatment of Subfoveal Choroidal Neovascularisation. Eye 2001; 15: 407–412.
Early Treatment Diabetic Retinopathy Study Research Group. Early treatment diabetic retinopathy study design and baseline patient characteristics: ETDRS Report Number. Ophthalmology 1991; 98: 741–756.
Macular Photocoagulation Study. Argon laser photocoagulation for senile macular degeneration. Results of a randomized clinical trial. Arch Ophthamol 1982; 100: 912–918.
McClure ME, Hart PM, Jackson AJ, Stevenson MR, Chakravarthy U . Macular degeneration: do conventional measurements of impaired vision equate with visual disability? Br J Ophthalmol 2000; 84: 244–250.
Sharma S, Brown GC, Brown MM, Hollands H, Shah GK . The cost-effectiveness of photodynamic therapy for fellow eyes with subfoveal choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology 2001; 108: 2051–2059.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding: St. Paul's Eye Unit has received departmental commercial funding as a clinical centre in TAP and VIP. ST, MCB and SPH have received support for travel and conference attendance.
Previously presented as a poster at the Annual Congress of the Royal College of Ophthalmologists May 2002.
Rights and permissions
About this article
Cite this article
Barnes, R., Gee, L., Taylor, S. et al. Outcomes in verteporfin photodynamic therapy for choroidal neovascularisation—‘beyond the TAP study’. Eye 18, 809–813 (2004). https://doi.org/10.1038/sj.eye.6701329
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701329
Keywords
This article is cited by
-
Neovascular age-related macular degeneration: decision making and optimal management
Eye (2010)
-
Baseline clinical measures and early response predict success in verteporfin photodynamic therapy for neovascular age-related macular degeneration
Eye (2010)
-
Photodynamische Therapie bei altersbedingter Makuladegeneration am schlechteren und besseren Auge
Der Ophthalmologe (2007)
-
Bevacizumab: a new way of doing business?
Eye (2006)
-
Influence of photodynamic therapy for age related macular degeneration upon subjective vision related quality of life
Graefe's Archive for Clinical and Experimental Ophthalmology (2006)