Abstract
Background Owing to contradictory results, HLA matching in penetrating keratoplasty still is equivocal. Different surgical techniques in multicentre studies, missing risk differentiation in high-risk situations, and faulty HLA typing can be identified as main reasons for these contradictory results. In this monocentre study, the value of HLA class I and II matching (A, B, DR loci) was examined in a homogeneous group of 418 normal-risk keratoplasty patients using serological typing techniques for HLA class I and immuno-genetic typing techniques for class II.
Methods Penetrating normal-risk keratoplasty was performed in two groups of patients (group I with 0–2, group II with 3–6 mismatches in the A/B/DR loci). All surgery was carried out by three experienced surgeons according to a standardized scheme. Furthermore, postoperative therapy and controls were standardized. There were no statistically significant differences between the two study groups with regard to the number of ABO or H-Y compatibilities, patient age, patient gender, ratio of previous intraocular surgery, ratio of triple procedures, indication for surgery, follow-up period, donor age, donor gender, post-mortem time of the graft, and endothelial cell density of the graft at the end of organ culture. All HLA typing was performed in a quality-controlled laboratory, serologically for HLA class I (A and B loci) and immunogenetically for HLA class II (DR locus).
Results At 4 years postoperatively, the ratio of clear and rejection-free graft survival was 92% in group I and 66% in group II (Kaplan–Meier estimation, log rank test, P=0.03). Monovariate analysis in the Cox model gave no influence of solitary HLA class I or II matching, but only an influence of combined HLA class I and II matching (P=0.03).
Conclusions In this monocentre study with proper typing techniques, the beneficial effect of HLA class I plus II matching on clear and rejection-free graft survival could be demonstrated in a homogeneous group of normal-risk keratoplasty patients.
Similar content being viewed by others
Background
Almost one century after the first successful penetrating keratoplasty,1 immune reactions are still a major problem in normal-risk as well as in high-risk situations.2,3,4 Owing to the immune privilege of the cornea and the anterior chamber,5,6,7,8 topical corticosteroid prophylaxis over some months postoperatively has been supposed to limit this complication sufficiently.9,10 In normal-risk keratoplasty about 18% and in high-risk situations up to 75% of the patients experience, however, immune reactions, often with subsequent graft failure.2,3,4 In order to improve graft prognosis, topical and/or systemic immunosuppressives may be administered in the long run, and/or HLA matched grafts may be used. In contrast to the first approach, HLA matching is not associated with side effects.
The beneficial effect of HLA class I and II matching in renal transplantation is unequivocal.11 Numerous penetrating keratoplasty studies performed within the past three decades gave, however, contradictory results.12,13,14,15,16,17,18,19,20,21,22,23,24,25 These contradictory results may be explained by three main reasons: (1) In multicentre studies with up to 200 centres and up to 400 surgeons, different surgical experience and techniques may influence the outcome.26 (2) Most studies were performed in high-risk patients with an elevated risk of immune reactions. Such patients may have additional risk factors such as surface disorders (eg in atopic keratoconjunctivitis or limbal stem cell deficiency) or glaucoma problems or they may experience viral or microbial recurrences.27 HLA matching has no influence on these additional risk factors, which may, of course, lead to irreversible graft failure, for example, in severest lime burn, the risk of graft failure from limbal stem cell deficiency alone may be 100% without necessity of an additional immune reaction. (3) In some studies, HLA typing was performed in laboratories that were not quality controlled. In the CCTS, concordance between original and retyping was only 55%.28,29 Völker-Dieben et al29 demonstrated that faulty HLA DR typing in only 5% abrogates the beneficial effect of HLA DR matching. HLA typing on an immunogenetic basis is the safest way to avoiding typing faults in HLA class II. This is especially true when blood obtained up to 72 h after the donor's death is analysed.11,30 In previous keratoplasty studies, however, HLA typing had been performed almost exclusively serologically.
In this study, faults committed in previous studies as mentioned above were avoided by a monocentre design with only three experienced cornea surgeons, by choosing normal-risk keratoplasty patients as participants, thus excluding nonimmunological reasons for graft failure, and by performing HLA typing in an optimally quality-controlled laboratory, serologically for class I and immunogenetically for class II.
Methods
Penetrating normal-risk keratoplasty was performed in a homogeneous monocentre group of 418 patients after approval by the local ethics committee and after obtaining written informed consent by every patient.
Patient selection
Only patients undergoing first keratoplasty within an avascular host cornea were included. All grafts with a diameter of 7.7 mm were positioned centrally. Indications for surgery were keratoconus, Fuchs’ endothelial dystrophy, bullous keratopathy, and nonherpetic scars. None of the patients had a history of severe surface disorders, glaucoma, or herpetic eye disease.
Since 1995, HLA typing has been performed in all normal-risk keratoplasty patients of the clinic. All patients were set on a waiting list for a maximum of 6 months. If a graft with 0–2 mismatches (group I) on the HLA A, B, and DR loci had not been found within this period, a graft with 3–6 mismatches was assigned (group II). Group I comprised 66, group II 352 patients: one patient received a graft with zero, 28 with one, 37 with two, 70 with three, 124 with four, 114 with five, and 44 with six mismatches. All relevant patient, donor, graft, and surgery data of both study groups are given in Tables 1ab and 2a.
HLA typing and matching
All serologic HLA A, B, and all immunogenetic HLA DRB, DRQB typings of donors and recipients were performed in a single laboratory accredited by the American Society for Histocompatibility and Immunogenetics.30 For HLA matching, only broad antigens (class I: A, B; class II: DR) were considered (Tables 2b and 2c).
Distribution of blood group mismatches (ABO)
ABO typing was performed serologically in the same optimally quality-controlled laboratory. In group I 40/66 patients and in group II 184/352 patients received ABO-matched grafts (donor A/recipient A or AB, donor B/recipient B or AB, donor AB/recipient AB, donor O/recipient A, B, AB, or O) (χ2 test, P=0.64) (Table 2a).
Distribution of minor histocompatibility H-Y mismatches
In group I 47/66 patients and in group II 244/352 patients received H-Y-matched grafts (donor male/recipient male, donor female/recipient male or female) (χ2 test, P=0.4) (Table 2a).
Grafts
All grafts were preserved in organ culture according to the guidelines of the European Eye Bank Association.31 Preoperative evaluation of the graft endothelium was performed in hypotonic solution under the phase contrast microscope the day before penetrating keratoplasty.32 This examination was proven to deliver reproducible results.33
Penetrating keratoplasty, postoperative treatment and controls
Surgery was performed by three experienced surgeons in retrobulbar anaesthesia according to a standardized scheme. Modified Franceschetti trephines with the diameters 7.5 mm (recipient) and 7.7 mm (donor) were used. Graft fixation was performed with a double running cross-stitch suture with Nylon 10.0.34 If necessary, cataract surgery was carried out simultaneously (Table 1a). After surgery, gentamycin ointment was administered at least until the graft was covered with a complete epithelial layer. Then corticosteroid eye drops (prednisolone-21-acetate 1%) were given five times daily and tapered during the first five postoperative months. All patients received 1 mg/kg body weight/day of systemic fluocortolon tapered within 3 weeks postoperatively. Acetazolamide was administered in a daily dose of 500 mg for 5 days postoperatively. Controls of the graft at the slit lamp were scheduled 6 weeks, 4, 12, and 18 months postoperatively and thereafter annually.
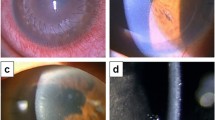
Immune reactions
Endothelial immune reactions were diagnosed via endothelial precipitates and stromal oedema, and stromal immune reactions via subepithelial infiltrates.35 All patients received corticosteroid eye drops (prednisolone-21-acetate 1%) every hour until elimination of all precipitates. Furthermore, a subconjunctival injection with betamethasone-21-acetate was performed. Topical corticosteroids were tapered individually. In severe cases, systemic corticosteroids at a daily oral dose of 1 mg fluocortolone/kg body mass were administered additionally and tapered within 3 weeks.
Statistical analysis
All statistical evaluation was performed using SSPS Windows NT 4.0 (Microsoft Corp., Redmond, USA). Clear graft survival, ratio of grafts without immune reactions, and rejection-free graft survival were calculated according to Kaplan and Meier.36 All Kaplan–Meier curves were compared via log rank test. Monovariate analysis was performed by entering patient, donor, graft, and surgery data into the Cox model.
Findings
At 4 years postoperatively, clear graft survival in group I was 100% and in group II 85% (P=0.065), ratio of rejection-free grafts was 92% in group I and 72% in group II (P=0.048) and ratio of clear and rejection-free graft survival was 92% in group I and 66% in group II (P=0.03) (Figure 1a–c Reasons for graft failure in group II were irreversible immune reactions in eight patients and chronic endothelial cell loss in three patients. In group I, four immune reactions were recorded. All were reversible. In group II, 50 of 58 immune reactions were reversible (Table 3).Monovariate analysis in the Cox model gave no influence of solitary HLA class I or II matching (P=0.31 and 0.13, respectively), but only an influence of combined HLA class I and II matching (P=0.03) on clear and rejection-free graft survival (Table 4).
An influence of blood group or minor H-Y compatibility on clear and rejection-free graft survival could not be demonstrated (Table 4). The same is true for patient age, patient gender, preceding or simultaneous intraocular procedures, donor age, donor gender, post-mortem time of the graft, time of the graft in organ culture, or endothelial cell density at the end of the culture period (Tables 5a and 5b).
Discussion
Many studies were performed within the past three decades considering the effects of HLA matching in penetrating keratoplasty. They delivered contradictory results (Table 6a and 6b).12,13,14,15,16,17,18,19,20,21,22,23,24,25 In this study, the beneficial effect of HLA class I plus II matching on clear and rejection-free graft survival after penetrating normal-risk keratoplasty could be demonstrated. Main difference between the two study groups was the number of HLA mismatches. All other factors possibly influencing study outcome were comparable. The study is unique because of five reasons:
-
1
In a monocentre design, only three experienced surgeons performed all transplantations according to a standardized scheme. Furthermore, all postoperative therapy and all postoperative examinations were performed in a standardized manner.
-
2
Only patients undergoing normal-risk keratoplasty were considered for the study in order to minimize the influence of nonimmunological risk factors. Another possibility would have been to study high-risk patients with an elevated risk for immune reactions as the only risk factor. Such patients are, however, much rarer than normal-risk patients.
-
3
Various patient, donor, and graft parameters may influence clear and rejection-free graft survival. In this study, patient age, patient gender, ratio of previous intraocular surgery, ratio of triple procedures, indication for surgery, and follow-up did not show statistically significant differences between the two study groups. The same is true for donor age, donor gender, post-mortem time, and endothelial cell density of the graft at the end of standardized organ culture. Only storage time in organ culture was statistically significantly longer in group I. If this had an influence on the study results, one might expect worse results in the group with the longer storage period.37,38 The contrary, however, was observed.
-
4
In the past, the influence of blood group compatibility on graft prognosis was discussed controversially.22 It may be important, therefore, that the number of patients with blood group compatibilities was comparable in both study groups. An influence of minor histocompatibility mismatches on graft prognosis was found by Streilein39 in the mouse penetrating keratoplasty model. The only minor histocompatibility antigen investigated in this study was H-Y. In the two study groups, the number of patients with minor histocompatibility antigen H-Y mismatches was similar.
-
5
All HLA typing was performed in only one quality-controlled laboratory, serologically for class I and immunogenetically for class II. In the past, serological typing of class I was shown to deliver reliable results.30 This is not the case for HLA class II, even if material from heart-beating donors is analysed.28,29 In penetrating keratoplasty, however, blood from cornea donors is often obtained up to 72 h after death. In this study, therefore, the DR locus was determined exclusively by immunogenetic means.30
The expression of class I and II antigens in the cornea is still controversially discussed. Streilein5 identified reduced expression of MHC antigens as one reason for the immune privilege of corneal grafts. Newsome et al40 demonstrated the presence of class I antigens on epithelial, stromal, and endothelial corneal cells. In contrast, class II antigens are regularly expressed only on epithelial Langerhans cells.41 After incubation with gamma-interferon, however, class II antigens are expressed on all corneal cells including the endothelium.42,43 CD4 T cells are the main source of gamma-interferon.44 In the rat penetrating keratoplasty model, CD4 T cells were found even in syngeneic grafts.45 Possibly, an elevation of gamma-interferon levels in the graft may already be caused by a surgical trauma such as penetrating (normal-risk) keratoplasty.
The evolution in keratoplasty has been such that the early attempts to exploit the theoretical advantages of HLA matching had unavoidably too often been technically weak so that the probability of negative or questionable results was high. On the other hand, the introduction of more and more efficient systemic immunodrugs has brought about such a quick and important breakthrough in the prognosis especially of high-risk keratoplasties that the current ‘neglect’ of the HLA system is understandable from this experience.
We have shown that even patients with a normal-risk keratoplasty benefit from a good HLA A/B plus HLA DR match. As others29,46 have recently published that HLA matching is beneficial also in high-risk and mixed-risk groups, these unisono reports mean that HLA matching must now be regarded as basically beneficial for all keratoplasty patients.
It does not follow that HLA matching must actually be required for every patient. For the time being, the practical consequences will anyway be limited because the logistics for a widespread application of matching principles in keratoplasty do simply not yet exist in most parts of the world. It must be discussed, however, whether it will be worthwhile to establish such logistics. We vigorously favour such a project.
For normal-risk patients, we would expect that their transplants’ lifespan, which currently on an average is not longer than about 10–20 years, will be considerably expanded. This is extremely important for all patients under the age of about 60 years. For high-risk patients, efficient HLA matching will help to bring about conditions in which tolerance of the graft by the host is established more easily and more efficiently and longer lasting than with systemic immunomodulative drugs alone. The application of the latter is often limited by severe side effects, or their effect may be insufficient when given as the only measure.
Thus, all keratoplasty patients should benefit to various degrees from HLA matching, and it is our hope that this paper together with those of others29,46 will lead to a re-evaluation and reappraisal of HLA matching in keratoplasty.
References
Zirm E . Eine erfolgreiche totale Keratoplastik. Graefe's Arch Clin Exp Ophthalmol 1906; 64: 581–593.
Hill JC . The use of cyclosporine in high risk keratoplasty. Am J Ophthalmol 1989; 107: 506–510.
Hill JC . Systemic cyclosporine in high risk keratoplasty. Short-versus long-term therapy. Ophthalmology 1994; 101: 128–133.
Reinhard T, Hutmacher M, Sundmacher R, Godehardt E . Akute und chronische Immunreaktionen nach perforierender Keratoplastik mit normalem Immunrisiko. Klin Monatsbl Augenheilkd 1997; 210: 139–143.
Streilein J . Unraveling immune privilege. Science 1995; 270: 1158–1159.
Niederkorn JY, Mellon J . Anterior chamber-associated immune deviation promotes corneal allograft survival. Invest Ophthalmol Vis Sci 1996; 36: 1530–1540.
Yamada J, Streilein JW . Induction of anterior chamber-associated immune deviation by corneal allografts placed in the anterior chamber. Invest Ophthalmol Vis Sci 1997; 38: 2833–2843.
Sano Y, Okamoto S, Streilein JW . Induction of donor-specific ACAID can prolong orthotopic corneal allograft survival in ‘high-risk’ eyes. Curr Eye Res 1997; 16: 1171–1174.
Sundmacher R . Immunreaktionen nach Keratoplastik. Klin Monatsbl Augenheilkd 1977; 171: 705–722.
Sundmacher R, Stefansson A, Mackensen G . Verlaufsbeobachtungen nach Keratoplastik. Fortschr Ophthalmol 1983; 80: 224–227.
Opelz G, Mytilineos J, Scherer S, Dunckley H, Trejaut J, Chapman J et al. Analysis of HLA-DR matching in DNA-typed cadaver kidney transplants. Transplantation 1993; 55: 782–785.
Gibbs DC, Batchelor R, Werb A, Schlesinger W, Casey TA . The influence of tissue-type compatibility on the fate of full-thickness corneal grafts. Trans Ophthalmol Soc 1974; 94: 101–126.
Vannas S . Histocompatibility in corneal grafting. Invest Ophthalmol 1975; 14: 883–886.
Stark WJ, Hugh RT, Bias WB, Maumenee AE . Histocompatibility (HLA) antigens and keratoplasty. Am J Ophthalmol 1978; 86: 595–604.
Ehlers N, Kissmeyer-Nielsen F . Corneal transplantation and HLA histocompatibility. Acta Opthalmol 1979; 57: 738–741.
Foulks GN, Sanfilippo FP, Locasio JA, MacQueen JM, Dawson DV . Histocompatibility testing for keratoplasty in high-risk patients. Ophthalmology 1983; 90: 239–244.
Sanfilippo F, MacQueen JM, Vaughn WK, Foulks GN . Reduced graft rejection with good HLA-A and -B matching in high-risk corneal transplantation. New Engl J Med 1986; 315: 29–35.
Völker-Dieben HJ, D’Amaro J, Kruit PJ, Lange P . Interaction between prognostic factors for corneal allograft survival. Transplant Proc 1989; 21: 3135–3138.
Boisjoly HM, Roy R, Bernard PM, Dubé I, Laughrea PA, Bazin R . Association between corneal allograft reactions and HLA compatibility. Ophthalmology 1990; 97: 1689–1698.
Baggesen K, Ehlers N, Lamm LU . HLA-DR/RFLP compatible corneal grafts. Acta Ophthalmol 1991; 69: 229–233.
Beekhuis WH, van Rij G, Renardel de Lavalette JG, Rinkel-van Driel E, Persijn G, D’Amaro J . Corneal graft survival in HLA-A-and HLA-B-matched transplantations in high-risk cases with retrospective review of HLA-DR compatibility. Cornea 1991; 10: 9–12.
CCTS. Effectiveness of histocompatibility matching in high-risk corneal transplantation. Arch Ophthalmol 1992; 110: 1392–1403.
Vail A, Gore SM, Bradley BA, Easty DL, Rogers CA, Armitage WJ . Conclusions of the corneal transplant follow up study. Br J Ophthalmol 1997; 81: 631–636.
Hoffmann F, Pahlitzsch T . Predisposing factors in corneal graft rejection. Cornea 1989; 8: 215–219.
Hoffmann F, Tregel M, Noske W, Bünte S . HLA-B and -DR match reduces the allograft rejection after keratoplasty. Ger J Ophthalmol 1994; 3: 100–104.
Gore SM, Vail A, Bradley BA, Rogers CA, Easty DL, Armitage WJ . HLA-DR matching in corneal transplantation: systematic review of published data. Transplantation 1995; 110: 1392.
Reinhard T, Sundmacher R, Heering P . Systemic Cyclosporin A in high-risk keratoplasties. Graefe's Arch Clin Exp Ophththalmol 1996; 234 (Suppl 1): 115–121.
Hopkins KA, Maguire MG, Fink NE, Bias WB . Reproducibility of HLA-A, -B, and -DR typing using peripheral blood samples: results of retyping in the CCTS. Hum Immunol 1992; 22: 132.
Völker-Dieben HJ, Claas FHJ, Schreuder GMT, Schipper RF, Pels E, Persijn GG, Smits J, D’Amaro J . Beneficial effect of HLA-DR matching on the survival of corneal allografts. Transplantation 2000; 70: 640–648.
Wernet P, Kögler G, Enczmann J, Kuhröber A, Knipper A, Bonte W, Reinhard T, Sundmacher R . Rapid method for successful HLA Class I and II typing from cadaveric blood for direct matching in cornea transplantation. Graefe's Arch Clin Exp Ophthalmol 1998; 236: 507–512.
Pels L, Maas H, Tullo A . European Eye Bank Association Directory, 8th ed., 2000, EEBA, Amsterdam.
Böhnke M . Spendergewebe für die Keratoplastik. Klin Monatsbl Augenheilkd 1991; 198: 563–571.
Reinhard T, Holzwarth D, Spelsberg H, Dahmen N, Sundmacher R . Wissensbasierte Bildanalyse von Hornhauttransplantaten. Klin Monatsbl Augenheilkd 1999; 214: 407–411.
Hoffmann F . Nahttechnik bei perforierender Keratoplastik. Klin Mbl Augenheilk 1976; 169: 584–590.
Allredge OC, Krachmer JH . Clinical types of corneal transplant reaction. Arch Ophthalmol 1981; 99: 599–604.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Armitage WJ, Easty DL . Factors influencing the suitability of organ-cultured corneas for transplantation. Invest Ophthalmol Vis Sci 1997; 38: 16–24.
Borderie VM, Scheer S, Touzeau O . Donor organ cultured corneal tissue selection before penetrating keratoplasty. Br J Ophthalmol 1998; 82: 382–388.
Streilein JW . Immunobiology and immunopathology of corneal transplantation. In: Streilein JW (ed). Immune Response and the Eye. Chem Immunol, Vol 79. Karger: Basel, 1999, pp 186–206.
Newsome DA, Takasugi M, Kenyon K, Stark WF, Opelz G . Human corneal cells in vitro: morphology and histocompatibility antigens of pure cell populations. Invest Ophthalmol Vis Sci 1974; 13: 23–32.
Jager M . Corneal Langerhans cells and ocular immunology. Regional Immunol 1992; 4: 186–195.
Donelly JJ, Li W, Rockey JH, Prendergast RA . Induction of class II alloantigen expression on corneal endothelium in vivo and in vitro. Invest Ophthalmol Vis Sci 185; 26: 575–580.
Young E, Stark WJ, Prendergast RA . Immunology of corneal allograft rejection: HLA-DR antigens on human corneal cells. Invest Ophthalmol Vis Sci 1985; 26: 571–574.
Vilcek J, Jumming L . Inferon gamma. In: Delves PJ, Roitt IM (eds). Encyclopedia of Immunology. Academic Press: San Diego, 1999, pp 1421–1426.
Reis A, Megahed H, Reinhard T, Godehardt E, Spelsberg H, Braunstein S et al. Coadministration of the new macrolide RAD and Mycophenolate mofetil in experimental corneal transplantation. Transplantation 2000; 70: 1397–1401.
Beekhuis WH . Langzeitergebnisse bei HLA-A und B gematchter Hochrisiko-Keratoplastik. Ophthalmologe 2001; 98: S6–S7.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the Bio Implant ServicesLeiden, NL
Proprietary interest: None
A special symposium took place on 30 September 2001 at Berlin which covered many problems and questions beyond the scope of this paper. The proceedings of this symposium will be published in a booklet separately
Rights and permissions
About this article
Cite this article
Reinhard, T., Böhringer, D., Enczmann, J. et al. Improvement of graft prognosis in penetrating normal-risk keratoplasty by HLA class I and II matching. Eye 18, 269–277 (2004). https://doi.org/10.1038/sj.eye.6700636
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700636
Keywords
This article is cited by
-
Gender medicine in corneal transplantation: influence of sex mismatch on rejection episodes and graft survival in a prospective cohort of patients
Cell and Tissue Banking (2021)
-
Development and characterization of Lyophilized Transparized Decellularized stroma as a replacement for living cornea in deep anterior lamellar keratoplasty
Cell and Tissue Banking (2019)
-
Humanes Leukozytenantigensystem in der Augenheilkunde
Der Ophthalmologe (2013)
-
100 Jahre erfolgreiche Hornhauttransplantation
Spektrum der Augenheilkunde (2007)
-
Intrakamerale Applikation von Kortikosteroiden zur Therapie der schweren endothelialen Abstoßung nach perforierender Keratoplastik
Der Ophthalmologe (2007)