Abstract
Aim To study the association between chronic hepatitis C virus (HCV) and Mooren's type keratitis.
Method A total of 50 patients with chronic HCV were screened for any evidence of corneal ulceration. Detailed ocular examination was conducted by slit-lamp biomicroscopy. Patients with history of trauma to the eye or previous herpetic keratitis were excluded from the study.
Results There were 37 males and 13 females. The age of the patients ranged from 10 to 70 years. There was no evidence of Mooren's ulcer in any of our patients.
Conclusion No association between chronic HCV and Mooren's ulcer was found in our study. Screening therefore in such cases is not necessary.
Similar content being viewed by others
Introduction
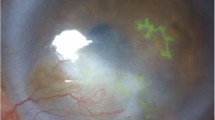
The worldwide incidence of hepatitis C virus (HCV) infection as estimated by World Health Organization is 3% and around 170 million individuals are estimated to be chronic carriers at risk of developing HCV infection.1 HCV infection has been associated with a range of different conditions2,3 that may or may not be causally linked to the hepatic infection. Viral, genetic, or possibly environmental factors may be responsible for the reported high frequency of systemic complications associated with chronic HCV infection.4 Infection with HCV has also been reported to be associated with Mooren's ulcer.5,6,7,8 Mooren's ulcer is a chronic relentlessly progressive, peripheral ulcerative keratitis. The aetiology of the disease has remained elusive. Autoimmunity has been suggested to have a role in the pathophysiology of the disease.9 Differences in therapeutic response between group of patients have suggested that Mooren's ulcer may be more than one disease with similar clinical and pathologic signs. Although most cases have been idiopathic,10,11,12 others are associated with trauma,10,13 cataract,14,15 and corneal surgery,16 alkali burns,10,13 herpes zoster,13,17 and herpes simplex.13 Case reports of infection with HCV have been reported to be associated with Mooren's ulcer. But no large series is available in the literature. Our aim is to know the occurrence of Mooren's type HCV-associated corneal ulceration in patients suffering from HCV infections.
Materials and methods
A total of 50 patients with diagnosed chronic HCV infection (positive serology for HCV) were recruited in the study from Hepatology Clinic of Nehru Hospital, PGIMER, Chandigarh. Detailed medical history was taken and anterior segment examination of the eyes was conducted on slit lamp, especially looking for features of Mooren's ulceration, which include:
-
1
Intense limbal inflammation and oedema of the episclera and conjunctiva without scleral involvement.
-
2
Crescent-shaped peripheral corneal ulcer commencing slightly central to corneo-scleral limbus.
-
3
Undermining of the central edge of the ulcer.
-
4
Stromal yellow/white infiltrates in advance of the ulcer.
-
5
Central and circumferential progression of the ulcer leaving a thin vascularised cornea behind.
Fundus examination was conducted to rule out any vasculitis.
It was also included in the protocol that in the event of diagnosis of Mooren's ulcer, various laboratory investigations such as antinuclear antibodies (ANF), rheumatoid factor, and antineutrophil cytoplasmic antibodies (ANCA) will be conducted to rule out any systemic cause of noninfectious corneal ulceration.
Exclusion criteria: A patient with history of:
-
1
Trauma to eye or alkali burns.
-
2
Cataract or corneal surgery.
-
3
Herpes simplex or herpes zoster.
-
4
Collagen vascular disorders.
-
5
Patients who were receiving therapy or who had undergone treatment with interferon.
The study was approved by the local ethics committee.
Results
The age of our patients ranged from 10 to 70 years (mean 46.2±5.4). There were 37 males and 13 females. None of the patients with chronic HCV infection had any clinical evidence of Mooren's ulceration. There were no clinical findings suggestive of systemic vasculitis. General ocular examination was unremarkable.
Discussion
The annual incidence of HCV in South East Asia is largely unknown because over 50% of infectious cases are asymptomatic. In addition, many symptomatic acute cases are not laboratory confirmed since testing of patients for HCV markers is not commonly carried out. In India, HCV antibodies have been found in less than 2% of voluntary blood donors.18 The clinical infection is often mild, usually asymptomatic with a high rate of chronic hepatitis (>50%). Our study was designed to see for the occurrence of keratitis in patients with HCV infection.
Wilson et al6 reported in 1994 that Mooren's ulcers may be linked to hepatitis C, but the probability of Mooren's ulcer in such patients was less than 1 : 10 000 considering the prevalence of HCV antibody to be 1%. He acknowledged at least 14 patients with Mooren's ulcers who also had hepatitis C.18 Three patients learned of the infection after development of the corneal ulcers. Also, the patients responded to interferon alpha-2b subcutaneous injections, the standard therapy for hepatitis C. One patient who relapsed was cured by another 6-month regimen of interferon alpha-2b subcutaneous injections. If chronic HCV is associated with development of Mooren's ulcer, it may be important to treat the acute hepatitis C with interferon alpha-2b to prevent chronic infection.19 Also, various genotypes of HCV respond differently to interferon treatment.20,21 Recently, a patient with hepatitis C and progressive bilateral corneal ulceration has been reported to have responded to intravenous administration of steroids within 5 days.22 A favourable outcome with lamellar keratoplasty and antiviral treatment in a case of herpetic perforated peripheral corneal ulcer with cutaneous porphyria and hepatitis C has also been seen.23
The typical regimen for management of Mooren's ulcer begins with topical or oral steroids, then progresses to stronger immunosuppressive agents such as cyclosporine or cyclophosphamide. Surgical treatment includes removing the conjunctiva adjacent to the area of active corneal inflammation or excising the inflamed leading edge of the ulcer.24
It may not be worthwhile screening HCV patients for Mooren's ulcer but still worthwhile screening Mooren's ulcer patients for HCV. If patient is HCV positive, one may be cautious in giving stronger immunosuppressives like cyclophosphamide. Antiviral agent interferon alpha-2b is an effective treatment for chronic hepatitis caused by HCV.25,26,27 Interferon alpha-2b, given at dose of 3 million units subcutaneously, three times in a week for 6 months is the most common protocol.28,29 Using this regimen at least 50–60% of patients have a histologic improvement in chronic hepatitis.26,27 More than 50% of patients will experience a relapse within 6–12 months of discontinuation of interferon alpha-2b therapy.26,27 Most of these patients will respond to retreatment.27 Interferon alpha-2b caused at least temporary remission of eye disease in two previously reported series.7,8
Genetic susceptibility may explain why the condition is seen in some patients and not others. There can be multiple causes of Mooren's ulcers, and some of them may not be associated in any way with any underlying systemic viral illness. However, Wilson observed the possibility of a number of flaviviruses that could cause hepatitis and trigger Mooren's ulcer.18 Whether to pursue looking for other flaviviruses as suggested by Wilson needs further studies.
Possible mechanism suggested for keratitis include antigenic mimicry in which host immunity against hepatitis C antigen crossreacts with epitopically similar autoantigens or immunoreactivity directed against exogenous viral antigens absorbed into the cornea. The concentration of HCV RNA can be higher in the tear fluid than in the plasma, so the exposure of the ocular surface to a relatively higher viral antigen load is possible.30 Other factors must be involved in the development of corneal disease associated with HCV infection. Possible variables include localised corneal factors, requirement of antigen antibody ratios in the serum within a specific range to yield immune complexes of an appropriate size to deposit in the cornea from the limbal vessels, genetic immune response difference between individuals infected with HCV, and the well-documented diversity of HCV.31
Hepatitis C also is a flavivirus that can be detected with available antibody tests. But four new hepatitis viruses have been discovered.18 Makers of tests to detect the viruses have reported one or two of the five antigens for hepatitis C detected by the Matrix test may be positive in patients actually infected by another flavivirus.18 This finding led them to suspect that there are other viruses to pursue. Zegans et al32 in their study from south India showed that none of the 21 patients suffering from Mooren's ulcer tested positive for HCV. Another study from the UK concluded that chronic HCV does not increase prevalence of significant ocular disease.33
Our study was designed to determine whether there was any association between Mooren's ulcer and chronic HCV infection. In our study, patients were recruited from the hepatology clinic at a tertiary care teaching hospital. It is therefore likely that the patients will have more advanced liver disease than is typical for patients with chronic HCV. If chronic HCV does cause significant keratitis, it is more likely to be detected in patients with more advanced form of HCV. Our study reveals that there was no association of keratitis with chronic HCV.
From this study we conclude that Mooren's ulcer may not have significant relation with HCV. Chronic HCV infection may not be associated with aetiology of Mooren's like ulcer. Screening therefore for the evaluation of such cases is not necessary until the association between HCV and keratitis is definitely established. Since hepatitis C occurs in less than 2% of the Indian population, and since Mooren's ulcer is relatively rare, peripheral corneal ulceration would have to be an infrequent complication of hepatitis C infection.10
Until the association between HCV and keratitis is either definitely established or found to be coincidental, it is wiser that all patients with inflammatory peripheral keratitis without systemic rheumatological disease be tested for HCV or herpetic virus. Further studies of a large series of cases are needed to substantiate any evidence of an association between the two entities.
References
WHO. Global surveillance and control of hepatitis C. J Viral Hepatitis 1999; 6: 35–47.
Gordon SC . Extrahepatic manifestations of hepatitis C. Dig Dis 1996; 14: 157–168.
Hadziyannis S . Non-hepatic manifestations of chronic HCV infection. J Viral Hepatitis 1997; 4: 1–17.
Verbaan H, Carlson J, Eriksson S, Larsson A, Liedholm R, Manthorpe R et al. Extrahepatic manifestations of chronic hepatitis C infection and the interrelationship between primary Sjogren's syndrome and hepatitis C in Swedish patients. J Intern Med 1999; 245: 127–132.
Wilson SE, Lee WM, Murakami C, Weng J, Moninger GA . Mooren's corneal ulcers and hepatitis virus C infection [letter]. N Engl J Med 1993; 329: 62.
Wilson SE, Lee WM, Murakami C, Weng J, Moninger GA . Mooren's type hepatitis C virus associated corneal ulceration. Ophthalmology 1994; 101: 736–745.
Moazami G, Auran JD, Florakis GJ, Wilson SE, Srinivasan DB . Interferon treatment of Mooren's ulcers associated with hepatitis C. Am J Ophthalmol 1995; 119: 365–366.
Baratz KH, Fulcher SFA, Bourne WM . Hepatitis C-associated keratitis. Arch Ophthalmol 1998; 116: 529–530.
Brown SI, Mondino BJ, Rabib BS . Autoimmune phenomenon in Mooren's ulcer. Am J ophthalmol 1976; 82: 835–840.
Wood TO, Kaufman HE . Mooren's ulcer. Am J Ophthalmol 1971; 71: 417–422.
Brown SI . What is Mooren's ulcer? Trans Ophthalmol Soc UK 1978; 98: 390–392.
Mondino BJ . Peripheral corneal ulcers and thinning disorders. Perspect Ophthalmol 1980; 4: 9–15.
Brown SI, Mondino BJ . Therapy of Mooren's ulcer. Am J Ophthalmol 1984; 98: 1–6.
Arentsen JJ, Christiansen JM, Maumenee AE . Marginal ulceration after intracapsular cataract extraction. Am J Ophthalmol 1976; 81: 194–197.
Salamon SM, Mondino BJ, Zaidman GW . Peripheral corneal ulcers, conjunctival ulcers, and scleritis after cataract surgery. Am J Ophthalmol 1982; 93: 334–337.
Gottsch JD, Liu SH, Stark WJ . Mooren's ulcer and evidence of stromal graft rejection after penetrating keratoplasty. Am J Ophthalmol 1992; 113: 412–417.
Mondino BJ, Brown SI, Mondzelewski JP . Peripheral corneal ulcers with herpes zoster ophthalmicus. Am J Ophthalmol 1978; 86: 611–614.
Cunningham Jr ET, Wilson SE . Link between Mooren's ulcer, hepatitis C is questioned. Associated flaviviruses could cause corneal problems, yet go undetected by available tests. Ocular Surgery News. 15 January, 2000.
Jaeckel E, Cornberg M, Wedemeyer H, Santantonio T, Mayer J, Zantiel M et al. Treatment of acute hepatitis C with interferon alfa-2b. N Engl J Med 2001; 345: 1452–1457.
Takada N, Takase S, Takada A . Effects of genotypes of hepatitis C virus on interferon treatment for chronic type C hepatitis. Gastroentrol Jpn 1993; 28: 268–275.
Lopez-Labrador FX, Ampurdanes S, Gimenez-Barcons M, Guilera M, Costa J, Jimenez de Anta MT et al. Relationship of genomic complexity of hepatitis C virus with liver disease severity and response to interferon in patients with chronic HCV genotype 1 b infection [correction of interferon]. Hepatology 1999; 29: 897–903.
Pluznik D, Butrus SI . Hepatitis C-associated peripheral corneal ulceration. Cornea 2001; 20: 888–889.
Naacke H, Borderie V, Touzeau O, Bourcier T, Scat Y, Laroche L . Marginal corneal perforation associated with herpes simplex virus in a patient with essential cutaneous porphyria. J Fr Ophtalmol 2000; 23: 699–702.
Sangwan VS, Zafirakis P, Foster S . Mooren's ulcer: current concepts in management. Indian J Ophthalmol 1997; 45: 7–17.
Kanai K, Iwata K, Nakao K, Kako M, Okamoto H . Suppression of hepatitis C virus RNA by interferon-alfa. Lancet 1990; 336: 245.
Davis GL, Balart LA, Schiff ER, Lindsay K, Bodenheimer HC Jr, Perrilo RP et al. Treatment of chronic hepatitis with recombinant interferon alfa. A multicenter randomized, controlled trial. N Engl J Med 1989; 321: 1501–1506.
Schvacez R, Weiland O, Wejstal R, Norkans G, Fryden A, Foberg U . A randomized controlled open study of interferon alpha-2b treatment of chronic non-A, non-B posttransfusion hepatitis: no correlation of outcome to presence of hepatitis C virus antibodies. Scand J Infect Dis 1989; 21: 617–625.
Lambiase L, Davis GL . Treatment of chronic hepatitis. Gastroentrol Clin N Am 1992; 21: 659–677.
Tang E . Hepatitis C virus. A review. West J Med 1991; 155: 164–168.
Feucht H, Polywka S, Zollner B, Laufs R . Greater amount of HCV-RNA in tear compared to blood. Microbiol Immunol 1994; 38: 157–158.
Houghton M, Weiner A, Han J, Kuo G, Choo QL . Molecular biology of the hepatitis C virus: implications of diagnosis, development and control of viral diseases. Hepatology 1991; 14: 381–388.
Zegans ME, Srinivasan M, McHugh T, Whitcher JP, Margolis TP, Lietman T et al. Mooren's ulcer in south India: serology and clinical risk factors. Am J Ophthalmol 1999; 128(2): 205–210.
Leyland M, Torok ME, Acheson, Foster GR . Hepatitis C virus infection is not associated with a marked increase in the prevalence of ophthalmic morbidity. Eye 2000; 14: 889–891.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jain, A., Sukhija, J., Saini, J. et al. Hepatitis C virus-associated keratitis. Eye 18, 131–134 (2004). https://doi.org/10.1038/sj.eye.6700604
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700604
Keywords
This article is cited by
-
Extrahepatic Manifestations of Hepatitis C Virus Infection: Mixed Cryoglobulinemia and Beyond
Current Hepatitis Reports (2011)
-
Chronic hepatitis C virus infection is not associated with Mooren's ulcer
Eye (2008)
-
Hepatitis C as a systemic disease: virus and host immunologic responses underlie hepatic and extrahepatic manifestations
Journal of Gastroenterology (2007)