Abstract
Purpose Pigment dispersion syndrome (PDS) is a well-described entity with Krukenberg's spindle, heavy trabecular pigmentation and retroilluminating iris defects. We have observed a group of patients in mesoendemic onchocercal communities of Kaduna State, Nigeria, with significant amounts of free-floating melanin in the anterior chamber, normal angle pigmentation and absence of iris defects. A pseudo-Krukenberg spindle forms when the patients are asked to maintain a 2 min head-down posture as is often done when examining eyes for the presence of anterior chamber microfilaria. This spindle gradually disappears (tumbles back) after about 2 min of return to the erect posture. This paper describes this finding, which does not appear to fit into accepted notions of pigment dispersion.
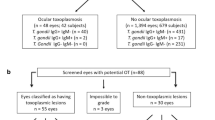
Methods As part of the seventh annual ivermectin dosing exercise during which evidence of optic nerve damage was sought, 455 patients were examined for the presence of microfilaria in the anterior chamber. A total of 352 had been selected for signs of optic nerve disease during an earlier screening exercise, while 103 belonged to a random sample of 5 years and above. Signs of onchocerciasis were sought, while gonioscopy and intraocular pressure measurements were carried out.
Results Of the 455 (11%) individuals examined, 53 demonstrated this phenomenon. Within the random sample, the prevalence was 20%. These tumbling Krukenberg positive (TK+) individuals are significantly younger than TK− individuals and the prevalence, highest in the first decade, dropped steadily to zero levels over the age of 75. Sex distribution was about equal. There was no difference in intraocular pressure, cup–disc ratio and angle pigmentation. Distributions of sclerosing keratitis and chorioretinitis were not statistically different. Optic nerve disease was more common in TK− but this was attributable to the older age distribution. Five TK+ were re-examined after a period of 7 years and had not developed PDS or glaucoma. Four of the five remained TK+. A familial tendency was noted and hereditary factors may be at play, possibly autosomal recessive. The same phenomenon was noted in two of 44 patients in an ophthalmic clinic in Abuja, Nigeria, an urban, non-endemic city south of Kaduna.
Conclusions This phenomenon does not fit into accepted notions of PDS and may well be a normal finding.
Similar content being viewed by others
Introduction
The presence of excess melanin deposits in the anterior chamber of the eye is most commonly associated with a diagnosis of pigment dispersion syndrome (PDS).1,2 Duke-Elder and Thommy have reported isolated large free-floating pigmented particles in a few individual cases (PDS).3,4 In the setting of a community-based trial of ivermectin for onchocerciasis in Kaduna State, Nigeria, we had cause to examine a sample of individuals aged 5 years and above in populations mesoendemic for onchocerciasis. The head-down posture is generally assumed in surveys for ocular microfilaria because this enhances visibility of anterior chamber microfilaria.5
During the course of the study, we observed that a proportion of patients had free-floating melanin in their anterior chambers made evident by the head-down posture. Having made this observation, we subsequently quantified this finding at the time of a repeat examination and dosing. This paper presents our findings.
Methods
Annual dosing with ivermectin of communities mesoendemic for onchocerciasis in Kaduna State of Northern Nigeria has been instituted for over 10 years. These communities were selected on the basis that they had skin snip positivity rates of over 70%. Details of methodology are discussed in an earlier paper.6 During the seventh annual dosing, 455 individuals within these communities were examined for, among other things, the presence of microfilaria in the anterior chamber. The 455 individuals included subjects who on the basis of a screening exercise had signs to suggest the presence of optic nerve disease (352),6 and a random sample of subjects 10 years and older (103). This examination necessitated the maintenance of a 2 min head-down posture to enhance visibility of microfilaria. The presence of free melanin particles was noted at the same time. Other signs of PDS, namely iris transillumination and the presence of a Krukenberg spindle were then sought. Intraocular pressure measurements and gonioscopy were undertaken prior to dilated fundoscopy. Records of gonioscopy and intraocular pressure measurements were available for 286 of the total group examined at the seventh dosing. A similar examination of 44 patients attending a clinic in Abuja, the non-onchoendemic urban capital of Nigeria 200 km south of Kaduna, was undertaken. Data were entered into a precoded form, transferred into a D-Base III format, and analysed using EPI-info version 5.
Tumbling Krukenberg
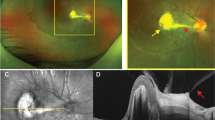
We have termed the observation made in this community ‘Tumbling Krukenberg’ (TK) since this most clearly describes the phenomenon. On examination of the anterior segment after adoption of the prone head posture for 2 min, free-floating melanin particles (of similar size to those seen fixed to the corneal endothelium in Krukenberg spindle) are observed adjacent to the endothelial surface of the cornea. Just like a Krukenberg spindle, they form a vertical pattern. Unlike a Krukenberg spindle, however, they fall out of position and disappear back into the inferior angle over about 2 min following assumption of the vertical posture on the slit lamp. Gonioscopy reveals the melanin particles as a brownish powdery dusting in the inferior angle but the remainder of the drainage angle is not heavily pigmented. Those who manifested this phenomenon are referred to as TK+ in this communication. Those who did not manifest this phenomenon are classified as TK−. This phenomenon is illustrated in Figure 1.
Results
Of the 455 individuals 43 (11%) were identified as TK+ (26 males, 27 females). However, 21 of 103 in the random sample (20%) were TK+. This implies that the prevalence in the general population in these communities is about one in five. The random sample was significantly younger than the general sample population (mean age 36.1 vs 48.5 years, P<0.0001). Of the 53 cases identified in total, 24 were bilateral, 15 were affected in the right eye only and eight in the left eye only. The laterality of the finding was not recorded in 4 cases.
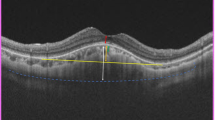
There was no evidence that these melanin particles were fixed to the endothelium or any other contiguous structure such as the lens or iris. There was no evidence of trans-illumination. TK+ individuals were significantly younger than TK− (mean age 35.3 vs 44.9 years, P=0.002). This difference was maintained when the analysis was limited to the random sample (26.4 vs 37.8 years, P<0.05). The age distribution also indicated that the prevalence of tumbling was highest in the 10–20 age group (32%), and this dropped and remained relatively constant at about 8.5% prevalence in the 30 to 70-year bracket, and then dropped to zero above the age of 75 (Figure 2). Mean intraocular pressure for TK+ and TK− was similar being 13.6 and 13.6 mmHg respectively (Student's t-test, P=0.918). There was also no notable difference in the cup/disc ratios (TK− 0.33, TK+ 0.28, Student's t-test, P=0.06).
Gonioscopic findings
The melanin granules were gonioscopically visible in the inferior angles in TK+ as a powdery dusting. TK+ individuals tended to have steeper angles on a semi-quantitative scale designed for the study (P=0.003) but more meshwork visibility (P<0.001). Most of the angles seen in the study were lightly pigmented and there was no significant difference in the distribution of angle pigmentation between the two groups. Importantly, 9.7% of TK+ had heavy pigmentation compared with 9.4% of TK− (χ2=0.85, df=3, P=0.84) (Table 1).
Onchocercal eye disease
Skin snip positivity in TK− was 78% and lower at 61% in TK+, but this is not statistically significant (χ2=3.02, P=0.82). The presence and degree of peripheral anterior synechia (PAS) was similar in the two groups (27% in TK−, 16% in TK+, χ2=2.43, P=0.6). A higher proportion of TK− had optic nerve disease (73 vs 50%, odds ratio 2.75 (1.21–6.19 95% CI) but this difference was age related. Using the right eye as sentinel and analysing 433 cases in which data are available, sclerosing keratitis (SK) was present in 39 of 394 TK− (9.9%) and in only two of 39 TK+ (5.2%); this difference, though not significant (P=0.25, Fisher's exact one-tailed test), may again be age related. Similarly, there was no difference between the groups for the presence of onchocercal chorioretinitis (27.5 vs 41.0%, P=0.097, Mantel Henzel χ2=2.75).
Follow-up
During the first annual dosing, the observation was recorded in 18 individuals. Seven years later, five of this group of 18 were re-examined. Four of these still demonstrated bilateral tumbling phenomenon, as was the case at initial examination. These were aged 10, 13, 20 and 27 respectively at first examination. The only individual who did not demonstrate tumbling at the second examination was aged 65 at first examination and 72 at second examination. There was no evidence of glaucomatous disease with the cup–disc (CD) ratios all being normal (all had CD ratios <0.4, including the 65-year-old subject) and normal Friedman central visual fields. There was in addition no evidence of PDS.
Familial clustering
There was evidence of familial clustering. Three affected individuals aged 16, 20 and 24 with the same father and mother were seen during the first dosing. Both parents were examined and were phenotypicaly normal, there was no evidence of pigment dispersion and the intraocular pressures were normal. This would suggest that if heredity was involved, it would likely be autosomal recessive with no X-linkage, as both sexes are equally affected. There were two other groups of three relatives from the same compound, and four groups of two from the same compound. One of the latter group of two affected relatives had the same father, and possibly the same mother, although this cannot be confirmed from our records.
Findings in Abuja
A total of 44 patients aged 10–70 years, mean 29.2 years, 24 male, 20 female, attending a routine ophthalmology clinic in Abuja were examined in a similar fashion and two demonstrated the same phenomenon. One was a 10-year-old boy and the other a 23-year-old female, both with bilateral TK spindles.
Discussion
The liberation of free melanin particles into the anterior chamber has been reported in the past with the use of 10% phenylephrine hydrochloride solution for dilation. 7 This is not the case of the finding in our cases. All observations were made prior to dilation. Besides, the age distribution of melanin liberation from topical mydriatics is opposite to our experience, being highest in the older groups.7 We believe this to be the first report fully detailing this phenomenon. Is this a finding peculiar to our population, related to pathology or a normal finding in individuals with dark irides?
This phenomenon of free pigment dispersion appears to be unrelated to onchocercal infection. There was no difference between TK+ and TK− individuals with regard to prevalence of skin snip positivity or of onchocerciasis-related lesions. In addition, the fact that the same phenomenon was demonstrable in an Abuja cohort in a nononcho-endemic setting clearly suggests that this is not necessarily oncho-related. The frequency of the finding in Abuja (4.5%) is much lower than would be expected for that average age group of 30 years. This could be a result of to selection bias in the clinic, hereditary or other factors.
Kristensen observed that pigment liberation occur-ring after mydriasis was accompanied by a temporary intra-ocular pressure rise and recommended this mydriatic test as a ‘provocative test’ for normal tension glaucoma patients.8 Patients with clinical PDS are reported more likely to have free aqueous melanin granules.9 Are those who are TK+ likely to develop glaucoma or classical PDS later on in life? Five individuals exhibiting the phenomenon at first examination were re-examined 7 years later and the same physical sign was still present in all except the most elderly. None showed any evidence of glaucomatous disease or of PDS.
One of the reviewers of our paper pointed out that, in contrast to classical PDS where the melanin granules are derived from the iris pigment epithelium, the melanin granules in the TK− syndrome might be released from iris stroma melanocytes. These granules are ‘smaller in size and more brownish than iris pigment epithelium granules. This difference in pathogenesis might explain the different clinical picture' seen in our patients.
In summary, we have described the occurrence of free melanin particles in the anterior chamber in a proportion of subjects examined for anterior chamber microfilaria in African eyes both in an onchocercal mesoendemic and nonendemic setting. The evidence does not suggest that the lesions are related directly to onchocerciasis and individuals do not show evidence of classical pigment dispersion or glaucomatous disease after follow-up for 7 years. This may be a benign physiological phenomenon with a hereditary component.
References
Ritch R . Editorial: pigment dispersion syndrome. Am J Ophthalmol 1998; 126(3): 442–445(review).
Ritch R . A unification hypothesis of pigment dispersion syndrome. Trans Am Ophthalmol Soc 1996; 94: 381–405.
Duke-Elder S . System of Opthalmology, Vol. III, Part 2. Henry Kimpton; London, 1964, pp 547–548.
Thommy CP . Free pigmented bodies in the anterior chamber. Indian J Ophthalmol 1980; 28(3): 139–140.
Taylor HR . In: Clinical Ophthalmology, Vol. 5(62). Harper & Row Publishers: Philadelphia, 1985, p 5.
Cousens SN, Cassels-Brown A, Murdoch IE, Babalola DE, Jatau D, Alexander NDE et al. Impact of annual dosing with Ivermectin on progression of onchocercal visual loss. Bull World Health Organ 1997; 75: 229–236.
Aggarwal JL, Beveridge B . Liberation of iris pigment in the anterior chamber after instillation of 10% phenylephrine hydrochloride solution. Brit J Ophthalmol 1971; 55: 544–549.
Kristensen P . Pigment liberation test in low-tension glaucoma. Acta Opthalmol 1967; 45: 594–600.
Kuchle M, Mardin CY, Nguen NX, Martus P, Naumann GO . Quantification of aqueous melanin granules in primary pigment dispersion syndrome. Am J Ophthalmol 1998; 126(3): 425–431.
Acknowledgements
The field work was carried out within the Kaduna Collaboration for Research on Onchocerciasis and received financial support from the UNDP/World Bank/WHO Special Programme for Research and Training in Tropical Diseases ID 890456, the Leverhulme Trust, and the Royal Commonwealth Society for the Blind. Principal investigators on the research were Prof. (Mrs) Adenike Abiose and Prof. Barrie R Jones. The untiring work of the whole field team, the logistical support team and the data processing group under the leadership of Mr Simon Cousens is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Babalola, O., Murdoch, I. Free-floating melanin particles in the anterior chamber: a normal finding in African eyes?. Eye 17, 410–414 (2003). https://doi.org/10.1038/sj.eye.6700349
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700349