Abstract
Purpose This national study was designed to audit anatomical outcome and complications relating to primary surgery for rhegmatogenous retinal detachments. This paper presents survey methods, characteristics of participating consultants and the demographic and clinical characteristics of the patient sample.
Methods Two surveys were undertaken. The first identified consultants who at the time performed retinal detachment surgery in the National Health Service. These surgeons formed the sampling frame for a nationwide cross-sectional clinical study that audited the outcomes of primary surgery for rhegmatogenous retinal detachments. Consultants selected patients according to the study eligibility criteria and data were collected by self-administered postal questionnaires. A validation exercise was carried out to examine selection bias and reporting accuracy.
Results Only 256/671 (38%) of UK consultants, who responded to the first survey, indicated that they performed retinal detachment surgery on NHS patients. Annual activity varied between 0 and 400 primary procedures for rhegmatogenous retinal detachments. Seven hundred and sixty-eight eligible patients from 167 consultants were recruited for the clinical study. Twenty per cent of patients had a single retinal break with less than one quadrant of associated detachment and 45% had single or multiple breaks within the same quadrant and/or less than two quadrants of associated retinal detachment. Over 50% patients had single or multiple horseshoe tears. Validation studies suggested that there was no significant bias from the selection of patients or inaccuracy in reporting outcomes.
Conclusions This large unselected group of primary rhegmatogenous retinal detachments provides a representative sample for considering variations in re-attachment rates.
Similar content being viewed by others
Introduction
Critical examination of clinical outcomes in the context of clinical governance has a high profile in medical practice and politics.1,2 When considering the production of clinical guidelines for the management of rhegmatogenous retinal detachments, the Royal College of Ophthalmologists identified that there was insufficient information on national practices and outcomes of surgery for retinal detachment repair in the United Kingdom (UK).
This study was therefore designed to audit the outcome of surgery for primary rhegmatogenous retinal detachment, including success and complication rates, and to provide baseline information on current practices of retinal detachment surgery from a nationally representative sample of patients.
This paper reports the study methods, characteristics of participating consultants and the demographic and clinical characteristics of the patient sample. The following paper reports clinical outcomes.3
Methods
All UK consultant ophthalmologists were invited to participate in the study. A preliminary questionnaire, to identify and characterise consultants who undertook retinal detachment surgery on National Health Service (NHS) patients in the UK, was distributed in November 1997. Those who indicated that they currently performed retinal detachment surgery on NHS patients were subsequently invited to participate in a survey of clinical practice.
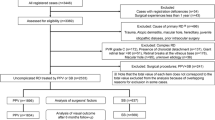
The clinical part of the study was a retrospective nation-wide cross-sectional survey. A cross-sectional design allowed small numbers of patients to be used from each surgeon, maximising response rate. Data were collected retrospectively to avoid inducing any change of practice that might result from knowledge of participating in the study. All clinical data were collected by a single questionnaire. Consultants were asked to review their operating theatre diaries and to select the most recent patients undergoing their first surgical procedure for rhegmatogenous retinal detachment before 1st October 1997. Consultants with a self-declared special interest in retinal surgery were asked to select their last six consecutive patients, and those consultants without a special interest, their last four consecutive patients. Patients with rhegmatogenous retinal detachments following penetrating eye injury, complicating a tractional retinal detachment or secondary to a macular hole and those who had previously undergone other posterior segment surgery were not eligible for inclusion in the study. The main clinical outcome measure was complete anatomical re-attachment at 3 months after the initial procedure and secondary outcome measures included complications relating to surgery. Complications were defined as any clinical event that had been reported in the clinical notes, either per-operatively, within 1 month (early) or between 1 and 3 months (late).
Audit standards were set for the outcomes of interest before the study commenced and were based on published evidence in conjunction with clinical experience.4,5,6,7,8,9,10,11,12,13,14 The minimum acceptable standards that the steering committee felt should be achieved are presented in Table 1.
In order to allow for case-mix a four-point grading system based on clinical features of the retinal detachment was devised by the steering committee (Table 2). One researcher (JAT), masked to surgeon and outcomes, graded all detachments.
Following piloting, data were collected using paper questionnaires. These were self-completed by participating surgeons. All data were kept in accordance with the Data Protection Act, with patients and consultants confidentiality maintained. Data were double entered and stored on a customised database and analysed using Stata Statistical Software: Release 5.0.
For the purposes of the analyses, a specialist was defined as a consultant with a self-declared special interest in retinal surgery and who also performed pars plana vitrectomy. The remaining consultants were defined as non-specialists. Multi-variate analysis was performed in order to identify predictors of successful anatomical outcome using the following variables; specialist status, grade of detachment, the presence of a high risk factor pre-operatively, type of surgery, break type and the timing of surgery from presentation. Associations between explanatory variables and outcome measures were measured using logistic regression, with statistical significance at P < 0.05. All analyses were adjusted for the cluster effect of sampling multiple patients from the same consultant.
A telephone survey of consultants who did not respond to the preliminary questionnaire was undertaken. Fifty per cent of the non-responders were randomly selected and up to four attempts were made to contact them by telephone to determine whether they operated on retinal detachments.
A validation study was undertaken to exclude significant bias in patient selection or the reporting of results by consultants. After the clinical questionnaires had been received, hospitals that had participated were divided into two groups, those with at least one surgeon with a special interest in retinal surgery (50 hospitals) and those without (44 hospitals). Five hospitals were randomly selected from each group. All consultants were contacted individually and their permission sought to include their patients in the validation sample. The principle investigator (JAT) visited each unit. Before the visit, each unit was asked to identify an individual to provide the hospital records of patients included in the study and those of other patients undergoing retinal detachment procedures at the same time. This latter group was identified from the theatre diary using local clerical support and checked during the visit.
To assess the accuracy of data reporting, 13/43 (30%) data items from the original questionnaire were selected and during the visit the principle investigator reviewed the clinical notes and recorded the data items on a prepared proforma, masked to the information supplied by consultants in the original questionnaire. Reporting accuracy was assessed by comparing the number of discrepancies between the original questionnaires and the proformas completed during the validation visit. The accuracy of patient selection was assessed by examining the notes of excluded patients undergoing detachment surgery during the same time period as patients included in the study, identified from the operating theatre diaries.
Results
Preliminary questionnaire response rates
The response rate to the preliminary questionnaire was 93% (671/722). Of the respondents, 38% (256/671) indicated that they currently performed retinal detachment surgery, 35% (233/671) that they had once performed detachment surgery as a consultant but now had ceased and 24% (164/671) that they had never performed detachment surgery as a consultant.
Twenty-seven of the 51 non-responders to the preliminary questionnaire were randomly selected for a non-responder survey. No response was obtained from five and two consultants had retired. Of the remaining 20, 16 did not perform detachment surgery and four did. This suggested that detachment surgeons were not underrepresented in the responders to the preliminary questionnaire.
Profile of current detachment surgeons
One hundred and five consultants declared a special interest in retinal surgery. Of these 93 performed pars plana vitrectomy and were defined as specialists for the analyses.
The number of surgical procedures to repair primary rhegmatogenous retinal detachments that surgeons performed annually, varied widely in both the specialist and non-specialist groups. The reported number of primary retinal detachments performed in 1996 by the consultants responding to the preliminary questionnaire varied between 2 and 400 (median = 70, mean = 90.6, 95% CI = 73.5–107.2, n = 91) for specialists and 0 and 50 (median = 5, mean 7.1, 95% CI = 5.9–8.2, n = 150) for non-specialists. From the reported activity by participating consultants and the response rates, the projected number of primary detachments performed annually in the UK was 10 276 (95% CI = 10094–10458).
Routine audit of the results of retinal detachment surgery was not universal. Only 70% (64/91) specialists and 46% (71/154) non-specialists routinely audited their surgical results.
The majority of surgeons had access to operating theatres to perform retinal detachment surgery outside normal working hours, but nearly 9% of specialists (8/91) and 7% of non-specialists (11/154) did not.
Clinical questionnaire response rates
Clinical questionnaires were sent in April 1998 to the 256 consultants who had been identified by the preliminary questionnaire. A response was obtained from 78% (200/256) consultants from this group. Eight consultants declined to participate in the study. Eighteen consultants had not operated on any patients in the year to 30th September 1997, although they had answered in the affirmative in the preliminary questionnaire. Clinical data were received from 167 consultants (72 specialists and 95 non-specialists) on 768 eligible patients. The adjusted response rate taking into account the consultants who indicated that they had no eligible patients was 70.4% (167/237).
Patient profile
The patients’ ages ranged from 9 to 89 years (median 61). The right eye was involved in 50% (385/768) cases. Twenty percent (152/753, missing data = 15) of eyes had undergone previous cataract extraction, and the majority were pseudophakic (83%, 126/152). In 54% (409/757, missing data = 11) the macula was detached pre-operatively. The proportions of cases by type of break are given in Table 3, and by grade of detachment in Table 4.
Validation
The sample consisted of 20 consultants, 13 non-specialists and seven specialists. All consultants contacted consented to the inclusion of their patients in the validation study. As in one department it was not possible to retrieve notes, the validation sample represented 9.6% (74/768) of the study sample. The notes of 93.2% (70/74) of this group were examined. The remainder could not be found. Six out of 70 patients (8.6%) had been incorrectly included. Comparing the retinal outcome, 5/6 had the same outcome as the incorrectly excluded patient they had replaced. The maximum number of errors on any questionnaire was three out 13 variables, noted in 11% of questionnaires examined. Of the remainder, 26% had no incorrectly reported variables, 40% had one incorrectly reported variable and 21% had two.
Discussion
The response rates of 93% to the preliminary questionnaire and 70% for the clinical questionnaire are in line with previous national audits.15,16,17 The non-response study showed that detachment surgeons were not underrepresented in the sample. The validation study established that there was no significant selection bias when patients were considered for inclusion by the participating clinician and that there was no significant inaccuracy when completing the clinical questionnaires.
The study design was necessarily retrospective to avoid inducing a change of practice by conducting the study. A prospective audit would have had the advantage of specifying in advance what data were collected on each patient, and standardising the collection and assessment methods. Because of the reliance on the contemporaneous clinical notes, it was inevitable that for some patients data were incomplete.
Visual acuity was not included as a main outcome measure for two reasons. First the study was conducted over a short time period (visual function continues to improve for many months after detachment surgery18) and second, the retrospective nature of the study, preferred in order to avoid inducing a change of practice, meant that it was not possible to standardise the methods for measuring acuity pre- or post-operatively. In addition it would not have been possible to adjust consistently for co-existing ocular pathology (lens opacities or macular dysfunction) that would have a bearing on visual outcome. These methodological issues prevent robust evaluation of visual outcome by this study.
The calculated figures for annual detachments show that specialists perform the vast majority of detachment surgery. Though this figure is an estimate, based on operating levels for 1996, it suggests that the survey sampled over 8% of all detachments performed annually by the participating consultants. However the audit only sampled 5.2% of the workload of specialists while auditing 33.4% of the workload of non-specialists.
The reported levels of routine local or individual audit by clinicians of retinal detachment surgery outcome were disappointing. It is hoped that the publication of these national clinical outcomes will stimulate regular local audit by providing relevant benchmarks against which clinicians can judge their performance.
In conclusion, the findings of the national audit outcome of primary surgery for rhegmatogenous retinal detachment are based on a large representative sample of patients undergoing detachment surgery from a broad spectrum of UK consultant ophthalmologists.
References
Department of Health. The New NHS. Modern. Dependable HMSO 1997
Department of Health. A First Class Service HMSO 1998
Thompson JA, Snead MP, Billington BM, Barrie T, Thompson JR, Sparrow JM . National audit of the outcome of primary surgery for rhegmatogenous retinal detachment. II. Clinical Outcomes. Eye 2002; 16: 771–777
Chignell AH, Fison LG, Davies EWG, Hartley RE, Gundry MF . Failure in retinal detachment surgery. Br J Ophthalmol 1973; 57: 525–530
Rachel WF, Burton TC . Changing concepts of failure after retinal detachment surgery. Arch Ophthalmol 1979; 97: 480–483
Hilton GF, Grizzard WS, Avins LR, Heilbron DC . The drainage of subretinal fluid: a randomised controlled clinical trial. Retina 1981; 1: 271–280
Wilkinson CP, Bradford RH . Complications of draining subretinal fluid. Retina 1984; 4: 1–4
McAllister IL, Meyers SM, Zegarra H, Gutman FA, Zakov ZN, Beck GJ . Comparison of pneumatic retinopexy with alternative surgical techniques. Ophthalmology 1988; 95: 877–883
Tournambe P, Hilton G . Pneumatic retinopexy. A multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. The Retinal Detachment Study Group. Ophthalmology 1989; 96: 772–783
Little BC, Inglesby DV, Wong D, Chignell AH . Results and complications of conventional repair of bullous retinal detachment using posterior segment air injection. Eye 1990; 4: 222–225
Wong D, Chignell AH, Inglesby DV, Little BC, Franks W . The treatment of bullous rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol 1992; 230: 218–220
Gartry DS, Chignell AH, Franks WA, Wong D . Pars plana vitrectomy for the treatment of rhegmatogenous retinal detachment uncomplicated by advanced proliferative vitreoretinopathy. Br J Ophthalmol 1993; 77: 199–203
Hakin KN, Lavin MJ, Leaver PK . Primary vitrectomy for rhegmatogenous retinal detachment. Graefes Arch Clin Exp Ophthalmol 1993; 231: 344–346
Sharma T, Challa JK, Ravishankar KV . Scleral buckling for retinal detachment. Predictors for anatomic failure. Retina 1994; 14: 338–343
Desai P . The national cataract surgery survey: I. Method and descriptive features. Eye 1992; 6: 487–492
Bailey CC, Sparrow JM, Grey RHB, Cheng H . The National Diabetic Retinopathy Laser Treatment Audit. I. Maculopathy. Eye 1998; 12: 69–76
Edmunds B, Thompson JR, Salmon JF, Wormald RP . The National Survey of Trabeculectomy. I. Sample and Methods. Eye 1999; 13: 524–530
Burton TC . Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc 1982; 80: 475–497
Acknowledgements
The authors would like to thank all the consultants who participated in both phases of the audit without whose support the study would not have been possible. They would like to thank Mr AH Chignell and Mr B Foot for participating in the steering committee; Mr AT Moore as past chairman of the audit committee; Miss M Hallendorff and the staff of the Royal College of Ophthalmologists and Mr CR Canning and Mr A Chopdar for piloting the clinical questionnaires.
This study was supported by core audit funding from the Department of Health. Presented in part at the Oxford Ophthalmological Congress 1998. Financial/proprietary interest: None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thompson, J., Snead, M., Billington, B. et al. National audit of the outcome of primary surgery for rhegmatogenous retinal detachment. I. Sample and methods. Eye 16, 766–770 (2002). https://doi.org/10.1038/sj.eye.6700324
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700324
Keywords
This article is cited by
-
Buckle-related complications following surgical repair of retinal dialysis
Eye (2008)
-
How effective is macula-off retinal detachment surgery. Might good outcome be predicted?
Eye (2007)
-
Retinal detachment following surgery for congenital cataract: presentation and outcomes
Eye (2005)
-
Clinical features and surgical management of retinal detachment secondary to round retinal holes
Eye (2005)
-
Retinal detachment in south India—presentation and treatment outcomes
Graefe's Archive for Clinical and Experimental Ophthalmology (2005)