Abstract
The prevalence of reactions against natural rubber latex (NRL) is thought to be increasing in both the general public and healthcare workers. These can vary from mild benign skin reactions to bronchospasm, anaphylactic shock, and death. Difficulties exist for ophthalmic departments wishing to establish protocols in providing ‘latex-free environments’ for patients undergoing cataract surgery. Currently no legislation exists regarding the labelling of NRL-containing products in the United Kingdom with information on a product's NRL content provided by the manufacturer on a voluntary basis only. It is hoped this review article will act as a basic guide in the management of NRL-sensitive patients undergoing cataract surgery in the United Kingdom.
Similar content being viewed by others
Introduction
Although it is over 70 years since allergic reactions to natural rubber latex (NRL) were first described,1 a dramatic rise in the number of reported cases has occurred over the past two decades. The majority of these reported cases have occurred in industrialised countries, and although it is well known that certain groups of patients have a higher risk of latex allergy, for example, children with spina bifida, it is believed that the frequency of NRL-induced reactions is increasing in the general population. Reports range from mild mechanical irritant reactions to life-threatening episodes caused by immediate IgE-mediated anaphylactic shock. Currently, no curative measures to eliminate hypersensitivity to NRL proteins exist. All current treatment options revolve around measures to reduce exposure to NRL proteins.2
In July 2001, the authors were involved in the management of patients undergoing cataract surgery who were known to be NRL sensitive. We discovered that not only did our hospital not have a formal management plan for NRL-sensitive patients undergoing cataract surgery, but also that our department was not alone, and a brief telephone survey of the theatre sisters of other ophthalmic units revealed a similar situation. Not only were these ophthalmology departments lacking a formal protocol of action, but there was also a general lack of awareness amongst ophthalmologists and ophthalmology nurses to the scale of the problem.
A MEDLINE and EMBASE literature review highlighted several review articles that describe the magnitude of the problem and basic science behind NRL reactions. In addition, many subspecialties, in particular dentistry, anaesthesia and otolaryngology, have provided review articles, which act as frameworks for the management of NRL-related problems within their specific subspecialty. There have been no similar articles specific to cataract surgery as yet. It is hoped that this article will help to address this.
Case report
An 80-year-old woman attended cataract assessment clinic. Her significant past medical history included hospital attendance at a dermatology outpatient clinic for a non-healing venous calf ulcer. Examination confirmed visually significant cataracts for which she was listed for surgery.
On the day of surgery, the patient mentioned that she had a ‘rubber allergy’ that had been diagnosed by the dermatologist. Although she had declared this at the preassessment clinic a fortnight earlier, there had been no change in the course of management of the patient.
It was realised that during the cataract operation, the patient would encounter multiple types of synthetic/natural types of plastic or rubber—the exact constituents of these were unknown. Several factors were unknown:
-
What was the exact allergen to which the patient was sensitive?
-
Whether or not she would be exposed to the allergen?
-
If exposure was inevitable, what was the ‘dose’ of exposure? Was this dose of exposure significant?
-
How sensitive would the patient be if she were exposed to the allergen? That is, what would be the nature/magnitude of hypersensitivity response if significant exposure of allergen occurred?
Surgery was deferred until these questions could be answered.
It was later discovered that this lady had attended the vascular surgery outpatient clinic at another hospital for a non-healing skin ulcer overlying her left calf, which had been managed unsuccessfully as a mixed arterial and venous ulcer. Its treatment consisted of regular pressure dressings, which were replaced weekly by a community nurse. She was eventually referred to a dermatologist for a second opinion and was diagnosed with localised dermatitis. Skin patch testing showed sensitivity to thiuram (rubber) and wool alcohol, and it was advised that all contact with latex be avoided, including the use of both latex-free dressings and gloves when dressing the ulcer. The ulcer promptly healed.
The cataract operation was performed two months later in a ‘latex-free environment’ (see later) without complications. Unaided visual acuity was 6/9, improving to 6/6 with a small mixed astigmatic correction and she was discharged.
Discussion
What is latex? The term latex has several meanings depending on the context in which it is used. Its definition is necessary to avoid confusion.
-
Natural rubber latex is the term used to describe the milk-like sap, which is derived from over 2000 species of plants. The most commercially used species is the common rubber tree Hevea brasiliensis.
-
Synthetic rubber is manufactured from oil-based products and is made of multiple synthetic polymers.
-
When the term latex is used generically, it refers to rubber-like compounds and therefore includes both synthetic rubber and NRL-based products.
-
Even more confusingly, medical and scientific articles that use the term to describe a suspension of particles within a liquid, even though the particles themselves are not made of NRL-based compounds or synthetic rubber, for example, latex dyes.
Epidemiology
Natural rubber latex has been in use for over 100 years. It is now estimated that it is found in over 40 000 products. Although the first allergic reaction to NRL was described over 70 years ago, recently there has been a heightened awareness of the problem. This is particularly so in subspecialties that have had to cope with the most dangerous of complications, for example, hypotension and sudden anaphylactic shock, airway obstruction and asthma. In the USA, there have been at least 220 cases of anaphylaxis due to latex exposure.3 The sensitisation of patients to NRL is thought to occur with repeated exposure to NRL proteins, for example, those patients who undergo multiple surgical procedures. The increased incidence of NRL allergy in certain high-risk groups can be explained by the associated increased exposure to NRL allergens. For example, it has been shown that the risk of latex allergy in a child with spina bifida increases with the number of operations performed on that child.4 It is therefore understandable that children with spina bifida and multiple orthopaedic problems have a higher incidence of NRL allergy. Consequently, much of the current literature regarding the clinical significance of NRL allergy originates from the subspecialties involved in their care, particularly anaesthetics, intensive therapy unit (ITU) nursing and orthopaedics.5,6,7,8,9,10,11
In addition to high-risk patient groups, there is also an increased incidence of NRL-related allergic reactions and NRL hypersensitivity seen in healthcare workers, for example, dentists, operating nursing staff, accident and emergency staff,12,13,14 and this is thought to be due to increased exposure to NRL allergens within the work environment. There have been several controlled studies to examine the link between NRL allergy and the amount of NRL exposure amongst healthcare workers. Studies on NRL allergy amongst dental students have shown a link with the degree of exposure. First and second year dental students studies showed no evidence of NRL allergy. However, levels of NRL allergy increased with the seniority of the students, with 6% of third year students and 10% of fourth year students respectively being affected. It was concluded that this pattern was due to increasing levels of exposure to NRL allergen as the students progressed through dental school.15
Even in the lower risk general population, there has been a dramatic increase in the number of reports of NRL-induced allergy over the past decade. It is unknown why this should be so, although many researchers have put forward their putative mechanisms:
-
The increasing use of disposable NRL-based gloves for surgical and medical procedures because of the increased awareness of cross infection leads to increased exposure to NRL proteins.16,17,18 Hence the risk of exposure to NRL allergens is higher during hospital attendance.
-
The use of gloves by the food processing industry may lead to the introduction of NRL proteins into the diet and increased exposure.19
-
Some proteins, which cause food allergies, may be cross-reacting with natural rubber latex allergens. Thus patients with allergies to certain foods, for example, chestnut, banana and avocado, may have an increased risk of NRL allergy and vice versa. 20,21,22,23
Extent of NRL-related disease
Many researchers dispute the actual prevalence of NRL allergy. A prevalence estimate by a particular researcher depends very much on the definition of NRL-related allergy and the systems used for confirming the diagnosis by that researcher. These vary from looking for anti-NRL IgE antibodies in serum (1% in operating staff,24 5.4–7.6% in blood donors,25 8.6% in general paediatric population, and 17.3% in high-risk children26), skin patch testing and skin prick testing (11% in healthcare workers27), to screening questionnaires (up to 21.8% in healthcare workers28). Many estimates of prevalence are based on the number of test positives in that population sampled and not on whether there is actual evidence of clinical allergy. Many researchers now believe that the prevalence of latex allergy is actually much lower than the prevalence of NRL protein sensitisation. That is, although a person may show immunological evidence of sensitisation to NRL proteins by having increased IgE levels to NRL, they may not show a clinical allergic reaction on exposure to NRL. Thus, some researchers feel that incidence figures based on scientific methods looking for sensitisation rates, and not actual incidents of allergic reactivity, may be overestimating the incidence of NRL allergy.29,30,31 Similarly, it is argued that a diagnosis based solely on a clinical history of an allergic reaction is inaccurate because it is often nonspecific. For example, many of the reported ‘allergic’ skin reactions may be due to nonspecific irritant dermatitis.31
NRL allergens and their use in diagnosis
NRL contains approximately 240 polypeptides. Approximately 60 are thought to be antigenic. Some of these have now been identified (Hev b 1, Hev b 2, Hev b 3, Hev b 4, Hev b 5, and Hev b 7 (with two variants— 7b and 7c). All of these characterised antigens have been identified in latex gloves.17 In patients who are known to be latex allergic, their sera most commonly contained IgE antibodies to Hev b 2, Hev b 4 and Hev b 7b. There is evidence to suggest that different groups of patients may show different patterns of seropositivity and that this may reflect different patterns/routes of exposure of latex allergens, for example, Hev b 1 is a common allergen in children with spina bifida but not for healthcare workers.32,16 Some of the antigens in NRL are nonspecific to NRL and may be present in other plants. These are frequently enzymes that are present in the H. brasiliensis plant and that are also present in other plants such as endochitinases.33 In vitro diagnostic tests that look for serological evidence of previous exposure NRL must therefore be specific for NRL antigens only. Tests for anti-NRL antigen antibodies can therefore be nonspecific since the patient may produce similar antibodies to the similar epitopes on antigens from different plants, for example, Ficus benjamina.34 Thus, a patient with an allergy to F. benjamina may be tested falsely positive using that test.35 IgE assay systems, which are currently in development include enzyme-linked immunosorbent assay (ELISA),36,25 and radioallergosorbent testing (RAST). It must be stressed that a diagnosis of latex allergy, therefore, is not based on the result on one specific test but on the basis of probability from the results of several factors, that is, history, IgE status and skin patch testing.37,31 The significance of IgE testing remains debatable at present. The IgE result may be falsely positive due to the crossreactivity of antigens in different plants, for example, they may be allergic to kiwi fruit, banana, avocado, etc. Also, different commercially available assays that measure serological status of an individual may disagree, this being due to the different types of anti-NRL IgE being measured.13 In addition, even if a patient's serum does contain IgE, which is specific for antigens that are solely in NRL (ie, no crossreactivity), he may still not show any clinical evidence of allergic reaction on exposure to NRL. This may be due to the differing clinical allergic sensitivities of patients to NRL.
A test of a patient's relative allergic sensitivity to NRL antigens may be made via skin prick in vivo testing. UK dermatologists commonly use skin prick testing using NRL milk or a homogenate of the material in latex gloves. At present, the US Food and Drug Administration (FDA) have yet to give a licence to a H. brasiliensis extract and as such there is not a standard extract for skin prick testing, although many extract variants are being tested.37 The use of recombinant NRL proteins has shed much light on the possible role of crossreaction of plant allergens and may provide a standard extract for in vivo testing in the future.38,39 The disadvantages of in vivo testing include the risk for severe anaphylaxis in the test subject, so full resuscitation facilities must be at hand. Unfortunately, skin prick testing also suffers from reliability and specificity issues. There are reports of false positives in skin prick testing using certain brands of glove extract because of the presence of other constituents.40 Other in vivo tests, which are all based on the responses to NRL allergen challenge, include the NRL glove wearing test (the sensitivity of which is dependent on the test protocol and the latex protein content of the glove41), aeroallergen challenge techniques42 and nasal challenge tests.43,44 At present specificity/sensitivity issues continue to be a problem for patch testing.45
Types of clinical reaction to latex
Clinical reactions to latex can be nonimmunological or immunological (immediate or delayed hypersensitivity).
Nonimmunological reactions are usually comprised of an irritant contact dermatitis with the symptoms of eczema: itching, redness, burning and scaling. They are common in healthcare workers using NRL-based gloves and are thought to arise from the irritant effects of glove powder, which can be caused by chemical or mechanical irritation. Thus testing for NRL hypersensitivity gives negative results. Mechanical irritation is thought to be caused by fine abrasions inflicted by the powder, which manufacturers use to finely coat the gloves. The gloves are supplied with a powdered surface to aid donning. Chemical irritation is thought to arise from the alkaline pH of powdered gloves. The use of powder-free gloves helps minimise both chemical and mechanical irritant reactions.
Immunological reactions to NRL allergens consist of immediate or delayed hypersensitivity type reactions. The term latex allergy describes the frequently more serious immediate-type reactions, which can range from mild urticarial type reactions—with wheals, redness and itching—to intermediate asthmatic and rhinitis type reactions—with breathlessness, profuse discharge of the airway mucosal glands (rhinoconjunctivitis)—to severe anaphylactic shock (hypotension, severe urticaria, bronchospasm). These reactions develop within minutes of exposure to the NRL allergen. Immediate type reactions result from type-I hypersensitivity reactions with the binding of allergens to mast cells via IgE and the release of inflammatory mediators. The uptake of NRL proteins by the immune system can occur via a respiratory route via aeroallergens, by transdermal passage, especially if the barrier function of the skin has been compromised,17 or via a parenteral route.46,47,48
The severity of the immediate type reactions is dependent on the clinical sensitivity of the patient and the dose of allergen challenge. There has been a lot of research into the possible ways of reducing the severity of aeroallergen challenge, since it is this exposure route which is associated with the more severe allergic reactions, with much of this work concentrating on air filter systems and the use of powder-free gloves.49,50,51 Cornstarch, which is used to coat latex gloves, is thought to bind to NRL allergens, thus producing an aeroallergen.52,53 The use of powder-free gloves not only reduces the incidence of nonimmunological reactions but can reduce latex allergic reactions due to aeroallergen exposure.
Type-IV delayed hypersensitivity causes the delayed clinical reactions to NRL, often manifesting as allergic contact eczema resulting from skin exposure. Transdermal entry of various substances in latex, including NRL antigens and accelerators—chemicals used in the manufacture of natural rubber latex—can result in the attraction of inflammatory cells to the area and a delayed reaction, usually within 6–48 h. Accelerators used in surgical glove manufacture include thiurams, mercaptobenzothiazoles (MBT) and carbamates. Thiurams, in particular, have been implicated as major contact sensitisers in NRL gloves, and glove manufacturers have now restricted their use to some extent. This practice has possibly reduced the frequency of delayed hypersensitivity reactions to NRL antigens resulting from exposure to thiuram-containing latex.54 Thiurams themselves can also induce type-IV hypersensitivity reactions and therefore can cause false positive results in in vivo tests that use thiuram-containing latex extract.45
Clinical relevance
NRL hypersensitivity can manifest as clinical problems both to the healthcare worker and to the patient.
Problems for the healthcare worker
All three types of clinical reaction, nonimmunological and immunological (immediate/delayed), have been reported in healthcare workers. There are numerous reports describing skin problems and occupational asthma in theatre nurses, dentists and emergency physicians due to glove-related reactions,55 with the risk of sensitisation to latex being increased with the duration/frequency of latex glove wear56 and in those with a history of atopy.57
Some occupational health studies have shown a dramatic decrease in the prevalence of latex reactions with the introduction of synthetic powderless gloves.58 Although they are generally more expensive than the latex-containing alternatives, it is suggested that it is economically feasible for healthcare trusts to convert to synthetic alternatives. They suggest that a reduction in the associated disability taken as a result of NRL-related problems would compensate for the increased cost of the gloves and recommend that all healthcare centres would benefit financially from conversion to a ‘latex safe’ environment.59
In contrast, other reports suggest that the prevalence of latex sensitivity amongst healthcare workers may be overestimated, such that a trust-wide adoption of latex-free powderless gloves is probably, at present, uncalled for. Page et al60 reported that the occupational use of latex gloves is not a risk factor for sensitisation to latex. In addition to the opinion that widespread conversion to latex-free alternatives is difficult and perhaps unnecessary, many subspecialties, including ophthalmology, require the high degree of sensitivity, flexibility and comfort associated with latex gloves, and feel that these necessary qualities are not provided by certain latex-free alternatives.61,62,63,64 Glove manufacturers produce different claims regarding the differing manufacturing methods/latex protein type and content of their products, ranging from ‘low-allergen’ latex-containing gloves to completely synthetic alternatives. So far there have been few studies that actually compare the allergenic potential of the different brands of gloves or whether or not their introduction is justified in terms of economic costs to the healthcare trusts and morbidity amongst its workers and patients.62,63,64 It is recognised that not only is the amount of NRL antigenic protein important but also the types of antigenic protein within that glove. Thus, some researchers feel that some brands of ‘low-allergen’ latex gloves may have an equivalent allergenic potential because they contain similarly significant sensitising levels of their dominant NRL protein.62 The lack of a consensus, regarding both the role of latex gloves and the prevalence of latex allergy, therefore accounts for the variable conversion to latex-free alternatives by different hospitals.65
Problems for the patient
The patients who are most at risk of serious allergic reactions are those who display a high sensitivity to NRL allergens, which manifests by an immediate type clinical immunological reaction. There have been numerous reports of bronchospasm, respiratory arrest and even death in many surgical subspecialties due to NRL protein exposure, both in high- and normal-risk patients undergoing elective surgery. Latex allergy is now seen by some anaesthetists as a major risk factor to safe general anaesthesia because of a lack of awareness among healthcare workers, the lack of screening facilities for the condition during preassessment, and the potential for unpredictable severe anaphylactic reactions.66,8,9 In addition to severe anaphylaxis, latex also produces milder problems, similar to those experienced by healthcare workers, such as asthma, rhinoconjunctivitis and irritant/allergic eczema.
The differential diagnosis of latex hypersensitivity as a cause for idiopathic complications experienced by patients during hospital admissions is being increasingly considered by subspecialties as awareness increases. Even though many researchers feel the screening for latex allergy, especially for those in high-risk groups undergoing surgery, is a necessary task, the relative nonspecificity of screening questionnaires, combined with the lack of a reliable quick objective screening test, reduces their usefulness at present.
Latex allergy in the patient undergoing cataract surgery
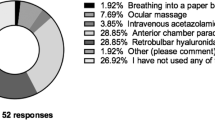
Although, there are no formal audits of the awareness of cataract surgical units for operating on latex-sensitive patients, a brief telephone audit by the authors of several eye operating theatres suggests that latex allergy awareness is fairly low, with either no formal ‘latex-free’ protocol or ‘latex-free’ equipment set aside. Keh et al67 performed a postal questionnaire study of the preparedness of 205 main theatre units in England, Scotland and Wales. Of the 120 units that responded to the study, about two-thirds of them did not have a latex allergy protocol and less than one-third had latex-free equipment set aside. They also reported that of the latex allergic patients who did undergo surgery in these operating theatres, a significant number developed major anaphylactic reactions.
A MEDLINE and EMBASE literature search for latex problems in ophthalmology revealed only a few reports pertaining to natural rubber latex allergy in the ophthalmology literature. Bergwerk and Kodsir68 reported an allergic type bilateral conjunctivitis in a 13-year-old girl, which was associated with the use of the Tonopen. The conjunctivitis resolved after the latex-containing cover of the Tonopen was substituted for a non-latex glove fingertip. Both type-I and type-IV hypersensitivity reactions can arise against natural rubber latex antigens, and although there have been no reports of intraocular pathology secondary to natural rubber latex, it is plausible that sterile postoperative uveitis may develop with the introduction of latex antigens into the eye during cataract surgery.
Despite the fact that problems specific to the eye due to latex hypersensitivity are probably low, it is clear that ophthalmic surgeons should be prepared to operate in a ‘latex-free’ environment to reduce the risk of unpredictable severe anaphylaxis. Because desensitisation of hypersensitive patients using immunotherapy is still in its experimental stages,69,70 the mainstay of management of the latex-allergic patient involves the avoidance/reduction of contact with the allergen.
A management plan to reduce the risk to latex-allergic patients undergoing cataract surgery involves:
-
Identification/diagnosis/screening of all patients at risk
-
Thorough communication to all healthcare workers involved in the care of that patient of the latex allergic status
-
Preparation of the preoperative, perioperative and postoperative care environment to minimise the dose of latex allergen exposure to the patient
-
Education of all healthcare workers to increase awareness of the problem.
Identification/screening of at risk patients
Accurate screening for latex allergy is hindered as a result of the nonspecificity of screening questionnaires and lack of a standardised quick in vitro confirmatory diagnostic test. Often the diagnosis is only made after consultation with other subspecialties, for example, dermatology, respiratory medicine. Patients who have previously been diagnosed as being latex allergic should therefore be informed of their diagnosis and educated about the risks of surgery. Screening questionnaires, although suffering from problems of nonspecificity, may have an important role in helping to identify those patients who may be at risk so that further testing/referral can be implemented. These could be incorporated into the preassessment clinic: 71,72
Children:
-
Lip swelling, mucosal reactions, or asthma after blowing up balloons
-
History of atopic diseases
Adults:
-
Contact urticaria, rhinoconjunctivitis, asthma, or ana-phylaxis after contact with NRL gloves, condoms, or other NRL products
-
Allergic reaction during medical or dental procedures or anaphylaxis during surgical interventions
-
Allergies to food, with special regard to tropical fruits (banana, avocado, papaya and chestnut)
-
History of hand eczema or atopic diseases
Patients identified as being at risk should undergo formal referral to dermatologists or respiratory physicians for more rigorous in vivo/in vitro diagnostic testing.
Thorough communication to all healthcare workers involved in the care of that patient of the latex allergic status
All healthcare workers involved in the chain of care, from the preoperative to postoperative stage, should be notified of all at-risk patients. A robust and explicit system to identify those at risk should operate so that the environment can be adapted to suit them. The authors recommend that patients should be labelled as being latex allergic in a similar manner to that if they were allergic to drugs. Latex allergic patients should ideally be operated on during the same theatre list. The anaesthetist, theatre nurses and postoperative nurses involved should be informed in advance. The patient's latex allergic status should be written on the inpatient identification band.
Preparation of the preoperative, perioperative and postoperative care environment to minimise the dose of latex allergen exposure to the patient
Natural rubber latex is present in many medical products including:
-
Gloves
-
Face masks
-
Mattresses
-
Stethoscopes
-
Blood tourniquets
-
Tubing for blood pressure monitoring
-
Rubber syringe stoppers
-
Medical vial stoppers
-
Anaesthetic laryngeal masks
-
Honan's anaesthetic compression balloons
-
Catheters
-
Sleeves on phacoemulsification tips
The American Academy of Allergy, Asthma, and Immunology and the American College of Allergy, Asthma and Immunology in 1997 produced a joint statement, which recommended that powder-free latex gloves should be used to reduce the amount of aeroallergens in hospital. The field of anaesthesia has led the way in studies to try to reduce the amount of aeroallergens in the operating theatre. In September 1998, the FDA began requiring manufacturers to specify the latex content of their products and it became mandatory to issue warnings on some of their products regarding the risk of allergic reactions if natural rubber latex was used in their production.
There are currently still many products in use in UK ophthalmic operating theatres that contain natural rubber latex, but are not labelled as such. There is an increasing trend for manufacturers, however, to make all their products latex-free, with explicit labelling. However, at the time of writing of this article, the latex content of some specific operating theatre equipment required verification from the individual manufacturers. Similarly, some older stocks of equipment/drugs may contain latex, whilst newer stocks may be latex-free—the only way to verify the latex content to contact the manufacturer with the stock batch number (This applies, for example, to some sleeves in phacoemulsification equipment, viscoelastic devices). While conducting the research for this paper, the authors encountered many ophthalmic products that contained natural rubber latex; these are listed in Table 1. A list of NRL-free alternatives, if available, is also provided where possible. This list is not meant to be exhaustive, and in most cases only the commonly used items were researched.
A significant number of the rubber seals for injectable drug preparations do contain latex and anaphylaxis has been known to occur via parenteral exposure of allergen. The 1998 FDA ruling regarding labelling of products does not extend to the latex-containing medication vials; therefore, the only way to ensure safety is by contacting the manufacturer.73 Operating theatre equipment purchased prior to 1998 will usually not have latex content labelling. In hospitals where latex-free protocols exist, the practice of draping the matting and cushions, whose latex content is unknown, with polythene sheeting or a cloth drape reducing skin contact is often performed. The effectiveness of this practice is unknown. Some manufacturers contacted during the writing of this paper refrained from providing a list of their latex-containing products. Reasons cited included a rapidly changing product catalogue with gradual elimination of NRL content from their product lines; therefore they recommended direct contact with the manufacturer itself to ensure the most up-to-date information.
Disclaimer
It is hoped that this review article will act as a preliminary guide for the management of latex-allergic patients undergoing cataract surgery. It is recommended that local protocols for cataract surgery in latex-allergic patients should be devised with collaboration between the local ophthalmic team, anaesthetists, general physicians and theatre staff. It is also stressed that the latex content for equipment and medication should be checked with the manufacturer if in doubt.
Conclusion
It is unknown why the prevalence of latex allergy is increasing. Many subspecialties have addressed the problem by educating the healthcare workers involved about the scale of the problem, and the potentially severe risks to individual patients. At present, there is no cure for latex allergy and its treatment is based on prevention, by reducing its exposure to the patient. There is FDA legislation in the United States for manufacturers to provide information on the latex content of their products; however, no such legislation exists in the United Kingdom at present. Manufacturers and suppliers of ophthalmic products in the United Kingdom are currently providing information on a voluntary basis only. For detailed information about a product's latex content, the supplier/manufacturer often needs to be contacted directly.
The use of alternative latex-free equipment and protocols can contribute to providing a safer operating environment for latex allergic patients. These protocols can only be effectively implemented after all the healthcare workers involved in the chain of care for the cataract patient have been educated about the relevance of latex allergy in cataract surgery. It is hoped that this article will contribute to this.
References
Lee MH, Kim KT . Latex allergy: a relevant issue in the general pediatric population. J Pediatr Health Care 1998; 12: 242–246.
Poley Jr GE, Slater JE . Latex allergy. J Allergy Clin Immunol 2000; 105: 1054–1062.
Neuget AI, Ghatak AT, Miller RL . Anaphylaxis in the United States: an investigation into its epidemiology. Arch Internal Med 2001; 161: 15–21.
Niggemann B, Buck D, Michael T, Wahn U . Latex provocation tests in patients with spina bifida: who is at risk of becoming symptomatic? J Allergy Clin Immunol 1998; 102: 665–670.
Kashima ML, Tunkel DE, Cummings CW . Latex allergy: an update for the otolaryngologist. Arch Otolaryngol—Head Neck Surg 2001; 127: 442–446.
Barbara J, Chabane MHY, Leynadier F . Retention of airborne latex particles by a bacterial and viral filter used in anaesthesia apparatus. Anaesthesia 2001; 56: 231–234.
Floyd PT . Latex allergy update. J Perianaesth Nurs 2000; 15: 26–30.
Patterson LJ, Milne B . Latex anaphylaxis causing heart block: role of ranitidine. Can J Anaesth 1999; 46: 776–778.
Shapiro JH . Raising eyebrows: problems that get anesthesiologists' attention. Seminars in Pediatric Surgery 1999; 8: 45–48.
Kelly KJ, Walsh Kelly CM . Latex allergy: a patient and health care system emergency. Ann Emergency Med 1998; 32: 723–729.
Dakin MJ, Yentis SM . Latex allergy: a strategy for management. Anaesthesia 1998; 53(8): 774–781.
Strauss RM, Gawkrodger DJ . Occupational contact dermatitis in nurses with hand eczema. Contact Dermatitis 2001; 44: 293–296.
Toraason M, Sussman G, Biagini R, Meade J, Beezhold D, Germolec D . Latex allergy in the workplace. Toxicol Sci 2000; 58: 5–14.
Valsecchi R, Leghissa P, Cortinovis R, Cologni L, Pomesano A . Contact urticaria from latex in healthcare workers. Dermatology 2000; 201: 127–131.
Tarlo SM, Sussman GL, Holness DL . Latex sensitivity in dental students and staff: a cross sectional study. J Allergy Clin Immunol 1997; 99: 396–401.
Yeang HY, Chow KS, Yusof F, Arif SA, Chew NP, Loke YH . Appraisal of latex glove proteins in the induction of sensitivity to multiple latex allergens. J Invest Allergol Clin Immunol 2000; 10: 215–222.
Hayes BB, Afshari A, Millecchia L . Evaluation of percutaneous penetration of natural rubber latex proteins. Toxicol Sci 2000; 56(2): 262–270.
Petsonk EL . Couriers of asthma: antigenic proteins in natural rubber latex. Occup Med 2000; 15: 421–430.
Beezhold DH, Reschke JE, Allen JH, Kostyal DA, Sussman GL . Latex protein: a hidden “food” allergen? Allergy Asthma Proc 2000; 21: 301–306.
Perkin JE . The latex and food allergy connection. J Am Dietetic Assoc 2000; 100: 1381–1384.
Kim KT, Hussain H . Prevalence of food allergy in 137 latex-allergic patients. Allergy Asthma Proc 1999; 20: 95–97.
Blanco C, Diaz-Perales A, Collada C, Sanchez-Monge R, Aragoncillo C, Castillo R et al. Class 1 chitinases as potential panallergens involved in the latex-fruit syndrome. J Allergy Clin Immunol 1999; 103: 507–513.
Chen Z, Posch A, Cremer R, Raul-Heimsoth M, Baur X . Identification of hevein (Hev b6.02) in Hevea latex as a major cross-reacting allergen with avocado fruit in patients with latex allergy. J Allergy Clin Immunol 1998; 102: 476–481.
Hack ME . The prevalence of latex allergy in operating theatre staff. Anaesth Intensive Care 2001; 29: 43–47.
Saxon A, Ownby D, Huard T, Parsad R, Roth HD . Prevalence of IgE to natural rubber latex in unselected blood donors and performance characteristics of AlaSTAT testing. Ann Allergy Asthma Immunol 2000; 84: 199–206.
Faust K, Shrewsbury C, Zaglaniczny K, Jarrett M . A comparative analysis of latex allergy in the healthy versus high risk pediatric population. AANA J 1999; 67: 461–466.
Holness DL, Mace SR . Results of evaluating health care workers with prick and patch testing. Am J Contact Dermatitis 2001; 12: 88–92.
Kim KT, Wellmeyer EK, Miller KV . Minimum prevalence of latex hypersensitivity in health care workers. Allergy Asthma Proc 1999; 20: 387–391.
Horwitz IB, Kammeyer-Mueller JD, McCall BP . Assessing latex allergy among health care employees using workers' compensation data. Minnesota Med 2001; 84(3): 47–50.
Horwitz IB, Arvey RD . Workers' compensation claims from latex glove use; a longitudinal analysis of Minnesota data from 1988 to 1997. J Occup Environ Med 2000; 42: 932–938.
Pridgeon C, Wild G, Ashworth F, Egner W, Ward AM . Assessment of latex allergy in a healthcare population: are the available tests valid? Clin Exp Allergy 2000; 30: 1444–1449.
Chen Z, Cremer R, Posch A, Raulf-Heimsoth M, Baur X . On the allergenicity of Hev b1 among health care workers and patients with spina bifida allergic to natural rubber latex. J Allergy Clin Immunol 1997; 100; 684–693.
Mikkola JH, Alenius H, Kalkkinen N, Turjanmaa K, Palosuo T, Reunala T . Hevein-like protein domains as a possible cause for allergen cross-reactivity between latex and banana. J Allergy Clin Immunol 1998; 102: 1005–1012.
Chen Z, Duser M, Flagge A, Maryska S, Sander I, Raulf-Heimsoth M et al. Identification and characterization of cross-reactive natural rubber latex and Ficus benjamina allergens. Int Arch Allergy Immunol 2000; 123: 291–298.
Brehler R, Adams E, Sedlmayer S . Cross reactivity between Ficus benjamina (weeping fig) and natural rubber latex. Allergy 2000; 53: 402–406.
Raulf-Hemisoth M, Sander I, Chen Z, Borowitzki G, Diewald K, van Kampen V et al. Development of a monoclonal antibody-based sandwich ELISA for detection of the latex allergen Hev b 1. Int Arch Allergy Immunol 2000; 123: 236–241.
Hamilton RG, Adkinson Jr NF . Diagnosis of natural rubber latex allergy: multicenter latex skin testing efficacy study Multicenter Latex Skin Testing Study Task Force. J Allergy Clin Immunol 1998; 102: 482–490.
Sowka S, Hsieh LS, Krebitz M, Akasawa A, Martin BM, Peterbauer CK et al. Identification and cloning of prs a1 a 32-kDa endochitinase and major allergen of avocado and its expression in the yeast Pichia pastoris. J Biol Chem 1998; 273: 28091–28097.
Johnson BD, Kurup VP, Sussman GL, Arif SA, Kelly KJ, Beezhold DH et al. Purified and recombinant latex proteins stimulate peripheral blood lymphocytes of latex allergic patients. Int Arch Allergy Immunol 1999; 120: 270–279.
Yitalo L, Makkinen- Kiljunen S, Tarjanmaa K, Palosuo T, Reunala T . Cow's milk casein, a hidden allergen in natural rubber latex gloves. J Allergy Clin Immunol 1999; 104: 177–180.
Hamilton RG, Adkinson NF . Validation of the latex glove provocation procedure in latex allergic subjects. Ann Asthma Immunol 1997; 79: 266–272.
Kurtz KM, Hamilton RG, Schaefer JA, Adkinson Jr NF . A hooded exposure chamber method for semiquantative latex aeroallergen challenge. J Allergy Clin Immunol 2001; 107: 178–184.
Palczynski C, Walusiak J, Ruta U, Gorski P . Nasal provocation test in the diagnosis of natural rubber latex allergy. Allergy 2000; 55: 34–41.
Palczynski C, Walusiak J, Hanke W, Gorski P . Latex allergy in Polish nurses. Am J Ind Med 1999; 35: 413–419.
Wakelin SH, Jenkins RE, Rycroft RJ, McFadden JP, White IR . Patch testing with natural rubber latex. Contact Dermatitis 1999; 40: 89–93.
Cohen DE, Scherman A, Stewart L, Taylor J, Pratt M, Trotter K et al. American Academy of Dermatology's position paper on latex allergy. J Am Acad Dermatol 1998; 39: 98–106.
Slater JE . Latex allergy. J Allergy Clin Immunol 1994; 94: 139–149.
Leynadier F, Pecquet C, Dry J . Anaphylaxis to latex during surgery. Anaesthesia 1989; 44: 547–550.
Laoprasert N, Swanson MC, Jones RT . Inhalation challenge testing of latex-sensitive health care workers and the effectiveness of laminar flow HEPA-filtered helmets in reducing rhinoconjunctival and asthmatic reactions. J Allergy Clin Immunol 1998; 102: 998–1004.
Allmers H, Brehler R, Chen Z, Raulf-Heimsoth M, Fels H, Baur X . Reduction of latex aeroallergens and latex-specific IgE antibodies in sensitized workers after removal of powdered natural rubber latex gloves in a hospital. J Allergy Clin Immunol 1998; 102: 841–846.
Barbara J, Chabane MH, Leynadier F, Girard F . Retention of airborne latex particles by a bacterial and viral filter used in anaesthesia apparatus. Anaesthesia 2001; 56: 231–234.
Tomazic VJ, Shampaine EL, Lamanna A, Withrow TJ, Adkinson Jr NF, Hamilton RG . Cornstarch powder on latex products is an allergen carrier. J Allergy Clin Immunol 1994; 93: 751–758.
Petsonk EL . Couriers of asthma: antigenic proteins in natural rubber latex. Occup Med 2000; 15: 421–430.
Gibbon KL, McFadden JP, Rycroft RG, Ross JS, Chinn S, White IR . Changing frequency of thiural allergy in healthcare workers with contact dermatitis. Br J Dermatol 2001; 144: 347–350.
Strauss RM, Gawkrodger DJ . Occupational contact dermatitis in nurses with hand eczema. Contact Dermatitis 2001; 44: 293–296.
Wakelin SH, White IR . Natural rubber latex allergy. Clin Exp Dermatol 1999; 24: 245–248.
Vila L, Sanchez G, Ano M, Uasuf CG, Sanz ML . Risk factors for latex sensitization among health care workers. J Invest Allergol Clin Immunol 1999; 9: 356–360.
Trape M, Schenck P, Warren A . Latex gloves use and symptoms in health care workers 1 year after implementation of a policy restricting the use of powdered gloves. Am J Infect Control 2000; 28: 352–358.
Philips VL, Goodrich MA, Sullivan TJ . Health care worker disability due to latex allergy and asthma: a cost analysis. Am J Public Health 1999; 89: 1024–1028.
Page EH, Esswein EJ, Petersen MR, Lewis DM, Bledsoe TA . Natural rubber latex: glove use sensitization and airborne and latent dust concentrations at a Denver Hospital. J Occup Environ Med 2000; 42: 613–620.
Anonymous. Synthetic surgical gloves. Health Devices 2000; 29: 37–66.
Russell-Fell RW . Avoiding problems: evidence-based selection of medical gloves. Br J Nurs 2000; 9: 139–142.
Mahler V, Fischer S, Fuchs T, Ghannadan M, Valent P, Fartasch M . Prevention of latex allergy by selection of low allergen gloves. Clin Exp Allergy 2000; 30: 509–520.
Hwang KL, Kou SJ, Lu YM, Yang NC . Evaluation of the quality of surgical gloves among four different manufactures. Ann Occup Hyg 1999; 43: 275–281.
Jackson EM, Arnette JA, Martin ML, Tahir WM, Frost-Amer L, Edlich RF . A global inventory of hospitals using powder-free gloves: a search for principled medical leadership. J Emergency Med 2000; 18: 241–246.
Hepner DL . Sudden Bronchospasm on intubation: latex anaphylaxis? J Clin Anesth 2000; 12: 162–166.
Keh C, Soon Y, Wong LS . Latex allergy: an emerging problem in theatres. Int J Clin Practice 2000; 54: 582–584.
Bergwerk KL, Kodsir SR . Latex allergy associated with the latex cover on the Tonopen. Am J Ophthalmol 1999; 127: 191.
Beezhold DH, Hickey VL, Sussman GL . Mutational analysis of the IgE epitopes in latex allergen Hev b5. J Allergy Clin Immunol 2001; 107: 1069–1076.
Leynadier F, Herman D, Vervloet D, Andre C . Specific immunotherapy with a standardized latex extract versus placebo in allergic healthcare workers. J Allergy Clin Immunol 2000; 106: 585–590.
Brehler R, Kutting B . Natural rubber latex allergy: a problem of interdisciplinary concern in medicine. Arch Int Med 2001; 161: 1057–1064.
Meeropol EV . The R.U.B.B.E.R. tool: screening children for latex allergy. J Pediatr Health Care 1998; 12: 320–323.
Smith CC . Risk of latex allergy from medication vial closures. Ann Pharmacother 1999; 33: 373–374.
Acknowledgements
Financial support: Nil. Proprietary interest: Nil.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cheung, D., Gillow, T. Cataract surgery for natural rubber latex allergic patients. Eye 17, 129–138 (2003). https://doi.org/10.1038/sj.eye.6700321
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700321