Abstract
Central retinal vein occlusion is one of the commonest vascular diseases of the eye. The pathogenesis is multifactorial with both local factors and systemic diseases being aetiologically important. Many thrombophilic conditions have recently been identified and studies looking at their potential role in CRVO have been undertaken. The aim of this review is to critically appraise these studies as to date many have given conflicting results, making it far from clear what role thrombophilic conditions play in CRVO. It appears that hyperhomocysteinaemia and antiphospholipid syndrome are causes of CRVO and there is evidence that disorders causing hypofibrinolysis may also be important. The common hereditary thrombophilic conditions however do not appear to be strong risk factors but larger studies are needed for a definitive answer.
Similar content being viewed by others
Background
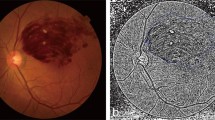
Following damage to vascular endothelium, platelets adhere to sub-endothelial tissues and then aggregate to one another via fibrinogen and von-Willebrand factor. The coagulation cascade—both intrinsic and extrinsic pathways—simultaneously activated, forms a blood clot consisting of polymerized fibrin. Ultimately the fibrin is digested by plasmin which has been converted from its inactive form-plasminogen—by tissue plasminogen activator which is itself regulated by plasminogen activator inhibitor (Figure 1).
The development of the haemostastic mechanism was a critical step to the evolutionary changes that accompanied the development of a circulation. With something so critical it is probably not surprising that a very thorough and complex control system similarly evolved to regulate haemostasis so that inappropriate clots are not formed. Abnormalities of this regulatory system may be inherited or acquired and pre-dispose patients to thrombosis. In 1965 the first family with anti-thrombin III deficiency and a predisposition to thrombosis was described and since then several other abnormalities, both quantitative and qualitative, have been identified, many of them very recently (Table 1). Also many of the recently described abnormalities are relatively common compared to those previously identified. Phenotypically most patient’s abnormalities cause venous rather than arterial thrombosis and we are now able to identify a pre-disposing factor in about 70–80% of patients with recurrent venous thrombo-embolic disease.
Early kindred studies showed however the phenotypic penetrance of many abnormalities was low and apparently variable with some family members with protein C deficiency suffering VTEs whilst others did not. The discovery of the relatively common factor V Leiden (FVL) helped explain this apparent anomaly.1 This abnormality is a single point mutation of the factor V gene which prevents protein C binding to and inactivating factor V.2 The multigenic basis for VTE was therefore established and has been confirmed in other kindreds with different abnormalities.3,4
It also became apparent that there are interactions and synergy between environmental and genetic predisposing factors. The average age of women with FVL for the first DVT is 28 years compared to 62 in men! We now know that FVL increases the risk of thrombosis 6–8 fold and the combined third generation oral contraceptives 4-fold. If however you have FVL and take the pill your risk is 30–50 fold, ie synergy.5 Similar synergistic interactions have been described with hormone replacement therapy and pregnancy.6,7,8 Similarly in men the age of first VTE is partly due to increasing immobility with age which acts in tandem with any inherited thrombophilia.
Central retinal vein occlusion
Similar to general venous thrombosis CRVO appears to be a condition with a multiple aetiology. There is an increased incidence with age with over 50% of patients being over 65 years of age.9,10 The incidence is higher in patients with diabetes, hypertension, retinal artery disease, open angle glaucoma, hyperlipidaemia and in those using oral contraception and hormone replacement therapy.11,12,13,14,15 Not surprisingly therefore clinicians started to look at the potential role of thrombophilia in the development of CRVO. Early reports mostly consisted of individual case reports but more recently studies with adequate statistical power have been published. The aim of this review is to present the available data from these studies to give an insight into the potential role of thrombophilia in patients who have experienced CRVO.
Protein C, protein S and anti-thrombin III deficiency
When the coagulation cascade is activated, both the intrinsic and extrinsic pathways help in the conversion of prothrombin to thrombin. Thrombin has many different roles in regulating thrombosis other than the production of fibrin from fibrinogen. In particular it binds with thrombomodulin which in the presence of protein S converts inactive protein C to an active form. Activated protein C binds to and inhibits the procoagulant action of activated factor V and factor VIII. Thus people deficient in protein S or protein C are prone to thrombosis.
Anti-thrombin III is a serine protease inhibitor which not only inhibits thrombin generation but also other coagulation factors notably activated X, IX, XI and XII. Deficiency of ATIII also results in an increased risk of thrombosis.
Initial case reports that deficiency of these naturally occurring anticoagulants may be a contributing factor to CRVO led to larger studies. Bertram et al in a study of 82 patients with CRVO found two with protein C, two with protein S and one with ATIII deficiency (overall, 6% of patients).16 As a group however the levels of protein C, protein S and ATIII were not significantly different from the normal range. Similarly in a study of 37 patients aged <50 years, three (8%) were found to have deficiency of protein C, protein S or ATIII.17 Tekeli et al found protein C deficiency in 20% (9/45) of patients with either central or branch vein occlusion.18 He also identified two cases of protein S deficiency and one of ATIII deficiency, giving an incidence of naturally occurring anticoagulant deficiency of 27% overall. There was however no significant difference in the levels of the various anticoagulants compared to the control group. Protein C deficiency however was significantly more prevalent in patients with CRVO (six out of 14 patients) than branch vein occlusion (three out of 31 patients) (P < 0.05). A similarly high incidence was found in a study of 57 patients with protein C deficiency in 20% (8/42), protein S deficiency in 19% (12/56) and ATIII deficiency in 7% (4/54).19 In this study however no comparison was made between the patient group and normal controls with regards to the levels of proteins C and S and ATIII. Three smaller studies however with only 14, 21 and 35 patients each with CRVO failed to identify any patients with these deficiencies.20,21,22 A controlled population study with 69 patients with CRVO compared to a normal matched population showed ATIII levels were significantly lower (although still within the normal range) in normal controls than patients!23
Superficially it appears that there may be an association between CRVO and deficiency of these naturally occurring anticoagulants. It is known however that these anticoagulants are very labile and levels physiologically fluctuate. It is recommended that they should be measured on at least two separate samples and if found abnormal confirmed with a third estimation. In virtually all studies single measurements have been used. The studies can also be criticised for lacking the statistical power to show a true difference either due to small sample size or lack of a suitable control group.
Factor V Leiden/activated protein C resistance
Activated protein C binds to activated factor V and activated factor VIII resulting in their degradation. In 1993 Dahlback and colleagues described a familial condition in which there was a poor anticoagulant response to activated protein C resistance.1 They went on to show that this was a common cause of venous thrombosis. In 1994 a single point mutation in the factor V gene at position 1691 resulting in a single nucleotide change G-A was identified—so-called Factor V Leiden.2 This was demonstrated to be responsible for the poor anticoagulant response to activated protein C as it only weakly bound to factor V and hence degradation was reduced.
This abnormality therefore can be detected either by molecular genetic testing or coagulation tests. The initial coagulation kits for measuring activated protein C resistance were not very specific or sensitive but the third generation kits now available may even distinguish heterozygous from homozygous carriers of FVL. It is estimated that FVL is present in about 5% of the normal (Caucasian) population and plays a significant role in 20–30% of all VTEs. Not surprisingly therefore with such a commonly occurring abnormality, case reports identifying patients with CRVO and APC resistance/FVL began to appear in the mid 1990s.
There have now been many cohort studies looking at the frequency of APC resistance/FVL and their role in CRVO, as shown in Table 2.17,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36 Although many studies suggest an increased frequency of APCR/FVL in patients with CRVO only two out of nine studies in which the incidence of APCR/FVL is compared with a normal cohort is there a significantly increased incidence of this abnormality. Surprisingly both of these studies included patients of any age where one would have anticipated an association with younger patients. Indeed a sub-group analysis by Larsson et al of 23 patients younger than 45 years showed that six (26%) had APCR which was significantly different to their normal control group (P = 0.0466).17 This study like that of Williamson et al used an early type of APCR assay which proved not to be as accurate as later assays.23 Indeed Ciardella et al studied 84 patients with CRVO and 70 controls. They found, using a first generation APCR assay, that 45% of CRVO patients had this abnormality compared to 9% of controls (P < 0.0001) but when using a second generation assay however there was no significant difference.31 Also there was no difference in the frequency of FVL mutation between the two groups. In the study by Gleuk et al, 24% of their patients with CRVO had also experienced another thrombosis, primarily deep venous thrombosis, possibly indicating inadvertent patient selection.20
Six studies have investigated the role of APCR/FVL in hemispheric and retinal branch occlusion.18,25,30,31,32,33,35 Although patients with this thrombophilic tendency were identified, the incidence compared to the normal population was not increased (in studies where a direct comparison was made).
Prothrombin gene mutation G20210A
In 1996 a new pro-thrombotic abnormality was described. A single point mutation was identified at position 20210 of the prothrombin gene resulting in a single nucleotide change G-A.37 This abnormality is present in 2–3% of the normal (Caucasian) population and for reasons not fully understood causes a rise in prothrombin levels.
Five studies have looked at this abnormality in CRVO patients.20,32,35,38,39 Between them a total of 232 patients have been assessed but only seven patients with this abnormality were identified—a frequency not dissimilar to that expected in the normal population.
Anti-phospholipid syndrome
Anti-phospholipid syndrome (APS) is a condition in which antibodies to phospholipid activate the coagulation cascade leading to both arterial and venous thrombosis.40 They can be detected using an immunological assay—anti-cardiolipin antibodies (ACA-IgG and IgM) or their effect on coagulation using a test for lupus anticoagulant (LA) such as the direct Russell Viper venom test. The condition can either be ideopathic or secondary to another condition such as systemic lupus erythematosus, infection or pregnancy. There is not a simple correlation between the two diagnostic tests and both should be performed to rule out APS. Also, certainly in the case of deep venous and placental thrombosis, the risk of thrombosis is higher if both tests are abnormal as opposed to just one. There is at present a debate as to whether IgM ACAs alone are able to induce thrombosis.
Both ocular and neuro-ophthalmic vascular eye diseases have been identified in patients with APS including arterial and vascular occlusion, ischaemic optic atrophy, preretinal neovascularization and vitreous haemorrhage.41,42,43 Overall 6–8% of patients with APS have ocular manifestations. There have been several recent comparative studies using LA and/or ACA to detect APS with many identifying an association between APS and CRVO (Table 3). These studies have shown a relatively consistent level of APS frequency in the control population of <5% but the incidence in patients with CRVO has ranged from 0–46%!17,19,20,21,44,45,46,47 The two studies by Abu El-Asrar and colleagues (both of which showed a significant increased frequency of LA/ACA) stand out from virtually all other studies in that they also had a extremely high level of all thrombophilic abnormalities detected in their CRVO cohorts.19,45 A total of 18 abnormalities in their earlier study of 17 patients and 46 abnormalities in 57 patients in their latter study were detected. In the study by Gleuk et al although a very high and significant difference in the incidence of LA was found, there was no difference at all in the incidence of ACA antibodies.20 Similarly in two studies in which the actual levels of ACA were analysed there was no difference in mean levels between patients and normal controls (5.6 vs 4.6 GPLU respectively and 5.4 vs 5.1 respectively).44,46 In the study by Corbo-Soriano et al however, not only was there a significantly increased incidence of ACA in CRVO patients but the levels were also significantly higher as a group compared to controls—IgG 10.1 vs 3.37 GPLU, IgM 7.6 vs 4.42 GPLU respectively.47
Branch retinal vein occlusion has also been studied with similar findings in terms of the role of APS to those found in the CRVO patients.45,47
Thus in conclusion APS may play a role in CRVO but very disparate results have been obtained due to many studies probably lacking adequate statistical power.
Hyperhomocysteinaemia
Homocysteine is a naturally occurring amino acid not found in protein. In a rare autosomally recessive inherited disorder a high level of homocysteine is found—homocystinuria—and patients suffer from an increased risk of both arterial and venous thrombosis.48 This disorder is due to rare enzyme deficiencies of cystathione β-synthase (more commonly) or methylene tetrahydrofolate reductase.
In 1976 Wilcken reported the first case controlled study showing that higher than normal levels of homocysteine in ‘normal’ people pre-disposes to arterial vascular disease and later studies confirmed it was also a risk factor for venous thrombosis.49,50 Although the exact mechanism(s) by which hyperhomocysteinaemia causes thrombosis are unknown, it has been shown to be directly toxic to endothelial cells, impair thrombomodulin expression, directly activate factor V and inhibit protein C activation.51,52,53,54
There are many causes for hyperhomocysteinaemia including vitamin deficiencies (pyridoxine, folic acid, vitamin B12) chronic illnesses (chronic renal failure, diabetes, cancer), drugs (methotrexate, anti-epileptic agents), as well as the rare enzyme deficiencies mentioned above. In 1988 however a mild form of hyperhomocysteinaemia was identified due to a thermolabile variant of MTHFR.55 This was subsequently shown to be due to a single point mutation in the MTHFR gene C→T.56 This mutation is very common (allellic frequency 35%) in the normal population such that in North America 12% are homozygous for this mutation (TT) and 45% heterozygous (CT).57 It appears however that many normal patients with the TT genotype have normal homocysteine levels as the phenotypic expression is critically dependent on folic acid intake and folate levels.58
In keeping with other thrombophilic conditions hyperhomocysteinaemia is synergistic with other hereditary and acquired pro-thrombotic disorders including hypertension.59,60
There have been seven studies to date investigating the role of hyperhomocysteinaemia in CRVO. In 1998 Salomon et al found, in 102 patients with CRVO, BRVO and hemi-RVO, that homozygosity for the thermolabile MTHFR mutation was present in 25.5% of patients compared to 15.2% of control patients, giving an overall odds ratio of 1.9.32 Indeed this mutation was along with hypertension and a family history of stroke, independent risk factors for RVO whereas FVL and the prothrombin mutation were not. Similar results were obtained by Loewenstein et al in 59 patients who found a homozygous mutation rate of 18.6% compared to 10.4% in healthy controls (P < 0.038).61 These results however are not in accordance with Gleuk et al who found no such association in 17 CRVO patients compared to 234 controls (P = 0.22).20 Gleuk also found no association between plasma homocysteine levels and the risk of CRVO.
In contrast four studies have found significant associations between homocysteine levels and CRVO. In a study of 74 patients with CRVO, 21.6% had homocysteine levels above the 95th centile (P = 0.003).62 In addition five out of nine (55%) patients with bilateral CRVO had hyperhomocysteinaemia. Similarly a study by Cahill et al in 40 CRVO patients found a mean homocysteine level of 13.7 μmol/l compared to 11.7 μmol/l in BRVO patients (21 cases) and 10.7 μmol/l in 87 controls—CRVO vs normals (P = 0.0001), BRVO vs normals (P = 0.097).63 They also identified that hyperhomocysteinaemia was an independent risk factor for retinal vascular disease. These findings were confirmed by Martin et al who found significant associations between homocysteine levels and CRVO (36 patients) and BRVO (24 patients) (P = 0.045).64 A study by Wenzler et al identified two patients with RVO and hyperhomocysteinaemia. They suggested that the frequency was significantly higher than the carriage frequency of homocystinuria.65 This comparison however from what we now understand about hyperhomocysteinaemia is not valid.
At present there are few commercially available homocysteine assays and most studies use in-house methods making comparison between different studies difficult, but despite this five out of six studies indicate a role for homocysteine in the pathogenesis of CRVO.
Abnormalities of fibrinolysis
Several studies have looked at the incidence of these rarer/poorly defined causes of thrombophilia in the context of CRVO. Larsson et al in a study of 37 patients found no cases of plasminogen deficiency (incidence of 0.3% in the normal population).17 Williamson found normal levels of tissue plasminogen activator but significantly low levels of plasminogen activator inhibitor (PAI) (P = 0.03) indicating a hypofibrinolytic state in his 87 patients with CRVO.23 The high levels of PAI were confirmed by Gleuk et al who also showed, in 17 patients, a significantly higher level of the 4G/4G and 4G/5G polymorphisms of the PAI gene (P = 0.03).20 The PAI gene has two polymorphisms, 4G and 5G with the 4G allele being associated with significantly higher levels of PAI and consequently hypofibrinolysis. Lipoprotein Lp(a) has been associated with CRVO in many studies and is thought to be hypofibrinolytic due to its sequence homology to plasminogen, such that it competes with plasminogen for fibrin binding thus inhibiting fibrin degredation.66 Gleuk also showed a direct correlation between the three PAI polymorphisms—4G/4G, 4G/5G, 5G/5G—and Lp(a) levels, with 4G/4G patients having highest levels and these were higher than the normal controls (62 vs 5.3 mg/dl, P = 0.05). Interestingly however the association between polymorphism status and Lp(a) levels was not observed in the normal control group of 234 individuals.
Conclusion
CRVO is like other types of venous-thromboembolism (VTE) disorder, being multifactorial in origin, in which Virchows triad of abnormalities of blood flow, abnormal vessel walls and blood coaguability all play a role. There are now identified many hereditary and acquired causes of thrombophilia and therefore it is not surprising that these have been investigated in the context of CRVO. In undertaking any study however, goals should be set at the beginning as to what one is hoping to achieve. In thrombophilia studies for the common causes of VTE eg DVT, PE, these have largely been completed with the intention of answering three questions: (1) Is thrombophilia pathogenic in the aetiology of VTE? (2) Would the identification of a thrombophilic tendency alter the immediate management of a VTE episode? (3) Would subsequent management eg secondary prophylaxis be altered in patients shown to have a thrombophilic tendency? The answers to these three questions for DVT are yes, no and maybe, respectively. If one applies these three questions to CRVO, the answers from the literature would have to be maybe, maybe and maybe, respectively.
From the published studies the role of thrombophilia in the aetiology of CRVO is far from clear, due to researchers looking at different age and ethnic groups, different subgroups of CRVO as well as using different assays. Some authors have found highly significant differences in proteins C and S, ATIII, and FVL/APCR, compared with normal controls. Many of these studies however are, for the reasons outlined in the relative sections, far from conclusive and only a very large, probably national, or international-, study using a single laboratory for each test and follow-up samples if required, would answer the questions completely. This would enable multivariate analysis of all the known pathogenetically important risk factors, eg hypertension to be included as well as thrombophilia testing.
The role of antiphospholipid antibodies appears to be clearer cut. We already know that APS has a high incidence of ocular problems and testing for this condition may well alter management, as patients have a very high rate of VTE recurrence. Life-long anticoagulation is usually recommended for these patients if serious VTE eg PE occurs elsewhere in the body. Therefore after CRVO which has a recurrence rate of 3–15%, consideration especially in this sub-group of patients should be given to anticoagulation.67,68,69 Indeed although early studies showed no role for anticoagulation eg warfarin in the management of CRVO, a randomised study in patients with proven thrombophilia would be of interest. Hyperhomocysteinaemia also appears to be a risk factor with an easily available therapeutic option for secondary prevention. Treatment to reduce hyperhomocysteinaemia involves small doses of folic acid and vitamins B6 and B12, which are cheap and have no side effects.70 As with APS, if a study were to be undertaken to assess the benefit of this therapy, as secondary prevention a single laboratory to perform the relative diagnostic and follow-up assays would be ideal. Given the association between retinal artery (as well as other arteriopathies) and CRVO, it is intriguing that the thrombophilic tendencies which appear to be particularly associated with CRVO, ie APS and hyperhomocysteinaemia, cause both arterial and venous thrombosis. To this list may be added disorders of fibrinolysis but at present further confirmatory studies are probably required. Also new studies should be undertaken looking at the levels of clotting factors VIII, IX and XI.
In conclusion the case for widespread screening for thrombophilia in CRVO patients has yet to be made. Antiphospholipid syndrome and hyperhomocysteinaemia however are of great interest and further studies looking at their potential aetiological roles as well as primary and secondary therapeutic interventions are warranted.
References
Dahlback B, Carlsson M, Svensson PJ . Familial thrombophilia due to a previously unrecognised mechanism characterised by a poor anticoagulant response to activated protein C: prediction of a cofactor to activated protein C. Proc Natl Acad Sci USA 1993; 90: 1004–1008
Bertina RM, Koeleman BPC, Koster T, Rosendaal FR, Dirven RJ, De Ronde H et al. Mutation in the blood coagulation factor V associated with resistance to activated protein C. Nature 1994; 360: 64–67
Koeleman BPC, Reitsma PH, Allaart CF, Bertina RM . Activated protein C as an additional risk factor for thrombosis in protein C deficient families. Blood 1994; 84: 1031–1035
Koeleman BPC, Van Rumpt D, Hamulyak K, Reitsma PH, Bertina RM . Factor V Leiden: an additional risk factor for thrombosis in protein S deficient families?. Thromb Haemostat 1995; 74: 580–583
Vandenbroucke JP, Koster T, Briet E, Reitsma PH, Bertina RM, Rosendaal FR . Increased risk of venous thrombosis in oral-contraceptive users who are carriers of factor V Leiden mutation. Lancet 1994; 344: 1453–1457
Jick H, Derby LE, Myers MW, Vasilakis C, Newton KM . Risk of hospital admission for ideopathic venous thromboembolism among users of postmenopausal oestrogens. Lancet 1996; 348: 981–983
Daly E, Vessey MP, Hawkins MW, Carson JL, Gough P, Marsh S . Risk of venous thromboembolism in users of hormone replacement therapy. Lancet 1996; 348: 977–980
Hellgren M, Svenssonn PJ, Dahlback B . Resistance to activated protein C as a basis for venous thromboembolism associated with pregnancy and oral contraception. Am J Obstet Gynaecol 1995; 173: 210–213
Hayreh SS, Zimmerman MB, Podhajsky P . Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmol 1994; 117: 429–441
Mitchell P, Smith W, Chang A . Prevalence and associations of retinal vein occlusion in Australia. The Blue Eye Mountain Study. Arch Ophthalmol 1996; 114: 1243–1247
Dodson PM, Galton DJ, Hamilton AM, Blach RK . Retinal vein occlusion and the prevalence of lipoprotein abnormalities. Br J Ophthalmol 1982; 66: 161–164
Rath EZ, Frank RN, Shin DH, Kim C . Risk factors for retinal vein thrombosis: a case-control study. Ophthalmology 1992; 99: 509–514
Kirwin JF, Tsaloumas MD, Vinall H, Prior P, Kritzinger EE, Dodson PM . Sex hormone preparations and retinal vein occlusion. Eye 1997; 11: 53–56
Dodson PM, Clough CG, Downes SM, Kritzinger EE . Does type II diabetes predispose to retinal vein occlusion. Eur J Ophthalmol 1993; 3: 109–113
Hayreh SS, van Heuven WA, Hayreh MS . Experimental retinal vascular occlusion. Pathogenesis of central retinal vein occlusion. Arch Ophthalmol 1978; 96: 311–323
Bertram B, Remky A, Arend O, Wolf S, Reim M . Protein C, protein S and antithrombin III in acute ocular occlusive diseases. Ger J Ophthalmol 1995; 4: 332–335
Larsson J, Hillarp A, Olafsdottir E, Bauer B . Activated protein C resistance and anticoagulant proteins in young adults with central retinal vein occlusion. Acta Ophthalmol Scand 1999; 77: 634–637
Tekeli O, Gursel E, Buyurgan H . Protein C, protein S and antithrombin III deficiencies in retinal vein occlusion. Acta Ophthalmol Scand 1999; 77: 628–630
Abu El-Asrar AM, Abdel Gader AG, Al-Amro S, Al-Momen AK . Hypercoaguable states in patients with retinal venous occlusion. Documenta Ophthalmol 1998; 95: 133–143
Gleuck CJ, Bell H, Vadlamani L, Gupta A, Fontaine RN, Wang P et al. Heritable thrombophilia and hypofibrinolysis. Possible causes of retinal vein occlusion. Arch Ophthalmol 1999; 117: 43–49
Greiner K, Hafner G, Dick B, Peetz D, Prellwitz W, Pfeiffer N . Retinal vascular occlusion and deficiencies in the protein C pathway. Am J Ophthalmol 1999; 128: 69–74
Gottleib JL, Blice JP, Mestichelli B, Konkle BA, Benson WE . Activated protein C resistance, factor V Leiden and central retinal vein occlusion in young adults. Arch Ophthalmol 1998; 116: 577–579
Williamson TH, Rumley A, Lowe GDO . Blood viscosity, coagulation and activated protein C resistance in central retinal vein occlusion: a population controlled study. Br J Ophthalmol 1996; 80: 203–208
Hodgkins PR, Perry DJ, Sawcer SJ, Keast-Hutler J . Factor v and and antithrombin III mutations in patients with ideopathic central retinal vein occlusion. Eye 1995; 9: 760–762
Freyburger G, Bilhou-Nabera C, Dief S, Javorschi S, Labrouche S, Lerebeller MJ et al. Technical and biological conditions influencing the functional APC resistance test. Thromb Haemostat 1996; 75: 460–465
Graham SL, Golgberg I, Murray B, Beaumont P, Chong BH . Activated protein C resistance: low incidence in glaucomatous optic disc haemorrhage and central retinal vein occlusion. Austr NZ J Ophthalmol 1996; 24: 199–205
Raguenes O, Mercier B, Escoffre M, Traore L, Blouch MT, Robinet A et al. Mutation 16910G-A du gene du facteur V: pas d’association avec les thromboses de la veine centrale de la retine (letter). Presse Med 1996; 25: 460
Larsson J, Olafsdottir E, Bauer B . Activated protein C resistance in young adults with central retinal vein occlusion. Br J Ophthalmol 1996; 80: 200–202
Larsson J, Sellman A, Bauer B . Activated protein C resistance in patients with central retinal vein occlusion. Br J Ophthalmol 1997; 81: 832–834
Linna T, Ylikorkala A, Kontula K, Puska P, Tervo T . Prevalence of factor V Leiden in patients with retinal vein occlusion. Thromb Haemostat 1997; 77: 214–216
Ciardella AP, Yannuzzi LA, Freund KB, DiMichele D, Nejat J, De Rosa JT et al. Factor V Leiden, activated protein C resistance and retinal vein occlusion. Retina 1998; 18: 308–315
Salomeno O, Moisseiev J, Rosenberg N, Vidne O, Yassur I, Zivelin A et al. Analysis of genetic polymorphisms related to thrombosis and other risk factors in patients with retinal vein occlusion. Blood, Coag Fibrinol 1998; 9: 617–622
Demirci FYK, Guney DB, Akarcay K, Kir N, Ozbek U, Sirma S et al. Prevalence of factor V Leiden in patients with retinal vein occlusion. Acta Ophthalmol Scand 1999; 77: 631–633
Guven D, Sayinalp N, Kalayci D, Dundar S, Hasiripi H . Risk factors in central retinal vein occlusion and activated protein C resistance. Eur J Ophthalmol 1999; 9: 43–48
Kalayci D, Gurgey A, Guven D, Parlak H, Hasiripi H . Factor V Leiden and prothrombin 20210 A mutation in patients with central and retinal vein occlusion. Acta Ophthalmol Scand 1999; 77: 622–624
Faude S, Faude F, Siegemund A, Wiedemann P . Activated protein c resistance in patients with central retinal vein occlusion in comparison to patients with a history of deep vein thrombosis and a healthy control group. Ophthalmologe 1999; 96: 594–599
Poort SR, Rosendaal FR, Reitsma PH, Bertina RM . A common variation in the 3′-untranslated region of the prothrombin gene is associated with elevated prothrombin levels and an increase in venous thrombosis. Blood 1996; 88: 3698–3703
Backhouse O, Parapia I, Mahomed I, Lee D . Familial thrombophilia and retinal vein occlusion. Eye 2000; 14: 13–17
Larsson J, Hillarp A . The prothrombin gene G20210A mutation and the platelet glycoprotein IIIa polymorphism PIA2 in patients with central retinal vein occlusion. Thromb Res 1999; 96: 323–327
Hughes GRV . Thrombosis, abortion, cerebral disease and the lupus anticoagulant. Br Med J 1983; 287: 1088–1089
Asherson RA, Merry P, Acheson JF, Harris EN, Hughes GR . Antiphospholipid antibodies: a risk factor for occlusive ocular vascular disease in systemic lupus erythematosus and the ‘primary’ antiphospholipid syndrome. Ann Rheum Dis 1989; 48: 358–361
Castanon C, Amigo MC, Banales JL, Nava A, Reyes PA . Ocular vaso-occlusive disease in primary antiphospholipid syndrome. Ophthalmology 1995; 102: 256–262
Giorgi D, Gabrieli CB, Bonomo L . The clinico-ophthalmological spectrum of antiphospholipid syndrome. Ocul Immunol Inflam 1998; 6: 269–273
Glacet-Bernard A, Bayani N, Chretien P, Cochard C, Lelong F, Coscas G . Antiphospholipid antibodies in retinal vascular occlusions. Arch Ophthalmol 1994; 112: 790–795
Abu El-Asrar, Al-Momen AK, Al-Amro S, Abdel Gader AGM, Tabbara KF . Prothrombotic states associated with retinal venous occlusion in young adults. Int Ophthalmol 1996; 20: 197–204
Giordano N, Senesi M, Battisti E, Traversi C, Mattii G, Palumbo F, Gennari C . Antiphospholipid antibodies in patients with retinal vascular occlusion. Acta Ophthalmol 1998; 76: 128–129
Cobo-Soriano R, Sanchez-Ramon S, Aparicio MJ, Teijeiro A, Vidal P, Suarez-Loez M et al. Antiphospholipid antibodies and retinal thrombosis in patients without risk factors: a prospective case-control study. Am J Ophthalmol 1999; 128: 725–732
Mudd SH, Skovby F, Levy HL, Pettigrew KD, Wilcken B, Pyeritz RE et al. The natural history of homocystinuria due to deficiency of cystathione beta-synthase deficiency. Am J Hum Gen 1985; 37: 1–31
Wilcken DEL, Wilcken B . The pathogenesis of coronary heart disease. J Clin Invest 1976; 57: 1079–1082
den Heijer M, Rosendaal FR, Blom HJ, Gerrits WBJ, Bos GMJ . Hyperhomocysteinaemia and venous thrombosis: a meta-analysis. Throm Haemostat 1998; 80: 874–877
Harker LA, Slichter SJ, Scott CR, Ross R . Homocysteinaemia, vascular injury and arterial thrombosis. N Eng J Med 1974; 291: 537
Rodgers GM, Kane WH . Activation of endogenous factor V by a homocysteine-induced vascular endothelial cell activator. J Clin Invest 1986; 77: 1909–1916
Rodgers GM, Conn MT . Homocysteine, an atherogenic stimulus reduces protein C activation by arterial and venous endothelial cells. Blood 1990; 75: 895–901
Lentz SR, Sadler JE . Homocysteine inhibits von Willebrands factor processing and secretion by preventing transport from the endoplasmic reticulum. Blood 1993; 81: 683–689
Kang SS, Zhoo J, Wong PWK, Kowalisyn J, Strokosch G . Intermediate hyperhomocysteinaemia: a thermolabile varient of methylenetetrahydrofolate reductase. Am J Hum Genet 1988; 43: 414–421
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 1995; 10: 111–113
Rozen R . Genetic predisposition to hyperhomocysteinaemia: deficiency of methylenetetrahydrofolate reductase. Throm Haemostsat 1997; 78: 523–526
Jacques PF, Bostom AG, Williams RR, Ellison RC, Eckfeldt JH, Rosenberg IH et al. Relation between folate status, a common mutation in methylenetetrahydrofolate reductase, and plasma homocysteine concentrations. Circulation 1996; 93: 7–9
Graham IM, Daly LE, Refsum HM et al. Plasma homocysteine as a risk factor for vascular disease. JAMA 19997; 277: 1775–1781
De Stefano V, Zappacosta B, Persichilli S, Rossi E, Casorelli I, Paciaroni K et al. Prevalence of mild hyperhomocysteinaemia and association with thrombophilic genotypes (factor V Leiden and prothrombin G20210A) in Italian patients with venous thromboembolic disease. Br J Haematol 1999; 106: 564–568
Loewnstein A, Goldstein M, Winder A, Lazar M, Eldor A . Retinal vein occlusion associated with methylenetetrahydrofolate reductase mutation. Ophthalmology 2000; 106: 1817–1820
Vine AK . Hyperhomocysteinaemia: a risk factor for retinal vein occlusion. Am J Ophthalmol 2000; 129: 640–644
Cahill M, Karabatzaki M, Meleady R, Refsum H, Ueland P, Shields D et al. Raised plasma homocysteine as a risk factor for retinal vascular occlusive disease. Br J Ophthalmol 2000; 84: 154–157
Martin SC, Rauz S, Marr JE, Martin N, Jones AF, Dodson PM . Plasma total homocysteine and retinal vascular disease. Eye 2000; 14: 590–593
Wenzler EM, Rademakers AJ, Boers GH, Cruysberg JR, Webers CA, Deutman AF . Hyperhomocysteinaemia in retinal artery and retinal vein occlusion. Am J Ophthalmol 1993; 115: 1162–1167
Mclean JW, Tomlinson JE, Kuang WJ, Eaton DL, Chen EY, Fless GM et al. CDNA sequence of human apolipoprotein (a) is homologous to plasminogen. Nature 1987; 330: 132–137
Tsaloumas MD, Kirwin J, Vinall H, O’Leary MB, Prior P, Kritzinger EE et al. Nine year follow-up study of morbidity and mortality in retinal vein occlusion. Eye 2000; 14: 821–827
Hayreh SS, Zimmermann MB, Podhajsky P . Incidence of various types of retinal vein occlusion and their recurrence and demographic characteristics. Am J Ophthalmol 1994; 117: 429–441
Dodson PM, Kritzinger EE . Medical cardiovascular treatment trials: relevant to medical ophthalmology in 1997?. Eye 1997; 11: 3–11
Jacobsen DW . Homocysteine and vitamins in cardiovascular disease. Clin Chem 1998; 44: 1833–1843
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fegan, C. Central retinal vein occlusion and thrombophilia. Eye 16, 98–106 (2002). https://doi.org/10.1038/sj.eye.6700040
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700040
Keywords
This article is cited by
-
Choroidal infarction following ophthalmic artery chemotherapy
International Journal of Retina and Vitreous (2018)
-
Venous thromboembolism does not share familial susceptibility with retinal vascular occlusion or glaucoma: a nationwide family study
Journal of Thrombosis and Thrombolysis (2016)
-
Genetic polymorphisms and their association with central retinal vein occlusion combined with cilioretinal artery occlusion
Comparative Clinical Pathology (2015)
-
Central Retinal Vein Occlusion Secondary to Protein S Deficiency
Annals of Ophthalmology (2007)
-
Recurrent branch retinal vein occlusion with factor V leiden mutation
Eye (2006)