Abstract
Background:
To evaluate the impact of treatment on health states that affect patients’ quality of life in advanced follicular lymphoma.
Methods:
A quality-adjusted time without symptoms of disease or toxicity of treatment (Q-TwiST) analysis was performed on data from a phase III clinical trial (Marcus et al, 2008).
Results:
Cyclophosphamide, vincristine, and prednisone plus rituximab (R-CVP)-treated patients gained a mean of 15.17 months in TWiST, 8.33 months in Q-TwiST, and 11.30 months less in disease relapse, without increase in toxicity compared with cyclophosphamide, vincristine, and prednisone (CVP)-treated patients.
Conclusion
Rituximab plus CVP-treated patients reached a significant and clinically meaningful improvement within 12 months in quality-adjusted survival compared with CVP.
Similar content being viewed by others
Main
Follicular lymphoma (FL) is the most common form of non-Hodgkin's lymphoma (NHL), accounting for about 70% of indolent lymphomas and 20–25% of all cases of NHL (NHL classification project, 1997). Follicular lymphoma is characterised by slow disease progression and exhibits repeated chemotherapy-induced remissions followed by relapses, with times of remission and a median survival of 6–10 years (Horning, 1993), depending on the stage of disease and other prognostic variables at diagnosis. An open-label, randomised, multi-centre phase III trial investigated the clinical outcomes of previously untreated FL patients who received eight cycles of cyclophosphamide, vincristine, and prednisone (CVP) vs eight cycles of CVP plus rituximab (R-CVP) therapy (Marcus et al, 2005). The recently published 53-month median follow-up data showed that R-CVP-treated patients experienced clinically significant improvements in time to treatment failure and overall survival (OS), without an increase in clinically significant toxicity (Marcus et al, 2008). Although treatment goals for FL include freedom from symptomatic disease and toxicity-related impairment of quality of life (QoL), no QoL parameters were collected in this trial.
It is reasonable to assume that patients with no disease symptoms or treatment toxicity will have better health-related quality of life (HR-QoL) than those exhibiting disease symptoms and toxicity. Our objective was to conduct a quality-adjusted time without symptoms of disease or toxicity of treatment (Q-TWiST) analysis on the 53-month follow-up data from the phase III trial (Marcus et al, 2008). The Q-TWiST method was initially used to evaluate adjuvant therapies for breast cancer (Fairclough et al, 1999), and has since been applied to trials of interferon in advanced FL (Cole et al, 1998) and multiple myeloma (Zee et al, 1998).
Materials and methods
Patient population and treatment comparators
The design and main results of the phase III randomised, controlled clinical trial have been reported elsewhere (Marcus et al, 2005, 2008).
Analyses were conducted on all patients who received at least one administration of study medication. Patients were randomly assigned to R-CVP (n=162) or CVP alone (n=159). Patients treated with CVP alone received a combination of cyclophosphamide 750 mg m−2 i.v. on day 1; vincristine 1.4 mg m−2, up to a maximal dose of 2 mg i.v. on day 1; and prednisone 40 mg m−2 p.o. on days 1–5. Patients treated with R-CVP also received rituximab 375 mg m−2 i.v. on day 1 of each treatment cycle (length 21 days). Patients were treated for a maximum of eight cycles.
Q-TWiST analysis
The Q-TWiST analysis was performed on the 321 patients and consisted of three steps (Staquet et al, 1998; Fayers and Machin, 2000).
Step 1: Definition of clinical health states
The clinical health states considered relevant to treatment decision-making in patients with FL were as follows: TOX – the time period with treatment-related adverse events; REL – the time period with disease relapse (progression), ending with death or censoring; and TWiST – the time period during which patients experienced no disease symptoms or treatment toxicities, thus reflecting the best possible patient HR-QoL in this clinical setting.
This Q-TWiST analysis was performed using all investigator-determined treatment-related adverse events occurring from the start of treatment until 28 days beyond the last protocol-defined dose or progression. Although there was a higher incidence of grade 3–4 neutropenia during treatment with R-CVP, this did not translate into a higher infection rate (Marcus et al, 2005, 2008).
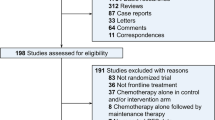
Step 2: Estimation of health state duration
Mean duration of OS partitioned into health states TOX, TWiST, and REL was estimated from the phase III trial data (Marcus et al, 2008). Owing to the shorter follow-up in the CVP arm, the event data were truncated to 67 months, the longest follow-up in the shortest progression-free curve of the comparator, to exclude follow-up time bias in favour of R-CVP. The mean duration of toxicity was calculated without restriction, whereas the mean time spent in REL and TWiST was restricted to the clinical follow-up period. These estimates are represented by the area between the partitioned curves (Figure 1).
Partitioned survival plots for (A) R-CVP and (B) CVP alone. Curves represent overall survival (OS), progression-free survival (PFS), and treatment toxicity (TOX). Areas between the curves represent the mean time spent in the health states: TOX, time without disease symptoms or treatment toxicity (TWiST), and time in relapse (REL), based on 53 months’ median follow-up truncated at 67 months.
Step 3: Estimation of Q-TWiST
A quality-adjusted survival model was developed with the use of utility coefficients for uTOX, uTWiST, and uREL to reflect the impact on the patient's HR-QoL. The utility coefficients are measured on a scale from 0 to 1, where 0 represents death and 1 represents the best possible patient QoL. Quality-adjusted time without disease symptoms or toxicities of treatment, defined as the weighted sum of time spent in each disease state is calculated as:

The utility weight of 0.618 (s.e., 0.056) used for REL was obtained from the UK study in 222 patients with FL (Pettengell et al, 2008). The base case Q-TWiST analysis assumed a TWiST utility of 1.0 and a utility of 0.618 for REL and TOX.
Statistical analysis
Point estimates of mean differences in OS, progression-free survival (PFS), disease relapse (REL=OS–PFS), TWiST (TWiST=PFS–TOX), and duration of TOX were calculated from patient follow-up data. Owing to the unknown distributions of the mean differences, non-parametric bootstrapping, a numerical resampling method, was performed (5000 iterations) to obtain reliable estimates of the s.e. for the clinical end points (Fine and Gelber, 2001). P-values with 95% CI were reported on the basis of the standard Z-statistic.
Threshold utility analysis
A threshold utility analysis assessed the Q-TWiST outcome over seven possible combinations of TOX and REL utility values with the TWiST utility set to 1.0 or 0.805 from the UK utility study (Pettengell et al, 2008).
Probabilistic sensitivity analysis
Probabilistic sensitivity analysis (PSA) was performed to address the uncertainty of the clinical end points and the co-dependency between utilities and the health states. This was carried out using Monte Carlo simulations (1000 iterations), in which OS, PFS, REL, and TOX utilities were randomly sampled from Beta-Pert distributions (Vose, 2000), with the most likely and extreme values obtained from the mean and s.e. reported in the 53-month update (Marcus et al, 2008) and the UK utility study (Pettengell et al, 2008).
Results
Q-TWiST analysis
Survival times partitioned into the three health states are shown separately for R-CVP and CVP in Figure 1A and B, depicting the time spent in each health state over the follow-up period. Rituximab plus CVP-treated patients gained a mean of 15.17 months TWiST (P<0.001), and spent a mean of 11.30 months less time in relapse (P<0.001) compared with CVP patients, without any increase in toxicity (mean difference 0.24 months (P=0.36; Table 1). Using the patient-reported utility of 0.618 for REL, an assumed utility of 0.618 for TOX, and a utility of 1.0 for TWiST, R-CVP patients experienced a mean of 8.33 months’ longer Q-TWiST compared with CVP (95% CI 4.51–9.25, P<0.001) (Table 1). On the basis of PSA, the mean increase in Q-TWiST for R-CVP compared with CVP was 7.38 (95% CI: 5.82–10.87), which is consistent with the bootstrapped estimates.
Utility threshold analysis
Results from the threshold utility analysis show that in all cases but one, the mean increases in Q-TWiST obtained with R-CVP vs CVP were statistically significant (Table 2).
Gain function
The gain function (Staquet et al, 1998; Fayers and Machin, 2000), defined as the incremental mean differences in Q-TWiST between R-CVP and CVP over time, is shown in Figure 2.
Gain function of incremental mean differences in Q-TWiST between R-CVP and CVP as a function of time (53 months’ median follow-up truncated at 67 months). The solid line represents the incremental mean differences in Q-TWiST over time with utilities 0.618 for TOX and REL and 1.0 for TWiST, whereas the shaded area depicts the range of differences in Q-TWiST, as the utility values for REL and TOX vary between 0 and 1.
Discussion
Comparative clinical and health outcomes
Long-term follow-up data (Marcus et al, 2008) showed statistically significant and clinically meaningful improvement for R-CVP over CVP in time to treatment failure and PFS, without an increase in clinically significant toxicity. Furthermore, OS for patients treated with R-CVP was significantly longer than for patients treated with CVP alone (Marcus et al, 2008). Quality-adjusted time without disease symptoms or toxicity of treatment analysis based on this 53-month update to the data shows that patients treated with R-CVP gained more time without treatment toxicities or disease symptoms and spent less time in relapse than did patients treated with CVP alone. Incorporating patient-reported utilities from the UK study in FL (Pettengell et al, 2008) confirmed the significant improvement in quality-adjusted survival with R-CVP vs CVP alone.
In their investigation of clinically important differences in Q-TWiST analyses, Revicki et al (2006) suggested that differences of 10–15% should be regarded as clinically important. A 15% increase in Q-TWiST was obtained with R-CVP vs CVP alone representing a clinically meaningful difference, with an 11% (mean 6.11 months) difference achieved within 12 months.
A previous Q-TWiST analysis comparing CHVP with CHVP plus IFN-α2b in 242 patients with FL (Cole et al, 1998) showed that after a median follow-up of 72 months, the IFN group gained a mean of 12.3 months’ PFS and 7.4 months’ OS, but experienced additional time with grade 3 or worse toxicity, compared with the CHVP group. In contrast, our study with 53 months’ median follow-up revealed that R-CVP treatment resulted in a mean increase in PFS of 15.4 months, a mean of 11.30 months’ less time spent in relapse, with no significant increase in toxicity vs CVP alone.
Strengths and weaknesses
In the threshold utility analysis, the increase in Q-TWiST was not statistically significant with the utility combination 0.90, 0.10 and 0.805 for REL, TOX and TWiST respectively (Table 2). However, it is clinically unlikely that the QoL of FL patients who have relapsed would be better than that of patients without symptoms or toxicity.
The bootstrap analysis incorporated uncertainty in the clinical end points used to estimate Q-TWiST using deterministic utility values. Probabilistic sensitivity analysis, by addressing the relationship between OS, PFS, REL, TOX, and utilities, represents a comprehensive sensitivity analysis to test the robustness of the Q-TWiST outcome.
The UK utility study did not investigate patient utilities for TOX. However, as there was no significant difference in the duration of toxicity between the treatment arms, the Q-TWiST results were insensitive to this utility. Finally, a median 53-month follow-up period is relatively short given that patients with FL have a median survival of 6–10 years (Horning, 1993). Parametric extrapolation of the clinical data beyond this period is one approach for determining whether R-CVP will further augment quality-adjusted survival.
Conclusions
Rituximab plus CVP-treated patients with advanced FL reached a significant and clinically meaningful improvement within 12 months in quality-adjusted survival compared with CVP alone.
Conflict of interest
The study described was funded by F. Hoffmann-La Roche Ltd, Basel, Switzerland. R Aultman and F Jost are employees of F. Hoffmann-La Roche; R Marcus has provided ad hoc consulting services for F. Hoffmann-La Roche, and has received honoraria and attended paid Advisory Boards for F. Hoffmann-La Roche.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Cole BF, Solal-Celigny P, Gelber RD, Lepage E, Gisselbrecht C, Reyes F, Sebban C, Sugano D, Tendler C, Goldhirsch A (1998) Quality-of-life-adjusted survival analysis of interferon alfa-2b treatment for advanced follicular lymphoma: an aid to clinical decision making. J Clin Oncol 16: 2339–2344
Fairclough DL, Fetting JH, Cella D, Wonson W, Moinpour CM (1999) Quality of life and quality adjusted survival for breast cancer patients receiving adjuvant therapy. Eastern Cooperative Oncology Group (ECOG). Qual Life Res 8: 723–731
Fayers PM, Machin D (2000) Quality of Life. Assessment, Analysis and Interpretation. Wiley: Chichester, pp xii +404. ISBN 0-471-96861-7
Fine JP, Gelber RD (2001) Joint regression analysis of survival and quality-adjusted survival. Biometrics 57: 376–382
Horning SJ (1993) Natural history of and therapy for the indolent non-Hodgkin's lymphomas. Semin Oncol 20: 75–88
Marcus R, Imrie K, Belch A, Cunningham D, Flores E, Catalano J, Solal-Celigny P, Offner F, Walewski J, Raposo J, Jack A, Smith P (2005) CVP chemotherapy plus rituximab compared with CVP as first-line treatment for advanced follicular lymphoma. Blood 105: 1417–1423
Marcus R, Imrie K, Solal-Celigny P, Catalano JV, Dmoszynska A, Raposo JC, Offner FC, Gomez-Codina J, Belch A, Cunningham D, Wassner-Fritsch E, Stein G (2008) Phase III study of R-CVP compared with cyclophosphamide, vincristine, and prednisone alone in patients with previously untreated advanced follicular lymphoma. J Clin Oncol 26: 4579–4586
Pettengell R, Donatti C, Hoskin P, Poynton C, Kettle PJ, Hancock B, Johnson S, Dyer MJ, Rule S, Walker M, Wild D (2008) The impact of follicular lymphoma on health-related quality of life. Ann Oncol 19: 570–576
Revicki DA, Feeny D, Hunt TL, Cole BF (2006) Analyzing oncology clinical trial data using the Q-TWiST method: clinical importance and sources for health state preference data. Qual Life Res 15: 411–423
Staquet MJ, Hays RD, Fayers PM (eds) (1998) Using the Q-TWiST Method for Treatment Comparisons in Clinical Trials. Oxford University Press: USA, pp 281–296
The Non-Hodgkin's Lymphoma Classification Project (1997) A clinical evaluation of the International Lymphoma Study Group classification of non-Hodgkin's lymphoma. Blood 89: 3909–3918
Vose D (2000) Risk Analysis – A Quantitative Guide 2nd edn, John Wiley & Sons: Chichester
Zee B, Cole B, Li T, Browman G, James K, Johnston D, Sugano D, Pater J (1998) Quality-adjusted time without symptoms or toxicity analysis of interferon maintenance in multiple myeloma. J Clin Oncol 16: 2834–2839
Acknowledgements
The programs used for data analysis as well as the results of the Q-TWiST analysis were independently reproduced by Professor Dr Jürgen Bock as part of the validation exercise. R Marcus was the primary investigator for the phase III trial and worked as a consultant for F. Hoffmann-La Roche. R Aultman designed and performed the research, analysed the data, and wrote the paper. F Jost participated in the design and analysis of the study and assisted in writing the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Marcus, R., Aultman, R. & Jost, F. A quality-adjusted survival analysis (Q-TWiST) of rituximab plus CVP vs CVP alone in first-line treatment of advanced follicular non-Hodgkin's lymphoma. Br J Cancer 102, 19–22 (2010). https://doi.org/10.1038/sj.bjc.6605443
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605443
Keywords
This article is cited by
-
Q-TWiST analysis comparing ipilimumab/dacarbazine vs placebo/dacarbazine for patients with stage III/IV melanoma
British Journal of Cancer (2013)
-
Q-TWiST analysis to estimate overall benefit for patients with metastatic renal cell carcinoma treated in a phase III trial of sunitinib vs interferon-α
British Journal of Cancer (2012)