Abstract
A substantial part of all hereditary breast cancer cases is caused by BRCA1 germline mutations. In this review, we will discuss the insights into BRCA1 functions that we obtained from mouse models with conventional and conditional mutations in Brca1. The most advanced models closely resemble human BRCA1-related breast cancer and may therefore be useful for addressing clinically relevant questions.
Similar content being viewed by others
Main
Breast cancer is by far the most frequent cancer in women, accounting for over 20% of all cancer cases. Familial breast cancers, including those associated with heterozygous germline mutations in the major susceptibility genes BRCA1 and BRCA2, account for 5–10% of breast cancer cases in the western world. BRCA1 mutation carriers have a lifetime risk of about 80% for developing breast cancer and a 40% lifetime risk for developing ovarian cancer. Most BRCA1-associated tumours show loss of heterozygosity (LOH) at the BRCA1 locus, leading to loss of the wild-type allele, which is consistent with a tumour suppressor function of BRCA1 (Narod and Foulkes, 2004).
Since the discovery of the BRCA1 gene in 1994 (Miki et al, 1994), several genetically engineered mouse models have been generated for studying the in vivo functions of BRCA1. Initial studies used conventional knockout mice with germline mutations in the mouse Brca1 gene. These conventional Brca1 mouse mutants have enabled us to learn a lot about the biological roles of BRCA1. Because of the embryonic lethality of homozygous animals carrying two defective Brca1 alleles and the lack of mammary tumour development in heterozygous mice carrying one defective and one wild-type Brca1 allele, these models could not be used to study the role of BRCA1 in tumorigenesis. To overcome these problems, the investigators generated conditional Brca1 knockout mice that enable tissue-specific inactivation of BRCA1 by Cre recombinase-mediated deletion of one or more Brca1 exons flanked by loxP recombination sites (Jonkers and Berns, 2002). The most recently developed conditional Brca1 mammary tumour models closely mimic several important aspects of human BRCA1-associated breast cancer and therefore serve as important tools for the development of novel therapies for this disease. Before elaborating on the Brca1 conventional and conditional mouse models that have been generated to date, we will discuss the characteristics of human BRCA1-related breast cancer in more detail.
Human BRCA1-associated breast cancer
BRCA1-associated breast tumours are mostly high-grade invasive ductal carcinomas (IDCs) that lack expression of estrogen receptor (ER), progesterone receptor (PR) and ERRB2/HER2, which is referred to as ‘triple-negative’ breast cancer (Johannsson et al, 1997). Consequently, most patients with BRCA1-mutated breast cancer do not benefit from therapeutics that target ER- or ERBB2/HER2-expressing tumour cells. Gene expression profiling revealed a strong resemblance between BRCA1-mutated tumours and sporadic basal-type breast cancer (Sorlie et al, 2003). BRCA1-related tumours commonly express basal cytokeratins (CK5, CK6, CK14 and CK17), are highly proliferative and show pushing margins (Foulkes et al, 2003). BRCA1-mutated tumours also show a significantly higher degree of genomic instability than sporadic breast cancers (Tirkkonen et al, 1997), which is likely because of the functions of BRCA1 in cell-cycle regulation and DNA repair (see below).
Mutations in BRCA1 are not confined to certain functional domains, but are scattered throughout the gene (Breast Cancer Information Core; http://research.nhgri.nih.gov/bic/). Approximately half of all BRCA1 mutations are protein-truncating or deleterious missense mutations, whereas the pathogenic potential of the remainder is unknown (Chenevix-Trench et al, 2006).
Mutations in the tumour suppressor gene TP53 are more frequent in BRCA1-associated breast tumours than in sporadic cases (Greenblatt et al, 2001), mainly because of a selective increase in protein-truncating TP53 mutations (Holstege et al, 2009; Manié et al, 2009).
Insights into the biological functions of BRCA1
BRCA1 has been implicated in a remarkably broad range of cellular processes and has also been reported to interact with a large number of different proteins. In this section, we will briefly describe some of the known functions of BRCA1 and also review some recent data that point towards the novel functions of BRCA1.
First, BRCA1 has been found to co-localise and interact with proteins involved in DNA repair, such as RAD51 (Scully et al, 1997). This interaction led to the suggestion that BRCA1 is involved in the maintenance of genomic stability through a function in DNA damage repair. The direct proof for this notion was provided by Moynahan et al (1999), who showed that BRCA1-deficient mouse embryonic stem (ES) cells are impaired in homology-directed repair of DNA double-strand breaks (DSBs). Further indications for a role of BRCA1 in DNA repair are the increased chromosomal instability and high sensitivity to DNA-damaging agents of BRCA1-deficient cells (Kennedy et al, 2004).
Besides its role in DNA repair, BRCA1 has been implicated in transcriptional regulation (through its interaction with RNA polymerase II and known transcription factors), cell-cycle progression (Deng, 2006), ubiquitination and chromatin remodelling (Mullan et al, 2006), as well as in maintenance of X-chromosome inactivation (Ganesan et al, 2002).
Recent work in the group of Wicha revealed that BRCA1 may have a role in the differentiation of ER-negative stem/progenitor cells to ER-positive luminal cells (Liu et al, 2008). Inhibition of BRCA1 in primary breast epithelial cells by RNA interference leads to an increase in ALDH1-positive stem/progenitor cells and a decrease in ER-positive luminal cells. Thus, loss of BRCA1 seems to induce a block in epithelial differentiation and expansion of the undifferentiated stem/progenitor cell compartment. These results might explain why most BRCA1-mutated breast tumours have an undifferentiated basal-like phenotype.
Conventional BRCA1 mouse models
A range of conventional Brca1 knockout mouse models has been generated in an attempt to study the effects of BRCA1 loss. Until now, a total of 10 different conventional Brca1 mouse mutants have been generated and characterised, each carrying a mutation in a different part of the gene (Xu et al, 1999b; Evers and Jonkers, 2006; Kim et al, 2006). In contrast to women with heterozygous BRCA1 germline mutations, none of the heterozygous Brca1 mouse mutants developed spontaneous mammary tumours. Although the reason for this inconsistency is still unclear, it could point to a species difference: the lifespan of a mouse might simply be too short or the rate of LOH might be too low for heterozygous Brca1 mice to acquire additional mutations necessary for tumour development. Alternatively, there might be (tissue-specific) differences in haplo-insufficiency of the heterozygous Brca1 allele between humans and mice. Embryonic lethality is observed for most homozygous Brca1 mouse mutants. In line with the embryonic lethality of Brca1 mouse mutants, no homozygous BRCA1 mutation carriers have been described (Kuschel et al, 2001).
Most homozygous Brca1 mouse mutants die at mid-gestation, between embryonic day 7.5 and 13.5, due to reduced cellular proliferation without signs of increased apoptosis (Evers and Jonkers, 2006). The variation in time point and penetrance of embryonic lethality could be a consequence of different genetic backgrounds of various Brca1 mouse strains. However, the differences in protein truncation and alternative splicing of Brca1 could also have an important role in the observed phenotypic variation between these models. A comprehensive characterisation of the regulation and function of alternative splice variants is necessary for accurate interpretation of the different Brca1 mutant phenotypes. Evolutionary conservation may be a good indication for the functionality of specific splice variants. Thus far, three Brca1 splice variants have been shown and functionally analysed in mice: Brca1-Δ11 (Xu et al, 1999b; Kim et al, 2006), Brca1-Iris and Brca1-Δ22 (Pettigrew et al, 2008).
Mouse embryos carrying Brca1 mutations that abolish expression of full-length Brca1 without affecting Brca1-Δ11 expression survive significantly longer than embryos harbouring Brca1 mutations that abolish expression of both transcripts (Evers and Jonkers, 2006). Mouse BRCA1-Δ11, similar to full-length BRCA1, is localised in nuclear foci and shows a cell-cycle-regulated expression pattern (Huber et al, 2001). However, BRCA1-Δ11 is not phosphorylated and does not promote formation of RAD51 foci upon DNA damage. Indeed, homozygous Brca1Tr mouse mutants that express BRCA1-Δ11 are viable on a BALB/c genetic background, but develop various tumours including mammary carcinomas after long latency (Ludwig et al, 2001). Similarly, mice with mammary gland-specific deletion of full-length Brca1 but retention of Brca1-Δ11 develop mammary adenocarcinomas characterised by genetic instability (Xu et al, 1999a). Thus, BRCA1-Δ11 may compensate for some of the functions of full-length BRCA1 during embryogenesis, but is unable to fully execute the functions of full-length BRCA1 in maintenance of genomic stability and tumour suppression.
The BRCA1-IRIS transcript comprises exons 1–11 and a part of intron 11, encoding for a protein with the same N-terminus as full-length BRCA1, but with a unique C-terminus (Elshamy and Livingston, 2004). BRCA1-IRIS was shown to be exclusively chromatin associated and to have a positive influence on DNA replication. Recently, Brca1-Iris, the mouse orthologue of human BRCA1-IRIS, was identified (Pettigrew et al, 2008). Most BRCA1 mouse models generated to date have deleted Brca1-Iris in addition to full-length Brca1 (Evers and Jonkers, 2006). Interestingly, the only Brca1 mutation that disrupts full-length Brca1 and Brca1-Δ11 transcripts but not Brca1-Iris, causes embryonic lethality at E10.5 (Hohenstein et al, 2001), suggesting that BRCA1-IRIS cannot compensate for the loss of full-length BRCA1 and BRCA1-Δ11 expression.
Pettigrew et al (2008) identified BRCA1-Δ22 in both human and mouse cells. Skipping of exon 22 leads to a loss of the second BRCT repeat and functional analysis revealed that the BRCA1-Δ22 protein is no longer capable of transcriptional activation. In line with this, a Brca1 truncation mutant lacking the second BRCT repeat shows a delayed embryonic lethality when compared with Brca1-null mutants (Hohenstein et al, 2001).
Similar to the differences in time point and penetrance of embryonic lethality observed for different Brca1 mouse mutants, the rescue of embryonic lethality by loss of p53 was also subject to phenotypic variation. In Brca1-null mutants, p53 deficiency resulted in only a partial rescue of embryonic lethality (Hakem et al, 1997; Ludwig et al, 1997). In hypomorphic Brca1 mutants, the effects of a Trp53-null or Trp53-heterozygous background were more pronounced, leading to a survival of Brca1 and Trp53 compound mutant mice to adulthood (Cressman et al, 1999; Xu et al, 2001).
In conclusion, several Brca1 conventional mouse mutants have been generated that show phenotypic variation, ranging from early embryonic lethality to viable mice that develop tumours. This phenotypic variation is likely due to the differences in expression of BRCA1 splice variants and BRCA1-IRIS in the various Brca1 mouse mutants.
Conditional BRCA1 mouse models
Although conventional Brca1 mouse models have enabled us to learn a lot about the biological functions of BRCA1, the observed embryonic lethality of homozygous animals and lack of mammary tumour development in heterozygous mice made it difficult to study the role of BRCA1 in tumour suppression. For this purpose, investigators turned to conditional mouse models to study the effects of BRCA1 loss.
To date, five different conditional Brca1 alleles have been generated (Table 1): Brca1F11 (Xu et al, 1999a), Brca1F5–6 (Mak et al, 2000), Brca1F5–13 (Liu et al, 2007), Brca1F22–24 (McCarthy et al, 2007) and Brca1F2 (Shakya et al, 2008). Although Cre-mediated deletion completely abrogates BRCA1 function for the Brca1F5–6, the Brca1F5–13 and the Brca1F22–24 allele, deletion of exon 11 in the Brca1F11 allele does not affect the expression of the BRCA1-Δ11 isoform.
Different tissue-specific promoters were used in combination with these conditional Brca1 alleles to achieve Cre expression in mammary epithelium. Xu et al (1999a) used transgenic mice expressing Cre from the whey acidic protein (WAP) or mouse mammary tumour virus (MMTV) promoter to induce mammary-specific recombination of the Brca1F11 alleles. In both models, different types of mammary tumours developed with a long latency and these tumours showed genomic instability and altered Trp53 expression. The vast majority of these tumours were negative for ER, but a large proportion overexpressed ERBB2 (Table 1). Removal of one Trp53 allele significantly reduced mammary tumour latency (Brodie et al, 2001). These results proved that BRCA1 functions as a tumour suppressor and cooperates with TP53 in tumorigenesis.
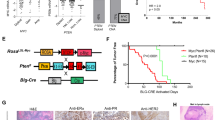
More evidence for interaction of BRCA1 and TP53 in tumorigenesis was provided by our lab. We generated a conditional mouse model with K14cre-mediated deletion of both Brca1 and Trp53 in several epithelial tissues, including mammary epithelium (Liu et al, 2007). Female mice of this strain showed a high incidence of mammary carcinomas that displayed important hallmarks of human BRCA1-associated breast tumours: tumours were poorly differentiated, highly proliferative, genomically instable, ER-negative and showed an increased expression of basal epithelial markers (Table 1).
Another mouse model for basal-like breast cancer was generated by conditional deletion of Brca1 exons 22–24 (which harbour the second BRCT domain) in the mammary gland by using β-lactoglobin (BLG)-cre (McCarthy et al, 2007). When combined with heterozygosity for a Trp53 mutation, this led to mammary tumour formation. The resulting mammary tumours were characterised by high histological grade, central necrotic areas and expression of basal-like markers. In addition, they frequently lacked expression of ER, PR and ERBB2 (Table 1). Because of their strong resemblance to human BRCA1-related breast cancer, especially the mouse models of Liu and McCarthy should prove useful in preclinical therapeutic intervention studies.
BRCA1 also interacts with BARD1, a protein that is structurally related to BRCA1 in that it contains an N-terminal RING domain and C-terminal BRCT repeats (Wu et al, 1996). The BRCA1/BARD1 heterodimer functions as a ubiquitin E3 ligase that can target proteins for destruction by transferring ubiquitin to these proteins (Hashizume et al, 2001). Until recently, the role of the BRCA1/BARD1 heterodimer in tumour suppression had not been evaluated. To address this question, Shakya et al (2008) generated mouse strains carrying conditional alleles of Bard1 and/or Brca1 and used Cre-mediated recombination to inactivate these genes specifically in mammary epithelial cells. Breast tumours arising in these conditional Bard1- and/or Brca1-mutant mice were indistinguishable from each other. These findings indicate that BARD1 itself is a tumour suppressor and that the tumour suppressor activities of BRCA1 are mediated by the BRCA1/BARD1 heterodimer.
Recent experiments have shown that ES cells expressing a ubiquitin ligase-deficient BRCA1-I26A mutant are viable and do not undergo spontaneous chromosomal rearrangements (Reid et al, 2008). These cells show higher levels of genomic rearrangements after mitomycin C (MMC) treatment, but do not show hypersensitivity to MMC. Brca1I26A-mutant ES cells form RAD51 foci in response to irradiation and are capable of repairing double-strand breaks by homologous recombination. These results suggest that the function of BRCA1 in the maintenance of genomic stability is not dependent on its ubiquitin ligase activity. Mouse models carrying ubiquitin ligase-deficient Brca1 alleles should reveal whether this activity is also dispensable for the tumour suppressor activity of BRCA1.
Chemoprevention studies in BRCA1 models
Although genetic testing for inherited BRCA1 mutations provides valuable information to women at high risk of breast cancer, carriers of BRCA1 mutations have few clinical options to reduce their cancer risk. Prophylactic surgery is still one of the most important measures of breast cancer prevention for BRCA1 mutation carriers. The rationale for antihormonal therapy as an alternative for prophylactic surgery comes from the observation that oophorectomy prevents breast cancer in BRCA1 mutation carriers (Narod and Offit, 2005). These data indicate that, despite the fact that most BRCA1-mutated tumours are ER-negative, tumour development in BRCA1 mutation carriers is hormone dependent. This hormone dependency might also be the reason why BRCA1 specifically functions as a tumour suppressor in hormone-sensitive tissues such as breast and ovaries. Although the mechanistic basis for the hormone dependency and tissue specificity of BRCA1-associated tumorigenesis is still unknown, BRCA1 has been shown to interact directly with ER-α and PR and to modulate their transcriptional activities (Fan et al, 1999; Katiyar et al, 2006). To address the role of PR signalling in BRCA1-mediated carcinogenesis, Poole et al (2006) made use of the WAPcre;Brca1F11/F11;Trp53F5–6/F5–6 mouse model. Treatment of 3- to 4-month-old mice with the PR inhibitor mifeprestone (RU 486) prevented mammary tumour formation in these mice. Although the results obtained with this conditional Brca1 mouse model hold promise for the development of anti-progesterones as prophylactic therapy for BRCA1-associated breast cancer, the jury is still out on this for several reasons. First, mifeprestone is not a selective PR antagonist because it also binds with high affinity to glucocorticoid receptors. It is therefore possible that the prevention of mammary tumours is (in part) caused by the antiglucocorticoid effects of mifeprestone. Second, it is not clear whether the mammary tumours arising in this WAPcre;Brca1F11/F11;Trp53F5–6/F5–6 mouse model do or do not express ER, PR and ERBB2. The status of ER, PR and ERBB2 could have an important role in the effectiveness of anti-progesterone therapy. Most human BRCA1-mutated breast cancers are ‘triple-negative’ tumours that do not express ER, PR and ERBB2. It is unclear whether anti-progesterone therapy will also protect against development of triple-negative breast tumours in BRCA1-mutation carriers. It may therefore be important to evaluate the effects of PR antagonists in Brca1 mouse models that certainly recapitulate development of triple-negative BRCA1-associated breast cancer.
Chemotherapeutic interventions in BRCA1 models
Breast cancers of BRCA1 mutation carriers frequently show poor responses to neoadjuvant therapy with docetaxel, whereas platinum-based chemotherapy seems to be highly effective (Byrski et al, 2008, 2009). Similarly, BRCA1/2 mutation carriers with ovarian cancer show higher response rates and longer overall survival after platinum-based chemotherapy than nonhereditary patients (Ben David et al, 2002; Tan et al, 2008).
Unfortunately, the experiments studying drug response and especially drug resistance in human patients are very time consuming. With regard to this time issue, conditional Brca1 mouse models that develop mammary tumours with strong resemblance to human BRCA1-mutated breast tumours (Liu et al, 2007; McCarthy et al, 2007) can be very helpful in predicting response and resistance to conventional and targeted therapeutics. Our K14cre;Brca1F5–13/F5–13;Trp53F2–10/F 2–10 mouse model was used for studying responses to various conventional chemotherapeutics, such as doxorubicin, docetaxel and cisplatin, and for analysing the mechanisms of acquired resistance (Rottenberg et al, 2007). Similar to the human situation, heterogeneity in the response of individual mouse mammary tumours was observed, but eventually all tumours became resistant to doxorubicin and docetaxel. The upregulation of ATP-binding cassette (ABC) drug transporters seemed to be the main mechanism responsible for resistance to doxorubicin. Remarkably, acquired resistance to platinum compounds was never observed. However, the tumours could also not be completely eradicated; even after dose-dense platinum therapy, the tumours appeared to regrow from a small fraction of surviving cells. Currently, these platinum-resistant tumour remnants are being further characterised. In addition, attempts are being made to achieve eradication of this small fraction of surviving cells by combination therapies.
Especially intriguing is the observation that platinum resistance is never observed in these mouse tumours, whereas resistance is a major problem in the clinic. As described earlier, BRCA1 has an important role in the error-free repair of double-stranded DNA breaks that occur after platinum therapy. These mouse tumour data raise the question whether platinum resistance can occur at all in BRCA1-deficient tumours that are completely defective in homology-directed DNA repair. This question became even more evident when Swisher et al (2008) showed that acquired resistance to platinum compounds in BRCA1-mutated human ovarian tumours is associated with secondary mutations in BRCA1 that restore the open-reading frame in platinum-resistant tumours. Three out of five platinum-resistant tumours showed secondary genetic changes in BRCA1, whereas no BRCA1 alterations were observed in three platinum-sensitive tumours. The main difference between the human situation and the K14cre;Brca1F5–13/F5–13;Trp53F2–10/F 2–10 mouse model is that the mouse tumours have a homozygous deletion of Brca1 exons 5–13. As a result of this large deletion, secondary mutations in Brca1 cannot restore Brca1 function and serve as a mechanism for platinum resistance in the mouse tumours. Together, the human and mouse data suggest that BRCA1 not only functions as a tumour suppressor, but is also required for development of resistance to therapy.
Intervention studies with conventional chemotherapeutics were also carried out in WAPcre;Brca1F11/F11;Trp53F5–6/F5–6 and MMTVcre;Brca1F11/F11;Trp53F5–6/F5–6 models (Shafee et al, 2008). In line with data obtained from the K14cre;Brca1F5–13/F5–13;Trp53F2–10/F 2–10 model, Brca1Δ11/Δ11;Trp53Δ5–6/Δ5–6 tumours also responded better to platinum compounds than to doxorubicin. Following initial regression, tumours relapsed at the same site at 2–3 months after treatment. Whereas platinum resistance was never observed in the K14cre;Brca1F5–13/F5–13;Trp53F2–10/F 2–10 model, Shafee et al (2008) observed platinum resistance in their Brca1F11/F11;Trp53F5–6/F5–6 models. After a second round of treatment with platinum drugs, tumours recurred with a faster growth rate. This rapid recurrence could suggest the existence of a population of platinum-resistant cells that are selected during a second round of platinum treatment. An important difference between the two studies described above is that Rottenberg et al (2007) used a mouse model with a conditional Brca1 null allele, whereas Shafee et al (2008) used a Brca1 hypomorphic allele that still expresses the Brca1-Δ11 isoform after Cre-mediated deletion of exon 11. Furthermore, the platinum treatment regime differs considerably between the two studies. It would be informative to see whether Brca1Δ11/Δ11;Trp53Δ5–6/Δ5–6 tumours would acquire full resistance to platinum drugs during additional rounds of therapy and if so, by which mechanism.
Interventions with targeted therapeutics in BRCA1 models
Until now, targeted therapeutics are only available for ER- and ERBB2-positive breast cancer, and no tailored therapy exists for triple-negative breast cancer. As mentioned earlier, BRCA1 deficiency causes defects in homology-directed DSB repair. A few years back, BRCA1/2-deficient cells were shown to be highly sensitive to chemical inhibitors of Poly(ADP-ribose) polymerase-1 (PARP1), a key molecule in the repair of DNA single-strand breaks (SSBs) (Farmer et al, 2005). It is thought that, upon inactivation of SSB repair by PARP inhibition, DSBs are induced by replication fork collapse at SSBs during S phase. Therefore, PARP inhibition may be synthetically lethal with BRCA1 loss and serve as a specific therapy for BRCA1-mutated tumours. The K14cre;Brca1F5–13/F5–13;Trp53F2–10/F2–10 mouse model was used to study the effects of PARP inhibition in a ‘realistic’ in vivo setting (Rottenberg et al, 2008). The BRCA1-deficient tumours arising in this model showed a prolonged response to the clinical PARP inhibitor olaparib without signs of toxicity. Eventually, long-term treatment with olaparib resulted in resistance as a consequence of upregulation of the P-glycoprotein drug efflux pump. Combining platinum therapy with PARP inhibition increased the relapse-free survival as compared with platinum monotherapy, suggesting that PARP inhibition enhances the effects of DNA-damaging agents. Recently, it was shown that olaparib has antitumour activity in patients with BRCA1- or BRCA2-associated malignancies (Fong et al, 2009). These findings illustrate how Brca1 conditional mouse models can be of use for preclinical assessment of new targeted therapeutics.
Next-generation BRCA1 models
Despite the fact that current Brca1 mouse models have enabled us to learn a lot about BRCA1 function in normal development and tumorigenesis, improvements can still be made.
For instance, nearly all existing mouse models for BRCA1-associated breast cancer described earlier are based on co-mutation of Trp53 and Brca1. It might be possible that mutations in yet other genes, such as Pten (Saal et al, 2008), are required to effectively model BRCA1-mutated breast cancer in mice.
Current Brca1 mouse models are also not ideally suited to study mechanisms of acquired resistance to conventional and targeted therapeutics. Rottenberg et al (2007, 2008) showed that upregulation of drug efflux pumps is the most prevalent mechanism of acquired resistance to conventional and targeted therapies for mammary tumours arising in the K14cre;Brca1F5–13/F5–13;Trp53F2–10/F2–10 mouse model. Currently, the treatment responses in this K14cre;Brca1F/F;Trp53F/F mouse model are being studied in a P-glycoprotein-deficient background to unravel P-glycoprotein-independent mechanisms of drug resistance (Table 2).
Mouse models based on deleterious missense or protein-truncating Brca1 mutations that closely mimic human BRCA1 germline mutations will be useful for studying tumorigenesis, treatment responses and acquired resistance associated with known pathogenic BRCA1 mutations. These mouse models could, for example, be used for studying the role of genetic reversion in therapy resistance (Table 2). As the number of therapy-resistant tumour samples from patients with specific BRCA1 founder mutations is low, the mouse models carrying these mutations could offer a larger platform to study if and how the genetic reversion occurs as a mechanism of drug resistance for different BRCA1 founder mutations. Eventually, insights gained from mouse models carrying specific Brca1 mutations could lead to tailored therapy for people with a particular BRCA1 mutation.
Another option is to study the consequences of individual mutations in the human BRCA1 gene in vivo by creating mice that express human BRCA1. Already in 2001 it was shown that human BRCA1 is able to rescue embryonic lethality in Brca1 knockout mice (Chandler et al, 2001). This shows that it may be possible to introduce human BRCA1 BAC clones harbouring specific mutations in an intact animal model system. This system would provide the best possible in vivo analysis of the phenotypic consequences of specific BRCA1 mutations.
Concluding remarks
Genetically engineered mouse models for BRCA1 deficiency have proven to be of critical importance for gathering insights on the diverse biological functions of BRCA1, both in normal development and tumorigenesis. In the past years, these mouse models have been further improved to recapitulate the salient features of human BRCA1-associated breast cancer, such as ‘triple-negative’ status, increased genomic instability and increased expression of basal epithelial markers.
Recapitulation of these characteristics in mouse models is crucial for preclinical development of chemoprevention strategies and tailored therapies for BRCA1-associated breast cancer. The first studies with targeted therapeutics in validated BRCA1 models have been conducted, showing excellent initial responses but P-glycoprotein-mediated drug resistance upon prolonged treatment with the PARP inhibitor olaparib (Rottenberg et al, 2008). Of course, it is important to keep in mind that data obtained from mouse tumour models are not necessarily predictive for clinical responses and acquired resistance in human cancer patients. Although genetically engineered mice for BRCA1 deficiency are promising preclinical models, their predictive value remains to be determined.
The PARP inhibitor olaparib was recently evaluated in a phase I clinical trial and showed antitumour activity in BRCA1 or BRCA2 mutation carriers with ovarian, breast or prostate cancer (Fong et al, 2009). In this case, the mouse data did seem to reflect the clinical response quite accurately. It will be of great interest to see whether the acquired resistance to the PARP inhibitor that we observe in the mouse model will also arise in the human situation.
Of course, current mouse models are not perfect yet and can still be further improved to closely mimic additional aspects of human BRCA1-related breast cancer, to study, for example, the role of genetic reversion in therapy resistance. It can be expected that the resulting models will be of even greater use in the development of therapies directed against various aspects of the disease.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ben David Y, Chetrit A, Hirsh-Yechezkel G, Friedman E, Beck BD, Beller U, Ben-Baruch G, Fishman A, Levavi H, Lubin F, Menczer J, Piura B, Struewing JP, Modan B (2002) Effect of BRCA mutations on the length of survival in epithelial ovarian tumors. J Clin Oncol 2: 463–466
Brodie SG, Xu X, Qiao W, Li WM, Cao L, Deng CX (2001) Multiple genetic changes are associated with mammary tumorigenesis in Brca1 conditional knockout mice. Oncogene 20: 7514–7523
Byrski T, Gronwald J, Huzarski T, Grzybowska E, Budryk M, Stawicka M, Mierzwa T, Szwiec M, oelig;niowski R, Siolek M, Narod SA, Lubinski J (2008) Response to neo-adjuvant chemotherapy in women with BRCA1-positive breast cancers. Breast Cancer Res Treat 108: 289–296
Byrski T, Huzarski T, Dent R, Gronwald J, Zuziak D, Cybulski C, Kladny J, Gorski B, Lubinski J, Narod SA (2009) Response to neoadjuvant therapy with cisplatin in BRCA1-positive breast cancer patients. Breast Cancer Res Treat 115: 359–363
Chandler J, Hohenstein P, Swing DA, Tessarollo L, Sharan K (2001) Human BRCA1 gene rescues the embryonic lethality of Brca1 mutant mice. Genesis 29: 72–77
Chenevix-Trench G, Healey S, Lakhani S, Waring R, Cummings M, Brinkworth R, Deffenbaugh AM, Burbidge LA, Pruss D, Judkins T, Scholl T, Bekessy A, Marsh A, Lovelock P, Wong M, Tesoriero A, Renard H, Southey M, Hopper JL, Yannoukakos K, Brown M, Easton D, Tavtigian SV, Goldgar D, Spurdle AB (2006) Genetic and histopathologic evaluation of BRCA1 and BRCA2 DNA sequence variants of unknown clinical significance. Cancer Res 66: 2019–2027
Cressman VL, Backlund DC, Avrutskaya AV, Leadon SA, Godfrey V, Koller BH (1999) Growth retardation, DNA repair defects, and lack of spermatogenesis in BRCA1-deficient mice. Mol Cell Biol 19: 7061–7075
Deng CX (2006) BRCA1: cell cycle checkpoint, genetic instability, DNA damage response and cancer evolution. Nucleic Acids Res 34: 1416–1426
ElShamy WM, Livingston DM (2004) Identification of BRCA1-IRIS, a BRCA1 locus product. Nat Cell Biol 6: 954–967
Evers B, Jonkers J (2006) Mouse models of BRCA1 and BRCA2 deficiency: past lessons, current understanding and future prospects. Oncogene 25: 5885–5897
Fan S, Wang J, Yuan R, Ma Y, Meng Q, Erdos MR, Pestell RG, Yuan F, Auborn KJ, Goldberg ID, Rosen EM (1999) BRCA1 inhibition of estrogen receptor signaling in transfected cells. Science 284: 1354–1356
Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I, Knights C, Martin NM, Jackson SP, Smith GC, Ashworth A (2005) Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434: 913–917
Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, Mortimer P, Swaisland H, Lau A, O’Connor M, Ashworth A, Carmichael J, Kaye SB, Schellens JHM, De Bono JS (2009) Inhibition of poly(ADP-Ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med 361: 123–134
Foulkes WD, Stefansson IM, Chappuis PO, Bégin LR, Goffin JR, Wong N, Trudel M, Akslen LA (2003) Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst 95: 1482–1485
Ganesan S, Silver DP, Greenberg RA, Avni D, Drapkin R, Miron A, Mok SC, Randrianarison V, Brodie S, Salstrom J, Rasmussen TP, Klimke A, Marrese C, Marahrens Y, Deng CX, Feunteun J, Livingston DM (2002) BRCA1 supports XIST RNA concentration on the inactive X chromosome. Cell 111: 393–405
Greenblatt MS, Chappuis PO, Bond JP, Hamel N, Foulkes WD (2001) TP53 mutations in breast cancer associated with BRCA1 or BRCA2 germ-line mutations: distinctive spectrum and structural distribution. Cancer Res 61: 4092–4097
Hakem R, De la Pompa JL, Elia A, Potter J, Mak TW (1997) Partial rescue of Brca15–6 early embryonic lethality by p53 or p21 null mutation. Nat Genet 16: 298–302
Hashizume R, Fukuda M, Maeda I, Nishikawa H, Oyake D, Yabuki Y, Ogata H, Ohta T (2001) The RING heterodimer BRCA1-BARD1 is a ubiquitin ligase inactivated by a breast cancer-derived mutation. J Biol Chem 276: 14537–14540
Hohenstein P, Kielman MF, Breukel C, Bennett LM, Wiseman R, Krimpenfort P, Cornelisse C, Van Ommen G, Devilee P, Fodde R (2001) A targeted mouse Brca1 mutation removing the last BRCT repeat results in apoptosis and embryonic lethality at the headfold stage. Oncogene 20: 2544–2550
Holstege H, Joosse SA, Van Oostrom CT, Nederlof PM, Jonkers J (2009) High incidence of protein-truncating TP53 mutations in BRCA1-related breast cancer. Cancer Res 69: 3625–3633
Huber LJ, Yang TW, Sarkisian CJ, Master SR, Deng CX, Chodosh LA (2001) Impaired DNA damage response in cells expressing an exon 11-deleted murine Brca1 variant that localizes to nuclear foci. Mol Cell Biol 21: 4005–4015
Johannsson OT, Idvall I, Anderson C, Borg A, Barkardóttir RB, Egilsson V, Olsson H (1997) Tumour biological features of BRCA1-induced breast and ovarian cancer. Eur J Cancer 33: 362–371
Jonkers J, Berns A (2002) Conditional mouse models of sporadic cancer. Nat Rev Cancer 2: 251–265
Katiyar P, Ma Y, Fan S, Pestell RG, Furth PA, Rosen EM (2006) Regulation of progesterone receptor by BRCA1 in mammary cancer. Nucl Recept Signal 4: e0006
Kennedy RD, Quinn JE, Mullan PB, Johnston PG, Harkin DP (2004) The role of BRCA1 in the cellular response to chemotherapy. J Natl Cancer Inst 96: 1659–1668
Kim SS, Cao L, Lim SC, Li C, Wang RH, Xu X, Bachelier R, Deng CX (2006) Hyperplasia and spontaneous tumor development in the gynecologic system in mice lacking the BRCA1-Δ11 isoform. Mol Cell Biol 26: 6983–6992
Kuschel B, Gayther SA, Easton DF, Ponder BA, Pharoah PD (2001) Apparent human BRCA1 gene knockout caused by mispriming during polymerase chain reaction: implications for genetic testing. Genes Chromosomes Cancer 31: 96–98
Liu S, Ginestier C, Charafe-Jauffret E, Foco H, Kleer CG, Merajver SD, Dontu G, Wicha MS (2008) BRCA1 regulates human mammary stem/progenitor cell fate. Proc Natl Acad Sci USA 105: 1680–1685
Liu X, Holstege H, Van der Gulden H, Treur-Mulder M, Zevenhoven J, Velds A, Kerkhoven RM, Van Vliet MH, Wessels LFA, Peterse JL, Berns A, Jonkers J (2007) Somatic loss of BRCA1 and p53 in mice induces mammary tumors with features of human BRCA1-mutated breast cancer. Proc Natl Acad Sci USA 104: 12111–12116
Ludwig T, Chapman DL, Papaioannou VE, Efstratiadis A (1997) Targeted mutations of breast cancer susceptibility gene homologs in mice: lethal phenotypes of Brca1, Brca2, Brca1/Brca2, Brca1/p53 and Brca2/p53 nullizygous embryos. Genes Dev 1: 1226–1241
Ludwig T, Fisher P, Ganesan S, Efstratiadis A (2001) Tumorigenesis in mice carrying a truncating Brca1 mutation. Genes Dev 15: 1188–1193
Mak TW, Hakem A, McPherson JP, Shehabeldin A, Zablocki E, Migon E, Duncan GS, Bouchard D, Wakeham A, Cheung A, Karaskova J, Sarosi I, Squire J, Marth J, Hakem R (2000) Brca1 required for T cell lineage development but not TCR loci rearrangement. Nat Immunol 1: 77–82
Manié E, Vincent-Salomon A, Lehmann-Che J, Pierron G, Turpin E, Warcoin M, Gruel N, Lebigot I, Sastre-Garau X, Lidereau R, Remenieras A, Feunteun J, Delattre O, De Thé H, Stoppa-Lyonnet D, Stern MH (2009) High frequency of TP53 mutation in BRCA1 and sporadic basal-like carcinomas but not in BRCA1 luminal breast tumors. Cancer Res 69: 663–671
McCarthy A, Savage K, Gabriel A, Naceur C, Reis-Filho JS, Ashworth A (2007) A mouse model of basal-like breast carcinoma with metaplastic elements. J Pathol 211: 389–398
Miki Y, Swensen J, Shattuck-Eidens D, Futreal PA, Harshman K, Tavtigian S, Liu Q, Cochran C, Bennett LM, Ding W (1994) A strong candidate for the breast and ovarian susceptibility gene BRCA1. Science 266: 66–71
Moynahan ME, Chiu JW, Koller BH, Jasin M (1999) Brca1 controls homology-directed DNA repair. Mol Cell 4: 511–518
Mullan PB, Quinn JE, Harkin DP (2006) The role of BRCA1 in transcriptional regulation and cell cycle control. Oncogene 25: 5854–5863
Narod SA, Foulkes WD (2004) BRCA1 and BRCA2: 1994 and beyond. Nat Rev Cancer 4: 665–676
Narod SA, Offit K (2005) Prevention and management of hereditary breast cancer. J Clin Oncol 10: 1656–1663
Pettigrew CA, French JD, Saunus JM, Edwards SL, Sauer AV, Smart CE, Lundström T, Wiesner C, Spurdle AB, Rothnagel JA, Brown MA (2008) Identification and functional analysis of novel BRCA1 transcripts, including mouse Brca1-Iris and human pseudo-BRCA1. Breast Cancer Res Treat (E-pub ahead of print 9 December 2008)
Poole AJ, Li Y, Kim Y, Lin SCJ, Lee WH, Lee EY (2006) Prevention of Brca1-mediated mammary tumorigenesis in mice by a progesterone antagonist. Science 314: 1467–1470
Reid LJ, Shakya R, Modi AP, Lokshin M, Cheng JT, Jasin M, Baer R, Ludwig T (2008) E3 ligase activity of BRCA1 is not essential for mammalian cell viability or homology-directed repair of double-strand DNA breaks. Proc Natl Acad Sci USA 105: 20876–20881
Rottenberg S, Jaspers JE, Kersbergen A, Van der Burg E, Nygren AOH, Zander SAL, Derksen PWB, De Bruin M, Zevenhoven J, Lau A, Boulter R, Cranston A, O’Connor MJ, Martin NMB, Borst P, Jonkers J (2008) High sensitivity of BRCA1-deficient mammary tumors to the PARP inhibitor AZD2281 alone and in combination with platinum drugs. Proc Natl Acad Sci USA 105: 17079–17084
Rottenberg S, Nygren AOH, Pajic M, Van Leeuwen FWB, Van der Heijden I, Van de Wetering K, Liu X, De Visser K, Gilhuijs KG, Van Tellingen O, Schouten JP, Jonkers J, Borst P (2007) Selective induction of chemotherapy resistance of mammary tumors in a conditional mouse model for hereditary breast cancer. Proc Natl Acad Sci USA 104: 12117–12122
Saal LH, Gruvberger-Saal SK, Persson C, Lövgren K, Jumppanen M, Staaf J, Jönsson G, Pires MM, Maurer M, Holm K, Koujak S, Subramaniyam S, Vallon-Christersson J, Olsson H, Su T, Memeo L, Ludwig T, Ethier SP, Krogh M, Szabolcs M, Murty VVVS, Isola J, Hibshoosh H, Parsons R, Borg A (2008) Recurrent gross mutations of the PTEN tumor suppressor gene in breast cancers with deficient DSB repair. Nat Genet 40: 102–107
Scully R, Chen J, Plug A, Xiao Y, Weaver D, Feunteun J, Ashley T, Livingston DM (1997) Association of BRCA1 with Rad51 in mitotic and meiotic cells. Cell 88: 265–275
Shafee N, Smith CR, Wei S, Kim Y, Mills GB, Hortobagyi GN, Stanbridge EJ, Lee EY (2008) Cancer stem cells contribute to cisplatin resistance in Brca1/p53-mediated mammary tumors. Cancer Res 68: 3243–3250
Shakya R, Szabolcs M, McCarthy E, Ospina E, Basso K, Nandula S, Murty V, Baer R, Ludwig T (2008) The basal-like mammary carcinomas induced by Brca1 or Bard1 inactivation implicate the BRCA1/BARD1 heterodimer in tumor suppression. Proc Natl Acad Sci USA 105: 7040–7045
Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S, Demeter J, Perou CM, Lønning PE, Brown PO, Børresen-Dale AL, Botstein D (2003) Repeated observation of breast cancer subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 100: 8418–8423
Swisher EM, Sakai W, Karlan BY, Wurz K, Urban N, Taniguchi T (2008) Secondary BRCA1 mutations in BRCA1-mutated ovarian carcinomas with platinum resistance. Cancer Res 68: 2581–2586
Tan DSP, Rothermundt C, Thomas K, Bancroft E, Eeles R, Shanley S, Ardern-Jones A, Norman A, Kaye SB, Gore ME (2008) ‘Brcaness’ syndrome in ovarian cancer: A case-control study describing the clinical features and outcome of patients with epithelial ovarian cancer associated with BRCA1 and BRCA2 mutations. J Clin Oncol 26: 5530–5536
Tirkkonen M, Johannsson O, Agnarsson BA, Olsson H, Ingvarsson S, Karhu R, Tanner M, Isola J, Barkardottir RB, Borg A, Kallioniemi OP (1997) Distinct somatic genetic changes associated with tumor progression in carriers of BRCA1 and BRCA2 germ-line mutations. Cancer Res 57: 1222–1227
Wu LC, Wang ZW, Tsan JT, Spillman MA, Phung A, Xu XL, Yang MCW, Hwang LY, Bowcock AM, Baer R (1996) Identification of a RING protein that can interact in vivo with the BRCA1 gene product. Nat Genet 14: 430–440
Xu X, Qiao W, Linke SP, Cao L, Li WM, Furth PA, Harris CC, Deng CX (2001) Genetic interactions between tumor suppressors Brca1 and p53 in apoptosis, cell cycle and tumorigenesis. Nat Genet 28: 266–271
Xu X, Wagner KU, Larson D, Weaver Z, Li C, Ried T, Hennighausen L, Wynshaw-Boris A, Deng CX (1999a) Conditional mutation of Brca1 in mammary epithelial cells results in blunted ductal morphogenesis and tumour formation. Nat Genet 22: 37–43
Xu X, Weaver Z, Linke SP, Li C, Gotay J, Wang XW, Harris CC, Ried T, Deng CX (1999b) Centrosome amplification and a defective G2-M cell cycle checkpoint induce genetic instability in BRCA1 exon 11 isoform-deficient cells. Mol Cell 3: 389–395
Acknowledgements
We thank Piet Borst, Peter Bouwman, Bastiaan Evers and Janneke Jaspers for critically reading the paper and providing helpful suggestions. We acknowledge the financial support from the Dutch Cancer Society (NKI2007-3772 and NKI2008-4116).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Drost, R., Jonkers, J. Preclinical mouse models for BRCA1-associated breast cancer. Br J Cancer 101, 1651–1657 (2009). https://doi.org/10.1038/sj.bjc.6605350
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605350
Keywords
This article is cited by
-
Loss of function of BRCA1 promotes EMT in mammary tumors through activation of TGFβR2 signaling pathway
Cell Death & Disease (2022)
-
Haploinsufficiency for BRCA1 leads to cell-type-specific genomic instability and premature senescence
Nature Communications (2015)
-
A critical role of CD29 and CD49f in mediating metastasis for cancer-initiating cells isolated from a Brca1-associated mouse model of breast cancer
Oncogene (2014)
-
Double heterozygosity for germline mutations in BRCA1 and p53 in a woman with early onset breast cancer
Breast Cancer Research and Treatment (2014)
-
Germline mutation of Brca1 alters the fate of mammary luminal cells and causes luminal-to-basal mammary tumor transformation
Oncogene (2013)