Abstract
Background:
To define the spectrum of human papillomavirus (HPV) types and establish an age limit for triage HPV testing in atypical squamous cells of undetermined significance (ASCUS) and low-grade squamous intraepithelial lesion (LSIL).
Materials and methods:
343 liquid-based cytological samples from the population-based screening programme with minor abnormalities were subjected to HPV genotyping (Linear Array, Roche, Basel, Switzerland).
Results:
High-risk human papillomavirus (HR-HPV) was found in 71% of LSIL and 49% of ASCUS cases (P<0.001). High-risk human papillomavirus prevalence was age-dependent in LSIL (P=0.01), with decreasing prevalence until the age of 50 years, followed by a slight increase. Human papillomavirus type 16 was the most common HR-HPV, found in 23% of HPV-positive women. Human papillomavirus type 18 was the sixth most common, found in 9.9% (P<0.001). An age-dependent quadratic trend was observed for multiple infections (P=0.01) with a trough at about 42 years. The most common HR-HPV types to show a coinfection with HPV16 (clade 9) were HPV39 (28%), 45 (38%), and 59 (46%), belonging to HPV18 clade 7. The frequency of low-risk (LR) vs probable HR and HR-HPV also followed an age-dependent quadratic trend.
Conclusions:
After the age of 25 years, HR-HPV prevalence is similar in LSIL and ASCUS cases, motivating a low age limit for triage HPV testing. Multiple infections and LR/HR-HPV dominance are age-dependent. Genotyping in longitudinal design is needed to elucidate the importance of multiple infections in cancer progression and in cross-protection from vaccination.
Similar content being viewed by others
Main
Persistent infection with high-risk human papillomavirus (HR-HPV) types has a critical aetiological function in the development of cervical intraepithelial neoplasia (CIN) and cervical cancer (Walboomers et al, 1999). Progression from low-grade to high-grade dysplasia and invasive disease is rare in the absence of HPV (Khan et al, 2005). Human papillomavirus types16 and 18 are incriminated as the causative agents in 65–77% of cervical cancers (Smith et al, 2007). The effect of multiple HPV infections on CIN and cancer development is still unclear, but several publications argue that certain multiple infections may confer a risk similar to the risk of a single HPV16 infection (Becker et al, 1994; Trottier et al, 2006; Wheeler et al, 2006). With the implementation of vaccination programmes, interest is also growing in cross-protection against HPV genotypes belonging to the same clade or phylogenetic species (Ault, 2007; Castellsague et al, 2008; Poolman et al, 2008; Sargent et al, 2008). Human papillomavirus type 16 belongs to clade 9, as do HPV31, 33, 35, 52, and 58, whereas HPV18 belongs to clade 7, along with HPV39, 45, 59, and 68 (de Villiers et al, 2004).
Awareness of the causal relationship between HPV infection and cervical cancer has made the detection of the virus an attractive approach to identify women at risk of developing cervical cancer (Cuzick et al, 2008). This approach, which is particularly important in cases of minor cytological abnormalities, is internationally accepted for use in cases of atypical squamous cells of undetermined significance (ASCUS). However, it has not been generally recommended in cases of low-grade squamous intraepithelial lesions (LSILs) because of the high prevalence of oncogenic HPV in this group (Sherman et al, 2002; Schiffman and Solomon, 2003; Arbyn et al, 2006; Wright et al, 2007). Women with minor cytological abnormalities account for a large proportion of those referred for further investigation, a process resulting in psychological stress and considerable health-care costs (Freeman-Wang et al, 2001; Idestrom et al, 2003).
In Sweden, about 3–5% of all smears show some kind of abnormality, almost 80% of which are minor cytological changes (Sparen, 2008). Current Swedish guidelines for management of minor abnormalities do not include HPV testing; rather, a second Pap smear or colposcopy is required (Ahlberg-Ranje et al, 2008). The question whether HPV testing may improve the Swedish screening programme is under discussion, especially in the light of the potential to identify precancerous lesions among ASCUS and LSIL and to distinguish these from reactive or degenerative lesions. According to our previous study, complementing liquid-based cytology (LBC) with an HPV test in cases of ASCUS and LSIL may lead to a 40% decrease in the number of these women referred for further investigation (Froberg et al, 2008). Human papillomavirus prevalence is high among younger women with LSIL, which is why an age limit for triage HPV testing is being sought. We wished to compare the age-specific prevalence of HR-HPV in these cytological categories to show that difference in prevalence is not an argument against triage testing.
The purpose of our study was to identify the HPV types present among women with minor cytological abnormalities using the PCR-based Linear Array HPV Genotyping Test (Roche Diagnostics, Basel, Switzerland) and to describe the prevalence of multiple infections in relation to age before the implementation of vaccination programmes.
Materials and methods
Patients
From September 2005 through to September 2006, 4204 LBC samples from a population-based screening programme were obtained from seven maternity health centres in Southern Stockholm as previously reported (Froberg et al, 2008). Later in 2006, an additional 2024 samples were collected. Minor cytological abnormalities were found in 343 (5.5%) of these 6228 LBC samples, comprising the cytological classifications of ASCUS and LSIL based on the Bethesda nomenclature system (Solomon et al, 2002). According to Swedish recommendations, koilocytosis without signs of dysplasia was reported as non-pathologic. Therefore, the LSIL group only contains samples corresponding to cytological cervical intraepithelial neoplasia grade 1 (CIN1). Approval from the ethics committee and written informed consent from all women were obtained before inclusion.
HPV DNA extraction and detection with linear array
A 2 ml PreservCyt suspension from the remaining LBC sample after cytological evaluation was centrifuged and the cell pellet was lysed according to instructions in the Total Nucleic Acid Isolation kit. DNA was extracted using the MagNA Pure LC robot and analysed with the Linear Array HPV Genotyping Test (LA), according to the manufacturer's instructions (all procedures by Roche). The method includes a PCR amplification of extracted HPV DNA using a pool of biotinylated primers that hybridise in the L1 region of the HPV genome, chemical denaturation of HPV DNA amplicons to single-stranded DNA, followed by hybridisation with matching type-specific DNA probes immobilised on nylon strips, and detection by colorimetric determination. The result is a pattern of blue lines on a nylon strip, which is visually read by comparing the pattern with a reference guide. The LA test covers 37 HPV types including 12 HR-HPV types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59), 6 probable high-risk (pHR-) HPV types (26, 53, 66, 68, 73, 82), and 19 low-risk or undetermined-risk (LR-) HPV types (6, 11, 40, 42, 54, 55, 61, 62, 64, 67, 69, 70, 71, 72, 81, 83, 84, IS39, CP6108) (Munoz et al, 2003).
Statistical analysis
Data were analysed with the software STATISTICA 6.1 (Statsoft Inc, Tulsa, OK, USA). Pearson's χ2 and Yates corrected χ2 (for n<5) tests were used to compare proportions, and Student's t-test was used to compare continuous variables between two groups. After plotting proportions of HR-HPV- and HPV-infected women and multiple infections, respectively, in each age group, a linear or polynomial fit was visually assessed to be the best model for logistic regression. We tested whether the proportion in each age group decreased linearly with age (log(p/1−p)=b0−b1x) and whether this was significantly different from null. Then we added a second degree (log(p/1−p)=b0−b1x+b2x2) to test whether the increase in women over a certain age was significantly different from null. We controlled for covariation between age and age2 using centred age and centred age2 in the model. The larger model with a second degree provided a better explanation as tested with Nagelkerke R2. Therefore, we concluded that the quadratic function, log(p/1−p)=b0−b1x+b2x2, could best describe the relationship between prevalence of HR-HPV in LSIL cases and age, multiple infections and age, and HR/LR-HPV dominance and age. Logistic regressions were also carried out using age group and cytological diagnosis as categorical predictors, as well as HPV prevalence as the dependent variable. The null hypothesis of no difference was rejected at a significance level of P<0.05.
Results
Cytology results and age distribution
There were 223 cases of LSIL and 120 cases of ASCUS, including three cases of atypical glandular cells of undetermined significance (AGUS). Age was illegible on one LSIL sample and on one ASCUS sample; therefore age was recorded in 341 of 343 women. The mean age was 33.6 years (median 32, range 22–60). Women were grouped according to age at 5-year intervals from age 20–49 years, whereas the oldest women, aged 50–60 years, were placed into a single comparably sized group. Table 1 shows age distribution. The mean age of women with ASCUS was 35.7 years and of those with LSIL was 32.4 years (P=0.002). In all, 73% of the women were younger than 40 years. Women with ASCUS were older than women with LSIL; 38% of women with ASCUS were 40 years or older, compared with 21% of women with LSIL (P<0.001, χ2).
HPV prevalence
The β-globin gene from all 343 samples was successfully amplified as shown by the presence of both low- and high-concentration bands on the array. A total of 282 (82%) women tested positive for one or more of the 37 included HPV types. Human papillomavirus prevalence ranged from 92% in the 20–29-year age group to 62% in women aged 40–45 years. Prevalence was 67% in women over 50 years. Age-specific prevalence for all HPV types and HR-HPV types (12 or 13 types) was higher in younger age groups and there was a linear decline with age (P<0.001, logistic regression, Table 1).
Human papillomavirus was more common in women with LSIL (207 out of 223, 93%) than in women with ASCUS (75 out of 120, 63%, P<0.001, χ2). Age-specific prevalence of all HPV types in women with ASCUS compared with women with LSIL is shown in Figure 1. Human papillomavirus prevalence was significantly dependent on age group (P=0.03), but did not reach a statistically significant difference between ASCUS and LSIL within each age group using logistic regression (P=0.098). However, there is an apparent tendency for increasing discrepancy with lower and especially higher age. χ2-tests to compare proportions gave significant differences in all age groups, except in the 30–39 year age group.
Age-specific prevalence of human papillomavirus (HPV) (all types) and HR-HPV infection in women with ASCUS and LSIL. Human papillomavirus all types P(age group × cytological diagnosis)=0.10; LSIL P(age)=0.20, P(age group)=0.03, P(age2)=0.003; ASCUS P(age)=0.001, P(age group)=0.04, P(age2)=0.34; HR-HPV P(age group × cytological diagnosis)=0.15; LSIL P(age)=0.001, P(age group)=0.01, P(age2)=0.19; ASCUS P(age)=0.04, P(age group)=0.11, P(age2)=0.16; all P-values calculated by logistic regression.
High-risk or pHR-HPV (18 types) was found in 68 (57%) ASCUS cases, compared with 181 (81%) LSIL cases (P<0.001, χ2). High-risk human papillomavirus (12 types) was found in 59 (49%) cases among women with ASCUS, compared with 158 (71%) in women with LSIL (P<0.001, χ2). Considering 13 types (HR-HPV and pHR-HPV 68), these were found in 60 (50%) ASCUS cases and in 159 (71%) LSIL cases (P<0.001, χ2). Figure 1 shows that HR-HPV prevalence was age dependent among women with LSIL (P=0.001, logistic regression), with a decreasing prevalence until the age of 50 years. A small increase was found in older women, but this was not statistically significant (P=0.19 for age2). A linear correlation between HR-HPV prevalence and age (but not age group) was also found in ASCUS cases (Figure 1). Age-specific HR-HPV prevalence did not reach a statistically significant difference between ASCUS and LSIL using logistic regression (P=0.15). χ2-tests revealed a significant difference in HR-HPV prevalence between ASCUS and LSIL in the youngest age group (Table 1).
HPV genotype distribution
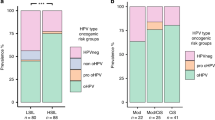
Figure 2 shows the prevalence of HR-HPV genotypes (including pHR-HPV68) in each age group in all women. Human papillomavirus type 16 was the most common HR-HPV and was found in 65 (23%) of the HPV-positive women, ranging from 30% (20 out of 67) in women aged 25–29 years to 14% (3 out of 22) in women aged 45–49 years (P=0.22, χ2). Remarkably, HPV18 was only found in 28 (9.9%) of all HPV-positive women (P<0.001 compared with HPV16, χ2). Human papillomavirus types 51, 52, 56, and 31 were also more common than HPV18. Human papillomavirus type 51 was equally or more common than HPV16 among women over 45 years of age. Among women with ASCUS, the most prevalent HR-HPV genotype was HPV16 (16%), followed by HPV51 and 52 (10%). Among women with LSIL, HPV16 was detected in 21%, followed by HPV56 in 11% of women (Figure 3). Table 2 outlines women infected with HPV16, 18, clade 9 HPV types, and clade 7 HPV types to elucidate the preventive potential of current HPV vaccines against low-grade cytological abnormalities. As shown in Figure 4, we found a shift in predominant genotypes with age. The proportion of LR genotypes increased with age, following a quadratic function (P<0.001, logistic regression).
Multiple infections
Multiple infections were common in our material (Figure 5). On average, we found 2.5 genotypes per HPV-positive sample. In one LSIL sample, nine different genotypes were found. In all, 54% (185 out of 343) of all women carried more than one HPV type. Women with LSIL had multiple types (61%, 136 out of 223) more frequently than did women with ASCUS (41%, 49 out of 120, P<0.001, χ2). Taking only HPV-positive samples into account, multiple infections were equally common in women with ASCUS and LSIL (65% or 49 out of 75, and 66% or 136 out of 207, respectively). The age-specific prevalence of multiple infections followed a quadratic function in LSIL cases (P=0.001, logistic regression, Figure 5). This was also found in multiple HR-HPV infections among the HR-HPV-positive LSIL cases (P=0.04, logistic regression). Among HR-HPV-positive samples, 39% (85 out of 217) were infected by more than one HR-HPV type and similar results were found for LSIL and ASCUS samples (39.9 and 37.3%, respectively, P=0.73, χ2).
Age-specific prevalence of multiple infections. Multiple HPV P(age group)=0.08, P(cytological diagnosis)=0.63, P(age group × cytological diagnosis)=0.73, LSIL P(age2)=0.001, turning point 41.6 years, ASCUS P(age2)=0.76. Multiple HR-HPV P(age group)=0.04, P(cytological diagnosis)=0.71, P(age group × cytological diagnosis)=0.24, LSIL P(age2)=0.04, turning point 38.6 years, ASCUS P(age group)=0.27, P(age2)=0.34. All P-values calculated by logistic regression.
In all, there were 710 individual HPV infections. Coinfection was equally common among LR-HPV genotypes (243 out of 268, 92%) and pHR-HPV genotypes (87 out of 101, 91%, P=0.21, χ2). Individuals infected with HR-HPV genotypes were somewhat less likely to be coinfected with a second HPV type (283 out of 341, 83%, P=0.006, χ2). The high-risk types that were most commonly seen in coinfection with HPV16 (clade 9) were HPV39 (28%), 45 (38%), and 59 (46%), belonging to HPV18 clade 7. Interestingly, HPV18 did not occur in either HPV39 or HPV45 (P⩽0.01, χ2), but was found in 13% of HPV59 infections (all clade 7). The high-risk types most commonly seen in coinfection with HPV18 were HPV56 (17%), 33 (14%), and 51 (14%), which did not differ from frequencies of HPV16 coinfection (P>0.7, χ2, for all). Figure 6 displays coinfection between HPV16 or HPV18 and the largest clades. HPV16-infected women were more often coinfected with clade 7 types (38%) than with similar clade 9 types (23%), although this did not reach statistical significance (P=0.06, χ2). Human papillomavirus type 18-infected women carried genotypes from clade 9 in 43% of cases, compared with similar clade 7 genotypes in 11% (P=0.02, χ2).
Discussion
We have presented an overview of HPV genotypes encountered in unselected ASCUS and LSIL cases of all ages detected in a population-based cytology screening programme and then established the prevalence of multiple infections in these cases.
We found that HPV prevalence varied with age and there was a slight but non-significant increase in HPV prevalence in women over 45 years. Others have found similar age-related patterns and attributed this slight increase to menopausal hormonal and immunological changes that may facilitate HPV DNA detection or reactivate latent infections from exposures earlier in life (reviewed by Bosch et al (2008)). Such findings may also be related to sexual behaviour and thus to increased exposure, as many women in this age group have divorced and remarried (Stevenson and Wolfers, 2007). Our finding of an increasing proportion of low-risk types in post-menopausal women was also observed by Castle et al (2006). This observation, including the increase in multiple infections among women over 50 years, might also reflect changes in hormonal or immunological status occurring at menopause. Some evidence suggests a hormonal effect on oncogene expression, at least for HPV16 and 18, by action on progesterone/glucocorticoid-responsive elements in the long control region of the HPV genome (Cole and Danos, 1987; Gloss et al, 1989). However, more recent research has called such a mechanism into question (Ruutu et al, 2006), and would instead suggest hormonal effects impairing apoptosis of infected cells. Oral contraceptives and high parity are known risk factors for cervical cancer (Munoz et al, 2002). One common characteristic of these factors and menopause is a state of anovulation. To our knowledge, no studies have explored whether other ovulatory hormones such as gonadotropins, inhibin, or prostaglandins could influence HPV-induced carcinogenesis.
The average prevalence of HR-HPV was higher in LSIL (71%) than in ASCUS cases (49%), which is consistent with a previous meta-analysis (Arbyn et al, 2005). However, the LSIL cases had a significantly lower rate of HR-HPV than the rate reported by the ASCUS-LSIL-Triage-Study (ALTS) Group (82.9%) (ALTS, 2000). The ALTS group concluded that triage HPV testing of LSIL had limited potential for clinical decision making. The difference in HR-HPV prevalence might be due to different criteria for defining ASCUS and LSIL, and also to a difference in the mean age of the populations (24.9 years in ALTS and 33.6 years in this study). We used the LA assay covering 37 HPV types and defined 12 HPV types as high risk. ALTS used Hybrid Capture II to define the same 12 HR-HPV types and HPV68 as high risk. This approach should not introduce any major difference, as HPV68 without coinfection with another HR-HPV was found only in one case of ASCUS and in one case of LSIL in our material. Age-dependent HPV prevalence in women without cytological abnormalities is a known phenomenon (Castle et al, 2006; de Sanjose et al, 2007; Bosch et al, 2008). Age-dependent prevalence in LSIL has been observed and discussed by Ronco et al (2007), although they only compared women who were older or younger than 35 years. High-risk human papillomavirus prevalence was age-dependent in our LSIL cases, but more stable in ASCUS cases. When using 5-year intervals for age grouping, the only significant difference in HR-HPV prevalence between ASCUS and LSIL was found within the youngest (20–24 years) age group. In LSIL, the largest drop in HR-HPV prevalence was after the age of 30 years (83% in women <30 vs 60% in women ⩾30, P<0.001). These findings suggest that age 30, or even younger, is a suitable cutoff point for HR-HPV triage in LSIL, when consideration is given only to the prevalence argument. This is supported by a histological follow-up study of 112 of these cases by our group, in which 48% of women over 30 years with LSIL and 60% of women with ASCUS were HR-HPV negative and none of these had a histology result of CIN2+ (Froberg et al, 2008) and could therefore have avoided additional investigation. This implies that the number of follow-ups after low-grade or ambiguous cytology results could be cut in half, at least in women over 30 years of age. In Figure 7, we present a suggested flowchart for triage HPV testing.
Viral persistence is believed to be the most important risk factor for cervical cancer. Yet, this is true only for certain oncogenic types (Schiffman et al, 2005). Assessment of viral persistence requires HPV genotyping. Genotyping will also be necessary to monitor the effects of vaccination and to explore the importance of multiple infections. One of the most noteworthy findings in our study was the high frequency of multiple infections. Similar results were previously reported by Cuschieri et al (2004) in a general screening population from Edinburgh using a linear array assay capable of identifying 27 types and similar liquid-based sampling. We found that the prevalence of multiple infections was consistent with a quadratic function, with increasing prevalence among women over the age of 50 years. One may speculate whether this finding is caused by re-infection, triggering of a latent infection, or if detection is favoured by menopausal changes in the epithelium as mentioned above. Epidemiological cancer data from Statistics Sweden (SCB) reveal a second peak in cervical cancer incidence in the 65–69-year age group, which also suggests increased susceptibility in postmenopausal women. Multiple infection increases the probability of finding at least one carcinogenic type. It is still unclear whether coinfections with certain types can exert a synergistic effect on malignant transformation. Microdissection studies have suggested a polyclonal origin for squamous cervical cancer (Guo et al, 2001). The importance of multiple infections needs to be elucidated in longitudinal studies with histological confirmation of progressive CIN.
The observed elevated specific coinfection rates of HPV16 with certain other HPV types, such as HPV39, 45, and 59, may be because of differences in susceptibility to certain genotypes (all clade 7), as postulated by Liaw et al (2001). We found that HPV18-infected women were more likely to be coinfected with non-related clade 9 types than with similar clade 7 types, arguing against specific susceptibility. Rather, our data support cross-protection from infection with HPV from the same clade. Up to 60% of women with minor cytological abnormalities would potentially benefit from catch-up vaccination, provided full cross-protection can be assumed, as discussed by Castellsague et al (2008).
As far as we know, our study is the only one to describe the prevalence of HPV genotypes in ASCUS and LSIL cases among women of all ages in Sweden. The relative frequencies of individual HR-HPV types were similar to those found during primary screening in a Swedish multicentre study comprising 5696 women aged 32–38 years (Swedescreen) (Naucler et al, 2007). The Swedescreen group found that HPV16, 31, and 33 represented the highest population-attributable risk proportion in the development of CIN2+. Human papillomavirus type 18 was only the sixth most commonly identified HR-HPV type resulting in CIN2+. Worldwide, HPV33 is associated with the third highest odds ratio (OR 373.5) for squamous-cell cervical cancer, behind HPV16 (OR 434.5) and HPV59 (OR 419.5) (Munoz et al, 2003). Considering that odds ratios vary for different HPV types, genotyping is needed to estimate risk in the individual case as well as to plan clinical follow-up and vaccination strategy. We think our data support the statement of Cuschieri et al (2004) that ‘a broad spectrum test should be implemented until the true impact of the persistence of less common HR-HPV types in neoplastic progression is established’.
Minor cytological abnormalities associated with certain HPV genotypes may progress to cervical cancer. High-risk human papillomavirus prevalence is similar among women with ASCUS and LSIL after the age of 30 years, supporting an age limit of 30 years or even younger for triage testing in LSIL cases and no age limit in ASCUS cases, in order to improve the effectiveness of the screening programme. Human papillomavirus genotyping in longitudinal studies is needed to elucidate the importance of multiple infections for cancer progression, as well as cross-protection from vaccination.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ahlberg-Ranje L, Andersson S, Bergmark K, Blomqvist L, Eriksson E, Larsson B, Lindblad E, Olsson S, Rosenborg L, Törnberg S, Zellbi A, Åvall-Lundqvist E (2008) Vårdprogram för cervix-, vaginal- och vulvacancer 2008. pp 1–85. Onkologiskt Centrum, Karolinska Universitetssjukhuset: Stockholm
ALTS (2000) Human papillomavirus testing for triage of women with cytologic evidence of low-grade squamous intraepithelial lesions: baseline data from a randomized trial. J Natl Cancer Inst 92: 397–402
Arbyn M, Paraskevaidis E, Martin-Hirsch P, Prendiville W, Dillner J (2005) Clinical utility of HPV-DNA detection: triage of minor cervical lesions, follow-up of women treated for high-grade CIN: an update of pooled evidence. Gynecol Oncol 99: S7–S11
Arbyn M, Sasieni P, Meijer CJ, Clavel C, Koliopoulos G, Dillner J (2006) Chapter 9: Clinical applications of HPV testing: a summary of meta-analyses. Vaccine 24 (Suppl 3): S78–S89
Ault KA (2007) Human papillomavirus vaccines and the potential for cross-protection between related HPV types. Gynecol Oncol 107: S31–S33
Becker TM, Wheeler CM, McGough NS, Parmenter CA, Jordan SW, Stidley CA, McPherson RS, Dorin MH (1994) Sexually transmitted diseases and other risk factors for cervical dysplasia among southwestern Hispanic and non-Hispanic white women. JAMA 271: 1181–1188
Bosch FX, Burchell AN, Schiffman M, Giuliano AR, de Sanjose S, Bruni L, Tortolero-Luna G, Kjaer SK, Munoz N (2008) Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine 26 (Suppl 10): K1–K16
Castellsague X, Klaustermeier J, Carrilho C, Albero G, Sacarlal J, Quint W, Kleter B, Lloveras B, Ismail MR, de Sanjose S, Bosch FX, Alonso P, Menendez C (2008) Vaccine-related HPV genotypes in women with and without cervical cancer in Mozambique: burden and potential for prevention. Int J Cancer 122: 1901–1904
Castle PE, Jeronimo J, Schiffman M, Herrero R, Rodriguez AC, Bratti MC, Hildesheim A, Wacholder S, Long LR, Neve L, Pfeiffer R, Burk RD (2006) Age-related changes of the cervix influence human papillomavirus type distribution. Cancer Res 66: 1218–1224
Cole ST, Danos O (1987) Nucleotide sequence and comparative analysis of the human papillomavirus type 18 genome. Phylogeny of papillomaviruses and repeated structure of the E6 and E7 gene products. J Mol Biol 193: 599–608
Cuschieri KS, Cubie HA, Whitley MW, Seagar AL, Arends MJ, Moore C, Gilkisson G, McGoogan E (2004) Multiple high risk HPV infections are common in cervical neoplasia and young women in a cervical screening population. J Clin Pathol 57: 68–72
Cuzick J, Arbyn M, Sankaranarayanan R, Tsu V, Ronco G, Mayrand MH, Dillner J, Meijer CJ (2008) Overview of human papillomavirus-based and other novel options for cervical cancer screening in developed and developing countries. Vaccine 26 (Suppl 10): K29–K41
de Sanjose S, Diaz M, Castellsague X, Clifford G, Bruni L, Munoz N, Bosch FX (2007) Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis 7: 453–459
de Villiers EM, Fauquet C, Broker TR, Bernard HU, zur Hausen H (2004) Classification of papillomaviruses. Virology 324: 17–27
Freeman-Wang T, Walker P, Linehan J, Coffey C, Glasser B, Sherr L (2001) Anxiety levels in women attending colposcopy clinics for treatment for cervical intraepithelial neoplasia: a randomised trial of written and video information. BJOG 108: 482–484
Froberg M, Johansson B, Hjerpe A, Andersson S (2008) Human papillomavirus ‘reflex’ testing as a screening method in cases of minor cytological abnormalities. Br J Cancer 99: 563–568
Gloss B, Chong T, Bernard HU (1989) Numerous nuclear proteins bind the long control region of human papillomavirus type 16: a subset of 6 of 23 DNase I-protected segments coincides with the location of the cell-type-specific enhancer. J Virol 63: 1142–1152
Guo Z, Wu F, Asplund A, Hu X, Mazurenko N, Kisseljov F, Ponten J, Wilander E (2001) Analysis of intratumoral heterogeneity of chromosome 3p deletions and genetic evidence of polyclonal origin of cervical squamous carcinoma. Mod Pathol 14: 54–61
Idestrom M, Milsom I, Andersson-Ellstrom A (2003) Women's experience of coping with a positive Pap smear: a register-based study of women with two consecutive Pap smears reported as CIN 1. Acta Obstet Gynecol Scand 82: 756–761
Khan MJ, Castle PE, Lorincz AT, Wacholder S, Sherman M, Scott DR, Rush BB, Glass AG, Schiffman M (2005) The elevated 10-year risk of cervical precancer and cancer in women with human papillomavirus (HPV) type 16 or 18 and the possible utility of type-specific HPV testing in clinical practice. J Natl Cancer Inst 97: 1072–1079
Liaw KL, Hildesheim A, Burk RD, Gravitt P, Wacholder S, Manos MM, Scott DR, Sherman ME, Kurman RJ, Glass AG, Anderson SM, Schiffman M (2001) A prospective study of human papillomavirus (HPV) type 16 DNA detection by polymerase chain reaction and its association with acquisition and persistence of other HPV types. J Infect Dis 183: 8–15
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, Snijders PJF, Meijer CJLM (2003) Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 348: 518–527
Munoz N, Franceschi S, Bosetti C, Moreno V, Herrero R, Smith JS, Shah KV, Meijer CJ, Bosch FX (2002) Role of parity and human papillomavirus in cervical cancer: the IARC multicentric case-control study. Lancet 359: 1093–1101
Naucler P, Ryd W, Tornberg S, Strand A, Wadell G, Hansson BG, Rylander E, Dillner J (2007) HPV type-specific risks of high-grade CIN during 4 years of follow-up: a population-based prospective study. Br J Cancer 97: 129–132
Poolman EM, Elbasha EH, Galvani AP (2008) Vaccination and the evolutionary ecology of human papillomavirus. Vaccine 26 (Suppl 3): C25–C30
Ronco G, Cuzick J, Segnan N, Brezzi S, Carozzi F, Folicaldi S, Dalla Palma P, Del Mistro A, Gillio-Tos A, Giubilato P, Naldoni C, Polla E, Iossa A, Zorzi M, Confortini M, Giorgi-Rossi P (2007) HPV triage for low grade (L-SIL) cytology is appropriate for women over 35 in mass cervical cancer screening using liquid based cytology. Eur J Cancer 43: 476–480
Ruutu M, Wahlroos N, Syrjanen K, Johansson B, Syrjanen S (2006) Effects of 17beta-estradiol and progesterone on transcription of human papillomavirus 16 E6/E7 oncogenes in CaSki and SiHa cell lines. Int J Gynecol Cancer 16: 1261–1268
Sargent A, Bailey A, Almonte M, Turner A, Thomson C, Peto J, Desai M, Mather J, Moss S, Roberts C, Kitchener HC (2008) Prevalence of type-specific HPV infection by age and grade of cervical cytology: data from the ARTISTIC trial. Br J Cancer 98: 1704–1709
Schiffman M, Herrero R, Desalle R, Hildesheim A, Wacholder S, Rodriguez AC, Bratti MC, Sherman ME, Morales J, Guillen D, Alfaro M, Hutchinson M, Wright TC, Solomon D, Chen Z, Schussler J, Castle PE, Burk RD (2005) The carcinogenicity of human papillomavirus types reflects viral evolution. Virology 337: 76–84
Schiffman M, Solomon D (2003) Findings to date from the ASCUS-LSIL Triage Study (ALTS). Arch Pathol Lab Med 127: 946–949
Sherman ME, Schiffman M, Cox JT (2002) Effects of age and human papilloma viral load on colposcopy triage: data from the randomized Atypical Squamous Cells of Undetermined Significance/Low-Grade Squamous Intraepithelial Lesion Triage Study (ALTS). J Natl Cancer Inst 94: 102–107
Smith JS, Lindsay L, Hoots B, Keys J, Franceschi S, Winer R, Clifford GM, Bosetti C, Munoz N, Herrero R, Bosch FX, Eluf-Neto J, Meijer CJ, Van Den Brule AJ, Peeling RW (2007) Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer 121: 621–632
Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, Raab S, Sherman M, Wilbur D, Wright Jr T, Young N (2002) The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA 287: 2114–2119
Sparen P (2008) Gynekologisk cellprovskontroll i Sverige: Rapport 2007 med data till 2006. pp 1–27. Nationella kvalitetsregistret för gynekologisk cellprovskontroll: Stockholm, Sweden
Stevenson B, Wolfers J (2007) Marriage and divorce: changes and their driving forces. J Econ Perspect 21: 27–52
Trottier H, Mahmud S, Costa MC, Sobrinho JP, Duarte-Franco E, Rohan TE, Ferenczy A, Villa LL, Franco EL (2006) Human papillomavirus infections with multiple types and risk of cervical neoplasia. Cancer Epidemiol Biomarkers Prev 15: 1274–1280
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Muñoz N (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189: 12–19
Wheeler CM, Hunt WC, Schiffman M, Castle PE (2006) Human papillomavirus genotypes and the cumulative 2-year risk of cervical precancer. J Infect Dis 194: 1291–1299
Wright Jr TC, Massad LS, Dunton CJ, Spitzer M, Wilkinson EJ, Solomon D (2007) 2006 consensus guidelines for the management of women with abnormal cervical cancer screening tests. Am J Obstet Gynecol 197: 346–355
Acknowledgements
We thank Marc Arbyn for valuable comments on the manuscript and Carmen Flores-Staino and Hamzah Safari for professional laboratory work. Financial support was provided by grants from the Swedish Cancer Society, the Swedish Research Council, and the Medical Research Council, as well as from the Cancer Society in Stockholm, the Stockholm County Council, and AFA Insurance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Brismar-Wendel, S., Froberg, M., Hjerpe, A. et al. Age-specific prevalence of HPV genotypes in cervical cytology samples with equivocal or low-grade lesions. Br J Cancer 101, 511–517 (2009). https://doi.org/10.1038/sj.bjc.6605165
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605165
Keywords
This article is cited by
-
HPV genotype prevalence and distribution during 2009–2018 in Xinjiang, China: baseline surveys prior to mass HPV vaccination
BMC Women's Health (2019)
-
HPV genotype distribution in Brazilian women with and without cervical lesions: correlation to cytological data
Virology Journal (2016)
-
Cost Effectiveness of Human Papillomavirus-16/18 Genotyping in Cervical Cancer Screening
Applied Health Economics and Health Policy (2015)
-
Prevalence of human papillomavirus infection and phylogenetic analysis of HPV-16 E6 variants among infected women from Northern Brazil
Infectious Agents and Cancer (2014)
-
Prevalence of high-risk HPV types and associated genital diseases in women born in 1988/89 or 1983/84 – results of WOLVES, a population-based epidemiological study in Wolfsburg, Germany
BMC Infectious Diseases (2013)