Abstract
Lung cancer screening programmes using chest X-ray and sputum cytology are routinely performed in Japan; however, the efficacy is insufficient. Screening using low-dose computed tomography (CT) is a more effective approach and has the potential to detect the disease more accurately. A total of 7183 low-dose CT screening tests for 4689 participants and 36 085 chest X-ray screening tests for 13 381 participants were conducted between August 1998 and May 2002. Sensitivity and specificity of lung cancer screening were calculated by both the detection method and the incidence method by linkage of the screening database and the Cancer Registry database. The preclinical detectable phase was assumed to be 1 year. Sensitivity and specificity by the detection method were 88.9 and 92.6% for low-dose CT and 78.3 and 97.0% for chest X-ray, respectively. Sensitivity of low-dose CT by the incidence method was 79.5%, whereas that of chest X-ray was 86.5%. Lung cancer screening using low-dose CT resulted in higher sensitivity and lower specificity than traditional screening according to the detection method. However, sensitivity by the incidence method was not as high as this. These findings demonstrate the potential for overdiagnosis in CT screening-detected cases.
Similar content being viewed by others
Main
Lung cancer is the leading cause of cancer death in Japan, with 45 927 men and 17 307 women dying from lung cancer in 2006. Since 1987, lung cancer screening programme using chest X-ray and sputum cytology for all residents aged 40 years of age and older regardless of smoking status has been conducted by the Ministry of Health and Welfare. Unfortunately, the efficacy of lung cancer screening using chest X-ray and sputum cytology is insufficient (Fontana et al, 1986; Marcus et al, 2000a, 2006b; Sagawa et al, 2003a). Therefore, a more effective approach is required to decrease lung cancer deaths.
Annual lung cancer screening using low-dose computed tomography (CT) has been performed as an opportunistic screening method since the early 1990s in Japan. Several study groups introduced low-dose CT for population-based screening in clinical trials. These previous studies reported a high detection rate, an ability to detect small tumours and a high survival rate in detected cases (Henschke et al, 2001, 2006; Sone et al, 2001; Nawa et al, 2002; Sobue et al, 2002a; Swensen et al, 2002; Diederich et al, 2004; Jett, 2005; Libby et al, 2006). Some studies referred to interval cancer cases of lung cancer screening using low-dose CT, and one study referred to the sensitivity of screening (Sone et al, 2001; Diederich et al, 2004). However, screening databases are yet to be linked to a cancer registry, which is essential for accurate evaluation of screening, including the confirmation of all interval cancer cases. To date, no study has been conducted on sensitivity and specificity of annual lung cancer screening using low-dose CT and cancer registry data. Therefore, the present study was conducted to evaluate sensitivity and specificity of annual lung cancer screening using low-dose CT and data from screening and local cancer registry databases.
Materials and methods
Study setting
Since 1998, annual population-based lung cancer screening using low-dose CT has been conducted at five municipalities in Osaka prefecture: A (city), B (city), C (town), D (town) and E (town). All residents aged 40 years of age and older were recruited by mail using a letter from the public health division of each municipality regardless of smoking status. Subjects recruited to the lung cancer screening programme underwent either miniature chest X-ray or low-dose chest CT.
As a principle, heavy smokers were recommended to undergo low-dose CT screening. In addition, the persons who want to undergo low-dose CT screening also underwent low-dose CT screening. Others underwent chest X-ray screening.
A high-risk group for lung cancer, smokers with over a 20 pack index or who had haemosputum, was examined by 3-day pooled sputum cytology.
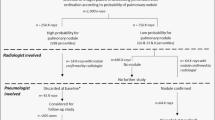
Low-dose CT or chest X-ray images were reviewed and classified by two trained physicians to determine the need for further clinical examination. Sputum cytology was also performed by a certified cytopathologist to determine the need for further clinical examination.
Those diagnosed with the need for further clinical examination were regarded as screen-positive. These individuals were asked to undergo further diagnostic evaluation at Osaka Medical Center for Cancer and Cardiovascular Disease. All individuals with positive chest X-ray screening were asked to undergo chest CT as a further examination.
Data collection
All subjects were individuals who had undergone either low-dose CT or chest X-ray screening tests between August 1998 and May 2002. The following participants were excluded from the analyses: (1) participants who had a past history of lung cancer, (2) participants who were suspected of having lung cancer by a previous screening or other medical examination and had received medical treatment and (3) participants who were suspected of having lung cancer at the previous screening or by other medical examination, but had refused further examinations.
Participants were divided into two groups: (a) low-dose CT group and (b) chest X-ray group. The low-dose CT group consisted of persons who had undergone low-dose CT at least one time during the study period, whereas the chest X-ray group consisted of persons who had undergone only chest X-ray. The low-dose CT group included those who had undergone both CT screening and chest X-ray screening within the study period. For these cases, screenings using chest X-ray were ignored to evaluate low-dose CT screening.
All data were entered into the screening database that was linked to the Osaka Cancer Registry (OCR) database with data reflecting incidence cases through December 2003. The indices used to collate the two databases were name, sex, address and date of birth. Information about lung cancer cases was extracted from hospital medical records or the OCR file.
We assumed that the preclinical detectable phase was 1 year for interval cancer cases. For death certificate-only cases, the date of 3 months before death was regarded as the date of diagnosis. Using these parameters, all lung cancer cases diagnosed within 1 year after a negative screen were regarded as interval lung cancers. Screen-detected cases were considered as true-positive cases regardless of the time between the date of screening and the date of diagnosis.
Statistical analyses
The sensitivity of screening was calculated by both the detection method and the incidence method. Although the detection method is simple and widely used, sensitivity estimated by detection method is affected by length and overdiagnosis biases (Day, 1985). The incidence method is not affected by length or overdiagnosis bias and is often used for breast cancer screening or colorectal cancer screening (Fletcher et al, 1993; Zappa et al, 2001).
Detection method
Sensitivity and specificity were calculated by the detection method using the following formulae.

Sensitivity and specificity calculated by the detection method were stratified by smoking status, histological type and screening rank. The screening rank was classified as the initial and repeated screenings, regardless of the number of years since the initial screening.
Incidence method
In addition, we calculated sensitivity by the incidence method using the following approximate formula (Day, 1985; Zappa et al, 2001):

Where I(t)=the observed number of interval cancer cases during time t and I=the expected number of cases in the absence of screening.
We calculated the number of expected lung cancer cases in the absence of screening based on the following data. Age-specific lung cancer incidence rates provided from the OCR in 2001 were 16.3, 61.6, 180.9, 477.3 and 770.2 (per 100 000 person-years) for men, and 6.3, 25.9, 53.4, 116.7 and 241.3 for women, for age groups 40–49, 50–59, 60–69, 70–79 and ⩾80, respectively. Lung cancer incidence rates in the OCR were weighted by smoking status. According to the previous large-scale cohort study in Japan, the lung cancer incidence rates among ex-smokers and current smokers were assumed to be 2.2 times and 4.5 times of that of nonsmokers, respectively, among men, and 3.7 times and 4.2 times, respectively, among women (Sobue et al, 2002b). According to an official report from Osaka prefecture in 2003, the proportions of current smokers, ex-smokers and nonsmokers were 40, 30 and 30% among men, and 11, 7 and 82% among women, respectively (Department of public health, Osaka Prefecuture, 2006).
We assumed that smoking status proportions were the same across all age groups, so the expected incidence rate according to sex and smoking status was modified using the following formulae:

The expected incidence rates for ex-smokers and current smokers were assumed to be 2.2 times and 4.5 times of that of nonsmokers, respectively, among men, and 3.7 times and 4.2 times, respectively, among women.
The differences in sensitivity and specificity among the stratified variables were tested by χ2 test. All statistical analyses were performed using SAS software, version 8.01 (SAS Institute Inc., Cary, NC, USA).
Ethical approval
The protocol for the present study was approved by the Ethics Committee of Osaka Medical Center for Cancer and Cardiovascular Disease, Osaka, Japan. Informed consent for participation in the clinical trial, including CT screening, was obtained from all individuals.
Results
From August 1998 to May 2002, a total of 7190 low-dose CT screening tests and a total of 36 085 chest X-ray screening tests were performed. Seven screening participants were excluded from analysis because they did not meet the eligibility criteria. Participants were ineligible for the following reasons: two participants were under follow-up care, one was suspected of having lung cancer but refused further examination and four had a history of lung cancer. A total of 7183 low-dose CT screening tests for 4689 participants (2765 men and 1924 women) and 36 085 chest X-ray screening tests for 13 381 participants (4180 men and 9201 women) enrolled in the study.
Table 1 shows the number of screening tests by sex, age group, smoking status and rank of screening tests. Most of the participants who underwent low-dose CT screening were male current smokers or ex-smokers. Sputum cytology was additionally performed for 3539 screening tests for the low-dose CT group and 5417 screening tests for the chest X-ray group.
Forty cases in the low-dose CT group and 29 cases in the chest X-ray group were detected by the screening. Five interval cases in the low-dose CT group and eight interval cases in the chest X-ray group were confirmed by linkage to OCR (Table 2). All of the interval cancer cases for both the low-dose CT group and the chest X-ray group were smokers. As for the low-dose CT group, all of them were nonadenocarcinoma. Two cases, one in the low-dose CT group and one in the chest X-ray group, were detected by sputum cytology on negative radiological screen.
Table 3 shows sensitivity and specificity by the detection method according to histological type, smoking status and rank of screening. As a result, sensitivity and specificity (95% confidence interval) of screening were 88.9% (79.7–98.1%) and 92.6% (92.0–93.2%) for the low-dose CT group, and 78.3% (65.1–91.6%) and 97.0% (96.9–97.2%) for the chest X-ray group, respectively. Specificity of chest X-ray screening was significantly higher than that of low-dose CT screening (P<0.001). The difference in sensitivity by the detection method was not significant.
As for histological type, sensitivity for adenocarcinoma was significantly higher than that for nonadenocarcinoma (low-dose CT: 100 vs 61.5%; P<0.001, and chest X-ray: 95.8 and 50.0%; P<0.001); however, the histological type of three interval cases in the chest X-ray group was unknown. As for screening rank, specificity for the repeated screenings was significantly higher than that for the initial screenings (low-dose CT: 95.7 vs 91.0%; P<0.001, and chest X-ray: 97.7 vs 95.9%; P<0.001). As for sex, specificity for men was significantly lower than that for women (low-dose CT: 92.1 vs 93.5%; P<0.05, and chest X-ray: 95.7 vs 97.6%; P<0.001). Sensitivity of chest X-ray screening for women was significantly higher than that for men (100 vs 68.2%; P<0.05). As for smoking status, sensitivity of both low-dose CT and chest X-ray for nonsmokers was 100%.
Table 4 shows sensitivity estimated by the incidence method. Until the end of December 2003, a total of 14 434 person-years (total for men: 9173 person-years; total for women: 5512 person-years) for the low-dose CT group and a total of 59 725 person-years (total for men: 17 962 person-years; total for women: 41 763 person-years) for the chest X-ray group had been followed up for. The mean follow-up terms were 3.1 person-years and 4.5 person-years, respectively. The number of expected lung cancer cases was calculated to be 24.4 persons for the low-dose CT group and 59.3 persons for the chest X-ray group. As a result, sensitivity (95% confidence interval) estimated by the incidence method was 79.5% (63.5–95.5%) and 86.5% (77.8–95.2%), respectively. The difference in sensitivity by the incidence method was not statistically significant.
Discussion
The present study is the first report on sensitivity and specificity of annual lung cancer screening using low-dose CT and data from a local Cancer Registry. Sensitivity and specificity of low-dose CT screening according to the detection method were 88.9 and 92.6%. The sensitivity estimated by the incidence method resulted in a value of 79.5%. On the other hand, sensitivity and specificity of chest X-ray in the same time frame by the detection method were 78.3 and 97.0%, respectively. Furthermore, sensitivity of chest X-ray screening by the incidence method was 86.5%.
In previous studies conducted in the1980s, sensitivity and specificity of annual lung cancer screening using chest X-ray and sputum cytology were also evaluated by the detection method. In those studies, sensitivity and specificity for usual screening were 63.6–88.0% and 94.7–99.6%, respectively (Sobue et al, 1991c; Soda et al, 1993; Sagawa et al, 1994b; Tsukada et al, 2002). The use of low-dose CT screening resulted in a higher sensitivity and lower specificity than usual screening. The reported high sensitivity in participants undergoing low-dose CT screening is the result of improvement in the detection of small tumours. The lower specificity value indicates the difficulty of diagnosing nodules detected by screening.
Several points must be considered when the present study results are compared with previous results. Since 1980s, lung cancer incidence by histological type has undergone a change over time. With a large decline in the smoking rate among men, the proportion of squamous cell carcinoma or small cell carcinoma has decreased, whereas the proportion of adenocarcinoma has increased (Yoshimi et al, 2003). The current environment may be more advantageous for lung cancer screening because adenocarcinoma occurring in the peripheral lung has a longer doubling time than squamous cell carcinoma (Arai et al, 1994). In addition, as most low-dose CT screening-detected lung cancer lesions are too small to detect by chest X-ray and have a longer preclinical phase, simple comparison of low-dose CT screening with chest X-ray screening is difficult.
We used the detection method and stratified analyses by screening rank and histological type. As for screening rank, specificity of both low-dose CT and chest X-ray for the repeated screenings was significantly higher than that of the initial screenings. The high specificity associated with repeated screenings is due to the fact that the review of previous images facilitates ruling out benign nodules. Sensitivity of low-dose CT and chest X-ray for the repeated screenings was lower than that of the initial screenings; however, the difference was not statistically significant. Sensitivity for the initial screenings was affected by length bias and overestimation because lung cancers with long preclinical detectable phases were more prevalent. Regarding histological type, adenocarcinoma sensitivity estimated by the detection method was significantly higher than that for nonadenocarcinoma for both low-dose CT and chest X-ray. In the previous study, sensitivity of chest X-ray was 86.4% for adenocarcinoma and 44.2% for nonadenocarcinoma (Sobue et al, 1991c). Both low-dose CT screening and chest X-ray screening have a high sensitivity for the detection of adenocarcinoma. In contrast, sensitivity estimated by the detection method for nonadenocarcinoma remained low. As for smoking status, both low-dose CT and chest X-ray had superior performance for nonsmokers.
Although the detection method is simple and widely used, it is affected by overdiagnosis or length bias because cancers with long preclinical detectable phases are included in the denominator. In the 1980s, lung cancer was considered to be an aggressive and rapid-growing cancer; however, it has been reported that low-dose CT screening-detected lung cancer has a long doubling time and good prognosis (Sone et al, 2001; Nawa et al, 2002; Sobue et al, 2002a; Swensen et al, 2002; Henschke et al, 2006; Libby et al, 2006). The incidence method, which is not affected by overdiagnosis bias and length bias, is preferred for the correct evaluation of low-dose CT screening. Screening for breast cancers or colorectal cancers, with long doubling times, has been evaluated using the incidence method whereas lung cancer screening has been evaluated using the detection method only (Fletcher et al, 1993; Zappa et al, 2001).
In this study, we calculated expected lung cancer incidence to be 24.4 persons for the low-dose CT group and 59.3 persons for the chest X-ray group according to age-specific lung cancer incidence rate in the OCR, smoking status in Osaka prefecture and the relative risk of lung cancer incidence associated with smoking according to a large-scale cohort study in Japan. Unexpectedly, the sensitivity of low-dose CT screening estimated by the incidence method (79.5%) was lower than that of chest X-ray screening (86.5%); however, the difference was not statistically significant. There are several possible explanations for this contradiction. First, the mean follow-up term of the low-dose CT group (3.1 person-years) was shorter than that of the chest X-ray group (4.5 person-years). Furthermore, the mean pack index of current smokers among the low-dose CT group (42 for men and 23 for women) was somewhat higher than that of the chest X-ray group (38 for men and 16 for women). Therefore, expected lung cancer incidence for the low-dose CT group might be underestimated. Second, four screen-detected cases among the chest X-ray group were checked with lesions other than cancer. These lung cancer cases were incidentally detected by the subsequent chest CT as a further examination on positive tests; all of them were adenocarcinoma. When these cases were regarded as interval cases, sensitivity (95% confidence interval) of chest X-ray screening by the incidence method resulted in 79.7% (69.5–90.0%). Considering these points, sensitivity of low-dose CT screening according to the incidence method with 3–5 person-years of follow-up period would be almost equal to that of chest X-ray screening. These findings suggest that the efficacy of low-dose CT screening might be limited to rapid-growing lung cancer with a short preclinical detectable phase (<=1 year). Since low-dose CT screening-detected lung cancer is slow growing, further research with a longer follow-up period is required.
A total of 40 lung cancer cases were detected by low-dose CT screening, suggesting the possibility of overdiagnosis by low-dose CT screening. In particular, low-dose CT screening detected 13 lung cancer cases in nonsmokers whereas expected incidence in nonsmokers was only 1.7 persons. All of these cases were peripheral adenocarcinoma. In contrast, expected lung cancer incidence for the chest X-ray group was higher than the number of screen-detected cases. This fact might suggest that there is little possibility of overdiagnosis by chest X-ray screening.
Of the five interval cancer cases in the low-dose CT group, four cases were squamous cell carcinoma or small cell carcinoma, which are strongly associated with smoking (Sobue et al, 1991d; Shimizu et al, 1994; Stellman et al, 2001). Three cases had remarkable emphysaema. These interval cancer cases associated with smoking indicate the limitation of low-dose CT screening for nonadenocarcinoma among smokers. In other words, the high sensitivity of low-dose CT screening identified using the detection method is due to the detection of adenocarcinoma with a long preclinical detectable phase.
This study has some limitations. First, many nodules were detected by low-dose CT screening, but subsequent pathological examinations were not performed. In this study, small pure ground-glass opacity nodules (<10 mm) were carefully observed, and no invasive treatment was performed. In these cases, lung cancer was highly suspected, but a lung cancer diagnosis was not made and the cases were not registered in the OCR. Given the presence of such cases, the sensitivity according to the detection method might be underestimated. Second, to compare usual screening with low-dose CT screening, the preclinical detectable phase was assumed to be 1 year. We need to assess a longer preclinical detectable phase, because most of the low-dose CT screening-detected lung cancer cases were slow growing. Third, the sample size was relatively small for proper evaluation, particularly for stratified analyses.
In summary, the present findings suggest that lung cancer screening using low-dose CT has a higher sensitivity and a lower specificity than usual lung cancer screening by chest X-ray, when using the detection method analysis. However, sensitivity estimated by the incidence method was not as high as that estimated by detection method. As all interval cancer cases were associated with smoking, low-dose CT screening showed limited efficacy for nonadenocarcinoma in smokers. Furthermore, these findings demonstrate the potential for overdiagnosis in low-dose CT screening-detected cases.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arai T, Kuroishi T, Saito Y, Kurita Y, Naruke T, Kaneko M, The Japanese lung cancer research group (1994) Tumor doubling time and prognosis in lung cancer: evaluation from chest films and clinical follow-up study. Jpn J Clin Oncol 24: 199–204
Day NE (1985) Estimating the sensitivity of a screening test. J Epidemiol Community Health 39: 364–366
Department of public health, Osaka Prefecture (2006) Smoking, Kenko Osaka 21 Report, pp 26–64. Osaka Prefecture: Osaka
Diederich S, Thomas M, Semik M, Lenzen H, Roos N, Weber A, Heindel W, Wormanns D (2004) Screening for early lung cancer with low-dose spiral computed tomography: results of annual follow-up examinations in asymptomatic smokers. Eur Radiol 14: 691–702
Fletcher SW, Black W, Harris R, Rimer BK, Shapiro S (1993) Report of the international workshop on screening for breast cancer. J Natl Cancer Inst 85: 1644–1656
Fontana RS, Sanderson DR, Woolner LB, Taylor WF, Miller WE, Muhm JR (1986) Lung cancer screening: the Mayo Program. J Occup Med 28: 746–750
Henschke CI, Naidich DP, Yankelevitz DF, McGuinness G, McCauley DI, Smith JP, Libby D, Pasmantier M, Koizumi J, Flieder D, Altorki N, Miettinen OS (2001) Early lung cancer action project: initial findings on repeat screenings. Cancer 92: 153–159
Henschke CI, Yankelevitz DF, Libby DM, Pasmantier MW, Smith JP, Miettinen OS (2006) Survival of patients with Stage I lung cancer detected on CT screening. New Eng J Med 355: 1763–1772
Jett JR (2005) Limitation of screening for lung cancer with low-dose spiral computed tomography. Clin Cancer Res 11: 4988–4992
Libby DM, Wu N, Lee IJ, Faroogi A, Smith JP, Pasmantier MW, MacCauley D, Yankelevitz DF, Henschke CI (2006) CT screening for lung cancer: the value of short-term CT follow up. Chest 129: 1039–1042
Marcus PM, Bergstralh EJ, Fagerstrom RM, Williams DE, Fontana R, Taylor WF, Prorok PC (2000a) Lung cancer mortality in Mayo Lung Project: impact of extended follow-up. J Natl Cancer Inst 92: 1308–1316
Marcus PM, Bergstralh EJ, Zweig MH, Harris A, Offord KP, Fontana RS (2006b) Extended lung cancer incidence follow-up in the Mayo Lung Projects and overdiagnosis. J Nat Cancer Inst 98: 748–756
Nawa T, Nakagawa T, Kusano S, Kawasaki Y, Sugawara Y, Nakata H (2002) Lung cancer screening using low-dose spiral CT: results of baseline and 1-year follow up studies. Chest 122: 15–20
Sagawa M, Nakayama T, Tsukada H, Nshii K, Baba T, Kurita Y, Saito Y, Kaneko M, Sakuma T, Suzuki T, Fujimura S (2003a) The efficacy of lung cancer screening conducted in 1990s: four case–control studies in Japan. Lung Cancer 41: 29–36
Sagawa M, Saito Y, Takahashi S, Endo C, Usuda K, Kamma K, Sato M, Ohkuda K, Sato H, Fujimura S (1994b) Sensitivity and specificity of lung cancer screening with sputum cytology and chest X-ray film in high risk group. Haigan 34: 1–5 (in Japanese)
Shimizu H, Nagata C, Tsuchiya E, Nakagawa K, Weng SY (1994) Risk of lung cancer among cigarette smokers in relation to tumor location. Jpn J Cancer Res 85: 1196–1199
Sobue T, Moriyama N, Kaneko M, Kusumoto M, Kobayashi T, Tsuchiya R, Kakimura R, Ohmatsu H, Nagai K, Nishiyama H, Matsui E, Eguchi K (2002a) Screening for lung cancer with low-dose helical computed tomography: anti-lung cancer project. J Clin Oncol 20: 911–920
Sobue T, Suzuki T, Fujimoto I, Matsuda M, Doi O, Mori T, Furuse K, Fukuoka M, Yasumitsu T, Kuwahara O, Ichitani M, Taki T, Kuwabara M, Nakahara K, Endo S, Sawamura K, Kurata M, Hattori S (1991d) Lung cancer risk among ex-smokers. Jpn J Cancer Res 82: 273–279
Sobue T, Suzuki T, Matsuda M, Horai T, Kajita A, Kuriyama K, Fukuoka M, Kusunoki Y, Kikui M, Ryu S, Fujimoto I (1991c) Sensitivity and specificity of lung cancer screening in Osaka, Japan. Jpn J Cancer Res 82: 1069–1076
Sobue T, Yamamoto S, Hara M, Sasaduki S, Sasaki S, Tsugane S (2002b) Cigarette smoking and subsequent risk of lung cancer by histologic type in middle-aged Japanese men and women: the JPHC study. Int J Cancer 99: 245–251
Soda H, Tomita H, Kohno S, Oka M (1993) Limitation of annual screening chest radiography for the diagnosis of lung cancer. Cancer 72: 2341–2346
Sone S, Li F, Yang ZG, Honda T, Maruyama Y, Takashima S, Hasegawa M, Kawakami S, Kubo K, Haniuda M, Yamanda T (2001) Results of three-year mass screening programme for lung cancer using mobile low-dose spiral computed tomography scanner. Br J Cancer 84: 25–32
Stellman SD, Takezaki T, Wang L, Chen Y, Citron ML, Djordjevic MV, Harlap S, Muscat JE, Neugut AI, Wynder EL, Ogawa H, Tajima K, Aoki K (2001) Smoking and lung cancer risk in American and Japanese men: An international case–control study. Cancer Epidemiol Biomarkers Prev 10: 1193–1199
Swensen SJ, Jett JR, Sloan JA, Midthun DE, Hartman TE, Slykes AM, Aughenbaugh GL, Zink FE, Hillman SL, Noetzel GR, Marks RS, Clayton AC, Pairolero PC (2002) Screening for lung cancer with low-dose spiral computed tomography. Am J Respir Crit Care Med 165: 508–513
Tsukada H, Yokoyama A, Kurita Y, Misawa H (2002) Evaluation of population based lung cancer screening in Niigata and analysis of interval cases based on comparison lung cancer registry with screening records. Nihon Kokyuki Gakkai Zasshi 38: 501–508 (in Japanese)
Yoshimi I, Ohshima A, Ajiki W, Tsukuma H, Sobue T (2003) A comparison of trends in the incidence rate of lung cancer by histological type in the Osaka Cancer Registry, Japan and in the Surveillance, Epidemiology and Ends Results Program, USA. Jpn J Clin Oncol 33 (2): 98–104
Zappa M, Castuglione G, Paci E, Grazzini G, Rubeca T, Turco P, Crocetti E, Ciatto S (2001) Measuring interval cancers in population-based screening using different assays of fecal occult blood testing: the district of Florence experience. Int J Cancer 92: 151–154
Acknowledgements
This study was supported by a grant-in-aid from the Ministry of Health, Labor and Welfare of Japan for a Third term Comprehensive Control Research for Cancer (Grant no. 19141901). We would like to thank the staff of the Division of Epidemiology and the Osaka Cancer Registry, Department of Cancer Control and Statistics, Osaka Medical Center for Cancer and Cardiovascular Disease.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Toyoda, Y., Nakayama, T., Kusunoki, Y. et al. Sensitivity and specificity of lung cancer screening using chest low-dose computed tomography. Br J Cancer 98, 1602–1607 (2008). https://doi.org/10.1038/sj.bjc.6604351
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604351
Keywords
This article is cited by
-
The added value of using artificial intelligence in adult chest X-rays for nodules and masses detection in daily radiology practice
Egyptian Journal of Radiology and Nuclear Medicine (2023)
-
Tumor-educated platelet blood tests for Non-Small Cell Lung Cancer detection and management
Scientific Reports (2023)
-
AI-based improvement in lung cancer detection on chest radiographs: results of a multi-reader study in NLST dataset
European Radiology (2021)
-
Fluorescent paper strip immunoassay with carbon nanodots@silica for determination of human serum amyloid A1
Microchimica Acta (2021)
-
Chest X-ray in suspected lung cancer is harmful
European Radiology (2021)